Introduction to the Study
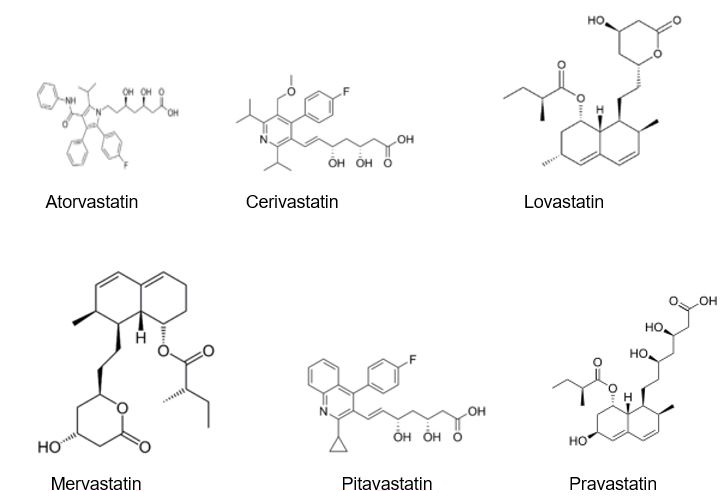
Statin medication is also known as HMG-CoA reductase inhibitors, are drugs that are used to reduce the levels of cholesterol within the human body by limiting the cholesterol production activities of the HMG-CoA reductase enzymes. Statins are also used to lower the low-density lipoprotein (LDL) cholesterol levels within the body. Apart from lowering the cholesterol levels in the body, statin drugs are also used to raise the high-density lipoprotein (HDL) cholesterol levels in the body to ensure that there is a balanced level of cholesterol. LDL is referred to as bad cholesterol in the body as it affects the functions of major organs such as the liver and the heart while HDL is known as good cholesterol. Examples of statins used to lower the low-density lipoprotein cholesterol include atorvastatin, lovastatin, and pravastatin (Sweetman 2009).
Statin medications have proved to be useful in reducing cardiovascular disorders as well as heart strokes and liver failure. They lower the LDL or bad cholesterol levels within the body by 1.8mmol/l or 70mg/dl which generally translates to a reduction of 60% of heart attack or cardiac arrest cases reported every year. Statins have been identified as the most suitable drugs that can be used in lowering the mortality rates of people that suffer from cardiovascular disorders. They are also used in patients that have a high predisposition to heart diseases or coronary disorders (Law et al 2003). Statin medications are useful when it comes to dealing with people that have a high LDL cholesterol level in their bodies. High low-density lipoprotein levels have been identified by many medical practitioners to be the major cause of coronary artery disease (CAD) which leads to the hardening of the body’s arteries over a significant period of time. By lowering the high low-density lipoprotein cholesterol levels, statins help to reduce the risk of developing heart diseases and coronary disorders. They are also useful in reducing the risks of heart attacks as well as stroke-related deaths in people that are suffering from coronary artery diseases (O’Connor et al 2005).
Statins were first developed in 1971 by a Japanese biochemist known as Akira Endo while conducting research to determine what drugs could be used to lower cholesterol levels within the human body. Endo created the statin drug based on research information that existed on the HMG-CoA reductase enzyme within the body’s liver. The biochemist reasoned that certain microorganisms could be released by the reductase enzyme to reduce the levels of cholesterol within the body. Some of these microorganisms included mevastatin which is a molecule that is produced by Penicillium citrinum and mevalonate which is necessary for the maintenance of cell walls and cytoskeleton tissues within the human body. Endo’s research enabled him to create statins based on the HMG-CoA enzyme to reduce fat within the body (Endo 1992)
Like other forms of medication, statin drugs have various side effects that might prove harmful to the users of the medication. Some of the most common side effects of statins include muscle problems or muscle cramps, cognitive loss, sexual dysfunction, gastrointestinal problems, neuropathy, and raised levels of liver enzyme production. Despite its effectiveness in reducing cholesterol levels within the body, statin medication poses these effects to people who are under statin medication. Unfortunately, very few patients are aware of the danger that is posed by consuming statin medication. Although all statin drugs contain labels that warn patients of the adverse effects of the medication, the labels have been viewed by many medical practitioners to be inadequate and inconsistent since the warnings are written in very small print that is at times illegible (Steinberg 2007).
Every patient that has a prescription for statin medication should be made aware of the risks posed by taking these drugs. Patients need to be informed by their physicians of these adverse side effects posed by statins before they begin taking the drugs. Patients should be advised by their doctors to follow the instructions in the medication to the letter to ensure that they do not suffer the adverse effects of the medication. Statin medication should be administered to patients with not just proper information but also regular supervision to ensure that the patients use the medication in the right way (Golomb et al 2008).
By properly adhering to the administration of the drugs, patients might be able to reduce the effects posed by statins when it comes to increasing liver enzyme production within the body as well as myositis and myopathy which increase the potential of the patient developing rhabdomyolysis, a condition that leads to the breakdown of skeletal muscle tissues. Providing patients with the relevant information will ensure that they use the statin medication in the right way to reduce any adverse side effects that are caused by statins. Doctors, therefore, have the important task of ensuring that there is effective communication when it comes to the use of statin medication with their patients when discussing their treatment plans (NCCPC 2010).
Background of the Study
The purpose of conducting this study is to determine the role of patient behavior and information in the adherence to a statin medication. Medication adherence is an important subject especially when it comes to the adherence to drugs that have adverse side effects like statin medications. Patient behavior is the action of the patient when it comes to adhering or conforming to medication or drugs prescribed by physicians. The adherence to statin medication is an important topic for all healthcare providers as these medications have many side effects that might prove to be detrimental to patients. While cholesterol is important in the body, it needs to be maintained at a certain level to ensure that it does not pose any health problems to the patient. High cholesterol levels contribute to the development of atherosclerosis within the body where cholesterol-containing plaques begin to develop within the body’s major arteries (Silva et al 2006).
Uses of Statin Treatments
The condition of atherosclerosis or plaque formation blocks the flow of blood in the body’s major arteries, reducing blood circulation which in turn affects the development of body tissues that are vital in the proper functioning of the body. When the plaques rupture or become damaged, they lead to the formation of blood clots which block the flow of blood within the body’s arteries. Reduced levels of blood flow cause heart attacks, chest pains, coronary artery disorders, heart strokes, and other conditions such as claudication which occurs in the legs. Statins are designed to reduce the levels of LDL cholesterol within the body which in turn reduces the formation of plaques and blood clots in the body’s arteries. Statins are also able to stabilize the plaques that exist in arteries by preventing them from rupturing and also reducing the occurrence of blood clots (Klein et al 2006).
Apart from treating blood clots and plaques that form in arteries, statins are also used in the treatment of atherosclerosis which is a complex condition that leads to the inflammation of the arterial walls as a result of high cholesterol levels within the body. Statins reduced the levels of inflammation within the body’s arteries reducing the chances of a person developing atherosclerosis (Sasmaz and Korkmaz 2004). Statins also reduce the chances of a patient acquiring chest pains, heart strokes, and claudication which arises as a result of atherosclerosis within the body. 35% of individuals who suffer from heart problems do not usually suffer from high blood cholesterol levels. Some of their heart problems are therefore attributed to the presence of atherosclerosis within their body (Nissen et al 2006).
Adherence to Medication
Adherence is a commonly used term in the medical prescription of drugs as it means that the patient will comply with the doctor’s directions in taking the medication as well as follow the drug usage instructions. Adherence to medication is generally used to refer to the observance and conformity of drug usage but it might also be used to refer to the attendance of counseling sessions, the undertaking of self-directed physiotherapy exercises, and the taking care of a chronic wound or illness (Kedward and Dakin 2003).
In the determination of the rates of adherence, the aspects that are usually considered include the percentage of the prescribed doses and the specified period of time that the patient is meant to complete the dosage. Medical practitioners have further expounded on the definition of adherence to refer to the information that relates to dose taking of a prescribed number of pills in one day. Medical research has shown that the adherence rate to medication is higher in patients that are suffering from acute conditions such as AIDS or HIV. While patients that suffer from acute conditions like HIV have a high level of medication adherence, patients that suffer from chronic conditions such as diabetes or asthma demonstrate a low adherence to medication (Osterberg and Blaschke 2005). According to a study conducted by Benner et al (2002), the number of patients who discontinued their intake of hydroxymethylglutaryl-coenzyme during the first three to six months of their medication was approximately half which demonstrated that chronic patients tended to have low medication adherence when compared to acute condition patients.
With regards to statin medication, many patients have been noted to stop taking their medication in less than six months after the statin medications have been prescribed. According to clinical trials, the discontinuation of statin medications was calculated to be 6% to 30% where patients stopped adhering to their medication within the first few months of treatment. In the US, 50% of the patients discontinued their medication during the first six months of their treatment while 30% to 40% discontinued their treatment during the first one year of their treatment. This poor adherence to statin medication has mostly been attributed to economic factors, social considerations, and psychological factors (Natarajan 2007).
Long Term Effects of Statin Medication
While the Federal Drug Association (FDA) has certified statins to be safe drugs in reducing cholesterol levels within the body, they have several adverse effects that affect individuals who have been taking the drugs for a prolonged period of time. The most common effects of statin medication are muscle cramps and muscle pain which might become potentially dangerous with the continued use of statin medication as muscle pain limits the ability of the patient to conduct basic functions such as walking, lifting of heaving objects, and lifting of the hands. Muscle pain also leads to rhabdomyolysis, a condition that breaks down the muscles within the body leading to muscle weakness and pain (Schneeweiss et al 2007).
Another long-term effect of statin medication is neuropathy which is a condition that leads to the malfunction of the peripheral nervous system that mainly controls the breathing functions of the heart. Neuropathy is also caused by the presence of poisonous chemicals within the body for a long duration of time. The prolonged use of statin medication by patients has been seen by most medical researchers to interfere with the normal functions of the body’s nervous system, making it hard for patients to breathe. Medical researchers and scientists have also noted that the build-up of satins within the body contributes to the development of neuropathy within the body (Blackburn et al 2005).
Apart from causing breathing problems, neuropathy which has been caused by the prolonged use of statin medications leads to muscle weakness which is a major sign of neuropathy. Patients who are under statin medication might not recognize this muscle weakness to be a symptom of neuropathy and they might confuse it with tiredness and aging. Apart from muscle weakness, other signs and symptoms of neuropathy include burning pains in the muscle joints, numbness in the hands and legs, pricking sensations in the hands, legs, and toes, and increased sensitivity to touch (Caspart et al 2005).
Another long-term effect of neuropathy is memory loss which occurs in patients that have taken statin medications for a period of two years. Statins create an inability to concentrate well in patients and they also speed up the development of Alzheimer’s disease in patients that have been taking the statin medication for a long period of time. The memory loss is at times usually so severe that it lasts for between 6 to 12 hours in patients that are under statin medication. This memory loss might at times become severe to the point the patient suffers from amnesia and delirium (Wright and Abrahamson 2007). A review of the cases analyzed by the FDA showed that half of the patients on statins experienced some form of memory loss within the first 60 days of statin treatment. The review showed that patients who discontinued usage of the statin medication were able to revert to normal and the cases of memory loss were reduced considerably. Apart from memory loss, studies have also shown that patients experience mood swings and behavioral changes as a result of the continued use of statin medication (Perreault et al 2005).
Statin Intoxication
In terms of statin intoxication, various research studies have identified that several statin medications lead to conditions such as myopathies, renal failure, and rhabdomyolysis. Studies conducted have shown that there are adverse manifestations of statin intoxication with the use of various statin medications such as lovastatin, fluvastatin, and atorvastatin. When patients use a combination of these drugs to reduce cholesterol levels in their bodies, they are more than likely to develop liver failure as well as an elevation of transaminase enzymes within the body. The continued use of different statin medications also increases the chances of a person developing hyperlipidemia which in turn increases the chances of a person developing transaminase within their body. Statin intoxication or the use of several types of statin medications at once increases the incidence of a person developing eye cataracts, neoplasia and psychiatric problems (Chiang et al 2004). The diagrams below demonstrate the different types of statin medications that are used to control cholesterol levels in patients that suffer from coronary heart disorders and heart problems.
Effects of Proper Communication
Effective communication between the physician and the patient is a major contributing factor in the patient’s adherence to medication and treatment plans. The presence of effective communication between the healthcare provider and the patient will greatly affect the adherence of the patient to their medication (Campione et al 2005). The inability of doctors to issue clear communication treatment plans might contribute greatly to the patient’s non-adherence to the prescribed medication. Previous research and studies have shown that poor communication by the doctor contributes to the low rates of medication adherence. One such study was conducted to investigate the level of doctor and patient communication when it came to patient adherence to medication (Anderson et al 2005).
The results of the study showed that 47% of the patients receiving at least one type of medication declined to ask their doctors any questions about their prescriptions. The patients failed to ask their doctors about the type of medication they were taking and also whether the medication had any adverse effects on their health. The study also revealed that doctors failed to explain the prescriptions properly to their patients which demonstrated that there was poor communication when it came to patient prescription medication. This ineffective communication led to the patients discontinuing their medication because of poor instruction as well as side effects caused by the medication (Nakamura et al 2006). The study demonstrated that a lack of proper communication contributed greatly to low adherence rates to patient medication.
Effective communication ensures that patients are able to communicate their fears and feelings towards taking medication that might seem harmful to their health. Patients are able to communicate their experiences with prescription drugs and medication if there is effective communication between the doctor and the patient. While there have not been many studies conducted to determine whether effective communication affects patient adherence to medication, patients who receive minimal or no communication about their treatment regimes are more than likely to discontinue their treatment once they start experiencing adverse side effects. It, therefore, becomes imperative for doctors to maintain effective communication with their patients in terms of their treatment plans and medication (Higgins et al 2003).
Effective communication in the pharmacy is also important when patients are purchasing statin medication. Pharmacy policies are an important step in modulating the adherence behavior of patients as they are meant to ensure that patients understand how they are going to take their prescriptions to reduce the risk of heart problems. It is therefore important for pharmacists to maintain an effective communication link with their customers to ensure that they understand the importance of completing their statin prescriptions (Deddens and Petersen 2004). Effective communication by doctors and health care providers will therefore entail providing patients with the necessary medication and treatment for their illness as well as providing them with the necessary instructions on how to use this medication (Brookhart et al 2007).
Effective communication will also involve recommending the minimum amount of medication that a patient can take for their illness as well as making the dosage for medication more simple by creating a schedule that will enable the patient to determine when they should take their prescriptions. During the treatment process, doctors are expected to continually observe the progress of their patients as they go through the treatment to see whether they are taking the medication as prescribed and to determine whether any side effects arise from consuming the prescriptions. Communication will also involve the doctors providing some recommendations that will be used by the patients in dealing with the side effects of the drugs in the event they occur (Brookhart et al 2007).
Aims and Purpose of the Research
The purpose of conducting this research will be to determine the adherence rates of patients to a statin medication. This will involve determining the various factors that come into play when patients are under statin forms of medication and how these factors affect their adherence rates. The aim of conducting this research will be to determine what type of patient characteristics or behavior are usually involved when adhering to statin medication and what role these characteristics play in the dosage intake. Another aim of the study will be to determine why patients do not conform to doctors’ instructions when they are taking their medication. The research questions that will be answered in the discussion will involve:
- What patient characteristics are used in the adherence to statin medication and how do these characteristics affect the treatment of cholesterol levels in patients that suffer from heart strokes and cardiovascular conditions?
- How much information is given to patients by healthcare providers such as doctors, physicians, and pharmacists when it comes to statin treatments?
- Is there effective communication between doctors and their patients on the adverse effects that are caused by statin medications when they are discussing their treatment plans?
Literature Review
Patient adherence to Statin Medication
Patient adherence to medication is important especially when it comes to treating acute conditions such as coronary artery disorders, heart problems, and liver failure. Heart attacks, liver, and kidney failures have been identified to be the major causes of morbidity and mortality around the world. As discussed earlier, the major causes of these problems have been identified to be high levels of low-density lipoprotein (LDL) cholesterol levels within the body as well as high cholesterol levels within the body. Statins have been identified by most medical practitioners to be the most effective drugs in reducing the levels of cholesterol within the body. Statins are therefore the preferred drug of choice for patients who are suffering from high levels of cholesterol (Wei et al 2002).
In the general adherence to medication, the therapeutic effects of a drug usually depend on the ability of a patient to comply with the treatment plan that comes with the medication. Many doctors and physicians around the world provide their patients with medication instructions and treatment plans that they can use when taking their medication. These doctors expect their patients to follow these instructions to the letter to ensure that the drugs are effective in treating their patients. However, most patients fail to adhere to the treatment plans prescribed by their doctors which make the drug to be ineffective. Studies conducted in the recent past with relation to adherence to statin medication have shown that there is a low rate of drug adherence amongst patients who are under statin treatment (Benner et al 2005).
The effects of failing to complete statin treatments might lead to the return of heart problems and coronary heart problems which the statin treatment was meant to reduce. Patient behavior, therefore, plays an important role when it comes to adherence to statin medication. Patient behavior is usually determined by various factors such as the patient’s understanding of the doctor’s instructions and their understanding of the prescription information. Patient behavior is also determined by their belief that the statin medication will reduce heart problems as well as their lifestyle choices such as regular exercising and a balanced healthy diet (Higgens et al 2003).
Studies on Patient Adherence to Statin Medication
A lot of studies have been conducted on the role of patient behavior concerning adherence to a statin medication. One of these studies was conducted by Huser et al (2005) to assess the role of behavior in adherence to a statin medication. The studies revealed that despite well-publicized guidelines on effective statin therapy, many patients did not finish their treatments which in the end exposed them to higher risks of cardiac events. The results of the study revealed that the adherence rates decreased from 56% to 35% in the first 9 months as the patients decreased their usage of statin medication. Another study was conducted to determine the impact of prescription size on the rate of adherence in statin treatments.
Batal et al (2007) conducted a study to determine whether the amount of prescription affected the adherence of patients to a statin medication. The researchers analyzed 3,386 patients who were under different types of statin medication in an inner-city healthcare system. The factors that were considered in the study included the age of the patients, their gender, race, and insurance status to determine whether any of these factors affected their adherence to a statin medication. The results of the study showed that 47.5% of the patients were adherent to their statin treatments when compared to 52.5% who were non-adherence to their statin medications. The univariate analysis of the results demonstrated that the insurance status of the patients as well as their obligation to co-pay did not have any correlation with their adherence to a statin medication. The table below represents patient characteristics and the adherence to statin medication (Batal et al 2007).
(Source: Batal et al 2007)
The results of the study also showed that patients who had a larger prescription of statin medications had a greater adherence rate when compared to those who had a lower prescription of statin medication. Patients who had a 30-day fill to a 60-day fill had a higher adherence rate as they had more prescriptions to finish. The study revealed that the major reason for non-adherence to statin medication was because of forgetfulness to take the medication and if the patient has a 30 to 60-day fill, they might be able to have higher adherence to the statin medication (Osterberg and Blaschke 2005). The results also showed that patients who had insurance coverage were able to record a greater adherence to a medication when compared to those that did not have any insurance coverage. This was because the cost of statin medication and prescriptions was lower for those that had insurance coverage (Batal et al 2007).
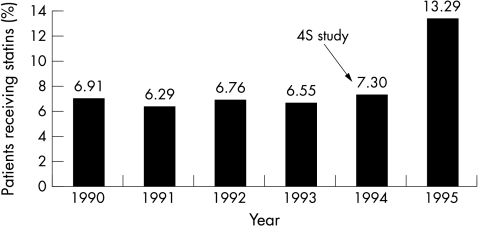
Various studies have been conducted on the role of patient behavior when it comes to patient adherence to a statin medication. One of these studies was conducted by Wei et al (2002) to investigate the adherence to statin treatments by patients who had suffered myocardial infarctions and to determine the effects of drug adherence to the recurrence of myocardial infarctions as well mortality and morbidity rates. The study was conducted in Tayside which is found in Scotland, the UK through the use of medical databases that contained information of patients that had suffered from myocardial infarctions between 1985 and 1995. The total number of patients who were examined under the controlled clinical trial totaled 5,590 patients who had experienced their first MI complication between the identified periods (Wei et al 2002).
The results of the study showed that 13% of the 5590 patients had experienced at least one MI between January 1990 and November 1995 while 23% of the patients had died during the following period of the study. Only 7% of the patients who had received statin medication for their myocardial infarctions had experienced a full recovery of their heart condition. There was a significant increase in statin medications after the first results first of the study were published in 1994. The published studies showed that patients who were undergoing statin treatment had an 80% adherence to their medication. The diagram below demonstrates the characteristics of patients that have recurrent myocardial infarctions and those that do not have any Myocardial infarctions recurrences (Wei et al 2002).
The results of a study conducted by Rifkin et al (2010) indicated that older patients were less than likely to be prescribed statin medication when compared to younger patients. The results of the study also demonstrated that women of all ages had higher adherence to statin medication when compared to men of the same age. Patients that lived in deprived areas recorded the highest level of statin medication adherence when compared to patients that lived in moderately deprived areas. The researchers based their analysis of the adherence to statin medication by patients on their gender, their age, deprivation category, and death status (Rifkin et al 2010).
Another study was conducted by Natarajan et al (2007) to determine the adherence that patients had in taking statin medication in Halifax. Information for the study was obtained from a self-report survey that was sent to a hospital-based practice and a community-based hospital. 400 patients who were under statin medication and were 40 years or older were identified for the study within the population and the self-report survey was sent to these 400 patients and their families to determine their adherence to a statin medication. The survey incorporated the use of a patient self-report survey that would measure the adherence of patients to statin medications. 330 out of the 400 patients that had been identified for the survey returned the self-report, the results of which showed that 18 out of the 330 patients had discontinued their statin medication. The results also showed that 17 out of the 330 patients were using non-statin medications to lower their cholesterol levels were. 63% of the patients were identified to be highly adherent to their statin medications while 37% were either non-adherent or moderately adherent to their statin treatment plans (Natarajan et al 2007).
The reasons proposed by Shroufi and Powles (2010) for the high adherence rate by patients undertaking statin medication were mostly attributed to the insurance coverage that most of the patients in the study had. Other factors that contributed to the high levels of adherence to statin medication were the age of the patients where people older than 65 years were more than likely to record a high adherence to statin medication than people who were between the ages of 40 and 55. Patients who were taking more than 4 to 6 types of statin medications had higher adherence than those who had between 2 to 4 types of statin medications (Shroufi and Powles 2010).
In terms of behavior, the study highlighted that patients who maintained a lifestyle of regular exercise and a healthy balanced diet were able to record high adherence to statin medications when compared to those patients who had a poor or unbalanced diet. The beliefs of the patient’s also played an important part in their statin medication adherence rates were in the study, patients who believed that statins reduced their risk of developing heart attacks recorded a high adherence rate when compared to those who did not believe that statin medication reduced their heart problems (Jackevicius and Mamdani 2002).
Research Methods
As identified in the introduction part of this research, the main aims of conducting this study are to determine the role of patient behavior in the adherence to statin medication and how this behavior affects the treatment of patients that suffer from heart problems and other cardiovascular disorders. The study also aims to determine whether there is any effective communication between doctors and their patients when it comes to statin medication and also if patients adhere to their statin medication.
Methodology
The type of research approach that will be incorporated to meet the above aims of the research will be a randomized control trial where a sample of the population that is under statin medication will be selected. 164 short-term patients who are under statin therapy will be placed in randomized controlled trials of five statin medications which include atorvastatin, fluvastatin, simvastatin, lovastatin, and pravastatin. A meta-analysis of these patients will be used to determine the rates of adherence in patients that are under statin therapy for a duration of five months by assessing the number of prescriptions they are taking, their age, gender, insurance coverage, health and lifestyle choices (whether they have a balanced diet or not).
Study Population, Study Period, and outcome
The study population for this research will be from Tayside which is a small town in Scotland and the patients that will be under study are those who have been under statin medication. The study period will be conducted in five months to ascertain the adherence rates of patients to statin medication with the follow-up period being five months to determine whether the patients are still adhering to their medication. The outcomes of the study will be to identify the role of patient behavior and patient characteristics in the adherence to a statin medication. Patient behavior and characteristics will be measured by age, gender, socioeconomic status, and deprivation category. The adherence to statin medication will be calculated as the number of days when the statin supply was divided by the total number of days the first prescription was dispensed to the patient (Wei et al 2002).
Statistical Analysis of Data
The data will be summarised as standard deviation (SD) for continuous variables and the percentage (%) for the number of subjects within the study. T-tests will be performed to determine the significant differences that exist in adherence to statin medication as well as patient behavior in the intake of statin medication. Multivariate and univariate analyses of the data will be carried out to determine the effects of age, gender, number of statin prescriptions, socioeconomic status, and the patient’s deprivation on the adherence to a statin medication.
Results of the Study
The number of patients who were under the randomized controlled trial was 164 in number. These patients were either taking atorvastatin, fluvastatin, simvastatin, lovastatin, pravastatin, or a combination of either type of statin medication. Their adherence to the medication was assessed with regards to their age, gender, number of prescriptions, their socio-economic status, deprivation category, and death status. The table below demonstrates the results of the randomized control trial for patients under the various statin medications as well as the duration of the study.
The table below demonstrates the adherence to statin use by analysing the age, sex, socioeconomic deprivation and death status of the patients under the controlled study. The table shows that women have a better adherence to statin treatment when compared to men but there was no difference in statin prescriptions in both sexes. Generally patients that lived in more deprived areas had a higher adherence to statin medication when compared to patients from the least deprived areas. There was also a significant trend between statin use and the deprivation of the patients in the study despite the fact that there was no correlation between statin adherence and deprivation.
The table below represents the univariate and multivariate analysis of the results of the study in determining the adherence rates of patients to statin medication. 80% of statin adherence was mostly associated with a lower risk of developing heart problems such as myocardial infarctions and coronary hear disorders in the multivariate analysis.
Discussion
The randomized control trial results showed that people with a high number of statin prescriptions had a greater adherence rate to their medication when compared to people with fewer statin prescriptions. This meant that the higher the number of prescriptions that a patient had, the greater the chances of them adhering to their statin medication. The poor adherence to statin medication in the study was used to explain the poor outcome of patients that suffered from coronary heart disorders as well as other heart problems. Patients who did not complete their statin medication were at a higher risk of developing heart problems when compared to those who were still taking their statin medication. The adherence goal of 80% that was used in the control trial to determine the adherence to statin therapy in the patients placed under the study was important as it ensured the safety and efficacy of the study. The adherence goal also ensured that the proper measurement of statin adherence was achieved within a controlled trial environment (Yilmaz et al 2004).
The meta-analysis demonstrated that the various statin prescriptions lowered the risks of developing heart problems and coronary disorders. Patients who adhered to any or all of the statin prescriptions were able to reduce their chances of developing heart problems while those who discontinued their medication increased their chances of developing heart complications. The meta-analysis also demonstrated that statin prescriptions that were of a higher dosage reduced the LDL cholesterol levels in the patients. The overall risk of developing a stroke was estimated to be 0.90 when a 1.0mmol/l reduction in LDL cholesterol was reduced through the use of various statin medications and treatments. Simvastatin prescriptions of 40mg per day as well as lovastatin and atorvastatin prescriptions of 10mg per day taken by the patients were able to lower their low-density lipoprotein cholesterol levels to 37% during the randomized control trial. Such interventions were able to reduce the chances of developing ischaemic heart disease problems that arise in people who are 65 years and older. Such statin prescriptions were also able to reduce the risk of the patients to heart strokes and heart problems by a percentage of 17%.
The results of the study demonstrated that patients who were over 65 years had greater adherence to statin medication when compared to patients who were under the age of 65 years who registered a lower adherence to a statin medication. This demonstrated that patients who were older tended to follow their statin prescriptions when compared to those who were younger. The results also demonstrated that women had a higher adherence rate to statin medication when compared to men despite the fact that statin medication was not frequently prescribed to women. This is based on studies and research work that has demonstrated that men are more than likely to suffer from heart problems and heart attacks when compared to women (Munger et al 2007).
The results of the study also showed that people from the more deprived areas had a higher adherence rate than the people from the less deprived areas. This high adherence rate was mostly attributed to the high costs of medication as well as treatment for heart problems. The use of the socioeconomic deprivation aspect in the study was necessary to determine the adherence rates of patients who came from different economic backgrounds. The study revealed that proper adherence to statin medication leads to lower risks of heart problems such as myocardial infarctions, coronary heart disease, coronary heart disorders, and heart problems. The daily dose of statin medication and other risk factors demonstrated that patients with a >80% adherence to statin therapy had a lower risk of developing heart problems. With regards to the various types of statin medications, they all had the ability to lower the low-density lipoprotein levels of cholesterol within the patients placed within the study. The absolute reductions which were measured in mmol/l were greater in patients that had had a higher pre-treatment concentration during the clinical trial. In the randomized control trials, patients demonstrated a higher adherence rate to statin medications that had fewer adverse effects on their health.
The study also assessed the number of deaths that had been caused by discontinuing statin medications during the clinical trial. The results of the trial showed that patients who had discontinued their statin medications developed heart problems such as heart attacks, strokes, and cardiac arrests which were so severe that they eventually lead to death (SD=65.3). Patients who adhered to their statin medication reduced their chances of developing heart problems and they were also able to reduce their low-density lipoprotein cholesterol levels within their body which eventually reduced their risk of heart problems.
When compared to studies conducted by Wei et al (2002) and Batal et al (2007), the adherence to statin medication in this study mostly depended on patient characteristics such as age or gender and also the number of prescriptions that the patient has which determined whether the patient would adhere to the medication. Many of the studies analyzed in the research showed that people who were in the 65 and over age bracket had higher adherence to statin medication when compared to people who were in the 60 and below age bracket. Other studies (Wei et al 2002) have also identified the gender of the patients to be a major determinant to statin medication adherence. Women had greater adherence to statin medication when compared to men which can mostly be attributed to their adherence to other forms of medication and their dieting and healthy lifestyles.
Men on the other hand had a lower adherence rate to statin medication which demonstrated that they were not committed to prescriptions and treatment regimes. Previous studies conducted to determine whether the number of prescriptions affected the adherence to statin medication (Batal et al 2007) showed that patients who had more than one statin prescription were more than likely to have higher adherence to their medication when compared to patients who had only one statin prescription. This showed that the higher the number of prescriptions that a patient had, the greater their chances of adhering to their statin medication.
Effect of Communication and Information on Adherence to Statin Medication
Nimalasuriya and Antwerp (2010) conducted a study to determine the effect of communication on the adherence to statin medication in patients suffering from heart conditions, peripheral arterial disease, and coronary heart diseases. Their study focused on determining the barriers to statin adherence as well as determining what communication techniques could be used to increase statin adherence in heart patients. The study also focused on how to improve communication between doctors and their patients to ensure that there was a higher rate of statin adherence. The researchers also assessed the impact of interactive voice response (IVR) technology in breaking the barriers of communication that existed between patients and their doctors. IVR technology involves using personalized communication to deliver treatment plans to patients (Nimalasuriya and Antwerp 2010).
The researchers utilized an experimental design to determine the effect of IVR communication technology on the adherence to statin medication on a target population of 850 patients. Patients who were receiving statin treatment in the Riverside Medical Centre in southern California were assessed under a timeframe of one year which started in December 2007 and ended in November 2008. The communication strategies which were under observance included interactive automated phone calls, personalized compliant messages, and educational barrier-breaking messages. The educational messages given to patients on the importance of statin medication were also assessed during the study (Nimalasuriya and Antwerp 2010).
The results of the study showed 88% of the target population were reachable through the communication strategies used during the study while the rest were unreachable. The impact of communication on statin adherence was noted to be an 85% improvement when the study was initiated. Before the study commenced, 21% of statin patients did not hear the message relayed by their doctors on statin medication treatments which means that their adherence to statins was low. During the study, an 85% improvement was noted as 39% of statin patients were able to understand their doctor’s instructions on how to adhere to statin treatment plans. Nimalasuriya and Antwerp (2010) noted in their discussion that 27% of patients who had not intended to refill their statin medication did so after communication strategies used by their doctors improved the level of communication which in turn improved statin adherence.
Pedan et al (2007) also conducted a study to determine the effect of communication and information in the adherence to a statin medication. Their study drew in 6,436 sick persons who had started statin treatment via the use of 2 huge nationwide chains of pharmacy. The aim of their study was to determine what caused variations in the patient’s statin adherence where patients treated by either physicians or pharmacists were assessed. The research design used for the study was a randomized controlled trial where patients receiving statin therapy through pharmacy care programs and usual care programs were analyzed to determine their rate of adherence (Pedan et al 2007).
Six months after the randomization of the trial, the adherence to statin medication was recorded to be 70% among patients who were under the usual care program while the adherence to statins was recorded to be 96% among patients that were under the pharmacy care group (p<0.001). The type of communication techniques used by pharmacy care programs included statin adherence aids such as custom-packaged blister packs and follow-up phone calls by pharmacists. Pedan et al’s study demonstrated that there was a variation in patient adherence to statin medication which was explained by the type of communications approach used to relay treatment plans to patients. Their study noted that 47% of patients under the usual care program used by doctors had a low statin adherence to their medication as they did not ask their doctors any questions with regards to their treatment plans (Pedan et al 2007).
The results revealed that two-thirds of physicians did not ask their patients any questions with regards to the side effects of statin medication as well as the barriers to completing their medication. Pedan et al (2007) noted that physicians with good interpersonal and communication skills made it easier for patients to discuss their problems with statin medication easier. Patient characteristics such as socioeconomic status and motivation also affected adherence to statin medication where these factors impacted how patients sought medical advice for their statin therapy. Pedan et al (2007) also noted that patients who were better educated and well informed were able to find physicians with good communication skills.
Another study conducted to determine the effect of communication on statin adherence in patients was performed by Casebeer et al (2009). The research focused on determining the effectiveness of education programs initiated by doctors and pharmacists to facilitate statin adherence in patients. A controlled trial was used to test the effectiveness of such programs which included a brief counseling kit used by physicians when treating patients and patient mailings. The endpoint of the study was to determine the adherence to filling statin prescriptions during a 120-day period. The total number of patients involved in the study was 1,949 while the number of physicians recruited for the study was 234 (Casebeer et al 2009).
The physicians were drawn from various fields in medicine such as cardiology, family medicine, and human anatomy within the 39 states in the US. An analysis of the study’s results revealed that nearly all of the patients felt that their physicians listened to them and explained their statin treatment in a clear and careful way. However 246 (14%) out of the 1,949 patients were not able to raise their concerns with their doctors especially if the doctor did not ask them. The table below demonstrates the results of the physician-patient communication.
(Source: Casebeer et al 2009)
As demonstrated by the table above, many of the patients included in the study noted that their physicians established dialogue with their patients when it came to determining their statin therapy and medication plans. Many of the patients had established communication relationships with their doctors which made it easier for them to seek more information on statin medication and the side effects of statins. Patients who were able to gain advice from their physicians were able to have a higher adherence to statin medication when compared to patients who did not have any dialogue with their doctors (Casebeer et al 2009).
Conclusion
The purpose of this study has been to examine the aspect of patient behavior when it comes to adherence to a statin medication. The various characteristics of patients such as their age, gender, and socio-economic status were used to determine their adherence rates to a statin medication. The results demonstrated that these characteristics affected the adherence rates of patients to their statin medications which means that patient behavior and characteristics played an important part in influencing the adherence of patients to their statin medication.
References
Anderson, S. A., Hjelstuen, A. K., Hjermann, I., Bjerkan, K. & Holme, I. (2005). Fluvastatin and Lifestyle Modification for Reduction of Carotid Intima-Media Thickness and Left Ventricular Mass Progression in Drug-Treated Hypertensives. Vol. 178, No. 2, pp 387-397.
Batal, H.A., Krantz, M.J., Dale, R.A., Mehler, P.S., and Steiner, J.F., (2007) Impact of prescription size on statin adherence and cholesterol levels. BMC Health Services Research, Vol. 7, p 175
Benner, J.S., Glynn, R.J., Mogun, H.,Neumann, P.J., Weinstein, M.C., Avorn, J.,(2002) Long-term persistence in use of statin therapy in elderly patients, Journal of American Medical Association. Vol. 288, Vol.455-461
Benner, J.S., Pollack, M.F., Smith, T.W., Bullano, M.F., Willey, V.J., and Williams, S.A., (2005) Association between short-term effectiveness of statins and long-term adherence to lipid-lowering therapy. American Journal of Health and Systematic Pharmacy. Vol. 62, No.14, pp 1468-1675
Blackburn, D.F., Dobson, R.T., Blackburn, J.L., Wilson, T.W., Stang, M.R., and Semchuk, W.M., (2005) Adherence to statins, beta-blockers and angiotensin-converting enzyme inhibitors following a first cardiovascular event: a retrospective cohort study. Canadian Journal of Cardiology, Vol.21, No.6, pp 485-488
Brookhart, M.A., Patrick, A.R., Schneeweiss, S., Avorn, J., Dormuth, C., Shrank, W., Van Wijk, B.L., Cadarette, S.M., Canning, C.F., and Solomon, D.H., (2007) Physician follow-up and provider continuity are associated with long-term medication adherence: a study of the dynamics of statin use. Arch. Intern.Med., Vol.167, No.8, pp 847-852
Campione, J.R., Sleath, B., Biddle, A.K. and Weinberger, M., (2005) The influence of physicians guideline compliance in patients statin adherence: a retrospective cohort study. American Journal of Geriatric Pharmacotherapy, Vol.3, No.4, pp 229-239
Caspart, H., Chan, A.K., and Walker, A.M., (2005) Compliance with a stain treatment in a usual-care setting: retrospective database analysis over 3 years after treatment initiation in health maintenance organization enrolees with dyslipidemia. Clinical Therapy, Vol.27, No.10, pp 1639-1646
Casebeer, L., Huber, C., Bennett, N., Shillman, R., Abdolrasulnia, M., Salinas, G.D., and Zhang, S.,(2009) Improving the physician-patient cardiovascular risk dialogue to improve statin adherence. BMC Family Practice, Vol. 10, No.48, pp 1-8
Chiang, C.A., Pella, D. And Singh, R.B., (2004) Coenzyme Q10 and adverse effects of statins. Journal of Nutritional and Environmental Medicine, Vol.14, No.1, pp 17-28
Deddens, J.A., and Petersen M.R., (2004) Estimating the relative risk in cohort studies and clinical trials of common outcomes. American Journal of Epidemiology, Vol.159, pp 213-214
Endo, A., (1992) The discovery and development of HMG-CoA reductase inhibitors. J.Lipid Res., Vol.33, No.11, pp 1569-1582
Golomb, B.A., Dimsdale, J.E., White, H.L., Ritchie, J.B., and Criqui, M.H., (2008) Reduction in blood pressure with statins: results from the UCSD stain study, a randomized trial. Arch. Intern. Med., Vol.168, Vol.7, pp 721-727
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. (2003). Measuring Inconsistency in Meta-Analyses. Vol. 327, No. 7414, pp 557-560.
Huser, M.A., Evans, T.S., and Berger, V., (2005) Medication adherence trends with statins. Adv. Ther, Vol. 22, No.2, pp 163-171
Jackevicius, C.A., and Mamdani, M., (2002) Adherence with statin therapy in elderly patients with and without acute coronary syndromes. Journal of American Medical Association, Vol.288, No.4, pp 462-467
Kedward, J., and Dakin, L., (2003) A qualitative study of barriers to the use of statins and the implementation of coronary heart disease prevention in primary care. General Practitioner, Vol. 53, No.494, pp 684-689
Klein, B.E., Klein, R., Lee, K.E., and Grady, L.M., (2006) Statin use and incident nuclear cataract, Journal of American Medical Association, Vol.295, No.23, 2752-2758
Law, M.R., Wald, N.J., and Rudnicka, A.R., (2003) Quantifying effect of statins on low density lipoprotein cholesterol, ischaemic heart disease and stroke: systematic review and met-analysis. BMJ, Vol.326, No. 7404, p 1423
Munger, M.A., Van Tassell, B.W., and LaFleur, J., (2007) Medication nonadherence: an unrecognized cardiovascular risk factor. General medicine, Vol. 9, No.3, p 58
Nakamura, H., Arakawa, K. & Itakura, H. (2006). MEGA Study Group. Primary Prevention of Cardiovascular Disease with Pravastatin in Japan (MEGA Study).
Natarajan, N., Putnam, W., Yip, A.M. and Frail, D., (2007) Family practice patients’adherence to statin medications. Canadian Family Physician, Vol.53, No.12, pp 2144-2145
National Collaborating Centre for Primary Care (NCCPC) (2010) NICE clinical guideline 67: lipid modification. London: National Institute for Health and Clinical Excellence
Nimalasuriya, A., and Antwerp, G.V., (2010) Improving statin adherence through interactive voice response (IVR) technology and barrier breaking communications. Washington, DC: The Forum 10
Nissen, S., Nicholls, S., Sipahi, I., Libby, P., Raichlen, J., Ballantyne, C., Davignon, J., Erbel, R., Fruchart, J., Tardif, J., Schoenhagen, P., Crowe, T., Cain, V., Wolski, K., Goormastic, M., and Tuzcu, E., (2006) Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: the ASTEROID trial, JAMA, Vol.295, No.13, pp 1556-1565
O’Connor, P.J., Gray, R.J., Maciosek, M.V., Fillbrandt, K.M., DeFor, T.A., Alexander, C.M., Weiss, T.W., and Teutsch, S.M., (2005) Cholestrol levels and statin use in patients with coronary heart disease treated in primary care settings. Prevention of Chronic Disorders, Vol. 2, No.3, A05
Osterberg, L., and Blaschke, T., (2005) Drug therapy: adherence to medication. New England Journal of Medicine, Vol. 353, pp 487-497
Pedan, A., Varasteh, L.T., and Schneeweiss, S., (2007) Analysis of factors associated with statin adherence in a hierarchical model considering physician, pharmacy, patients and prescription characteristics. Journal of Management Care Pharmacy, Vol. 13, No. 6, pp 487-496
Perreault, S., Blais, L., Dragomir, A., Bouchard, M.H., Lalonde, L., and Laurier, C., (2005) Persistence and determinants of statin therapy among middle-aged patients free of cardiovascular disease. European Journal of Clinical Pharmacology, Vol. 61, pp 667-674
Rifkin, D.E., Laws, M.B., Rao, M., Balakrishnan, V.S., Sarnak, M.J., and Wilson, I.B., (2010) Medication adherence behaviour and priorities among older adults with CKD: a semi-structured interview study. American Journal of Kidney Diseases, Vol.56, No.3, pp 439-446
Schneeweiss, S., Patrick, A.R., Maclure, M., Dormuth, C.R., and Glynn, R.J., (2007) Adherence to statin therapy under drug cost sharing in patients with and without acute myocardial infarction. American Heart Association, Vol.115, pp 2128-2135
Shroufi, A., and Powles, J.W., (2010) Adherence and chemoprevention in major cardiovascular disease: a simulation study of the benefits of additional use of statins. Journal of Epidemiology in Community Health, Vol.64, pp 109-113
Silva, M.A., Swanson, A.C., Gandhi, P.J., and Tataronis, G.R., (2006) Statin-related adverse events: a meta-analysis. Clinical Therapy, Vol. 28, No.1, pp 26-35
Steinberg, D., (2007) The cholesterol wars: the sceptics vs the preponderance of evidence. New York: Academic Press
Sweetman, S.C., (2009) Cardiovascular drugs. London, UK: Pharmaceutical Press Wei, L., Wang, J., Thompson, P., Wong, S., Struthers, A.D., and MacDonald, T.M., (2002) Adherence to statin treatment and readmission of patients after Myocardial infarction: a six year follow up study. Heart, Vol.88, No.3, pp 229-233
Wright, J. M., & Abramson, J. (2007) Statins For Primary Prevention of Coronary Disease. Journal of the American Medical Association, Vol. 369, No. 9567, p 1079.
Yilmaz, M.B., Biyikoglu, S.F., Guray, Y., Karabal, O., Caldir, V., Cay, S., Sahin, O., Sasmaz, H., and Korkmaz, S., (2004) Level of awareness of on-treatment patients about prescribed statins. Cardiovascular Drug Therapy, Vol. 18, No.5, pp 399-404