Introduction
The Australian Healthcare System (AHS) provides healthcare benefits for millions of Australian citizens and is regarded as one of the best examples of healthcare providers. The system is modeled along the lines of the US and UK healthcare systems and is funded by the government, employers, and their employees. This paper examines the Australian Healthcare System and develops an understanding of how it is structured and how it functions.
The organization and structure of local, state, and federal health services
Brief History
The health services of the US and Australia have certain common features such as a robust private physician network, private health insurance but Australia has a publicly financed health insurance system that is forceful, and privately financed alternatives are also available. The publicly financed system needs to essentially be able to compete against the private systems. Before 1972, AHS was not coordinated efficiently and was based on the patient’s ability to pay while private health insurance was growing. In 1972, the Australian government brought in a publicly financed insurance system called Medibank that was implemented in 1975. This was a compulsory health insurance system that was financed through income tax on employees and businesses. Many amendments and revisions were made and also included private insurance. In 1984, a new system called Australian Medicare was introduced to replace the Medibank system (The Australian Health Care System, February 1992).
Structure of AHS
Healthcare is provided through private and public healthcare systems. The policy, regulation, and service planning are done by the two levels of government bodies and active participation is also provided by doctors and medical professional organizations. Medicare is the major provider of care and it gives people access to subsidized rates for out-of-hospital medical care, free choice of the doctor, subsidized medicines and hospital care, and free public hospital care. Medicare is financed by the Commonwealth and State and Territory Governments. The policy objectives are to provide universal access to Australian citizens, affordable rates at quality care, equity in treatment, and the distribution of costs, and the allocation of resources and efficiency. The major part of the healthcare is given by general practitioners who have private practices in the community. These GPs are often self-employed and have a license and contract to practice. Medical bills and services are paid by the patient through Medicare rebates. Facility for direct billing or bulk billing is also available and the patients are not charged any money but the bill is directly paid by Medicare to the hospital. Free of charge public hospitals, accident and emergency hospitals, hospitals in rural areas also provide free care, and these units are funded by the State and Territory governments or through Medicare rebates. Secondary ambulatory care is provided in private hospitals by GPs or specialists who charge rebated rates as per the Medicare subsidy. Free of charge medical care is also provided by community hospitals and outpatient clinics. It must be noted that GPs play a very vital role in this system. Non-Primary healthcare is only provided at a rebate if they are referred to a specialist or hospital through a GP (Pflaum 2001).
Programs Funded by AHS
AHS funds a number of programs as part of the health care system. The Australian government funds initiatives for public health activities such as purchasing medicines and vaccines and programs that are facilitated by the Australian Divisions of General Practice and Aboriginal Medical Services. It also provides funding for many other grant programs that are aimed to improve medical and nursing worker participation in rural and remote areas and other areas of workers shortages. AHS includes privately supplied goods and services such as dentists, complementary therapies, aids, appliances, and other health professionals. A brief discussion of these programs is provided in the following section (Health overview 2006).
- MBS – Medicare Benefits Schedule: This is a universal program that gives people access to privately provided medical services. It may also include co-payments by consumers when the cost of healthcare services is not fully covered by the rebate.
- PBS – Pharmaceutical Benefits Scheme: Provides subsidies to extensive prescription medicines that are supplied by community pharmacies.
- PHI – Private Health Insurance (PHI) Rebates: This is a system of rebates for subsidizing the cost of premiums to private health insurance.
- AHCAs Australian Health Care Agreements: These provide the major transfer for funds from the Australian Government to the state and territory counterparts to contribute to the funding of free public hospital services.
- photos Public Health Outcome Funding Agreements: These are bilateral funding agreements between the Australian Government and the states and territories to provide a variety of public health programs.
Role and function of government and non-government agencies
The government plays the main role of a mediator in the AHS system. There are a number of agencies that ensure proper planning and implementation of policies and schemes are done. Figure 1. AHS Overview provides an overview of the health system and the various stakeholders and players (Pflaum 2001).
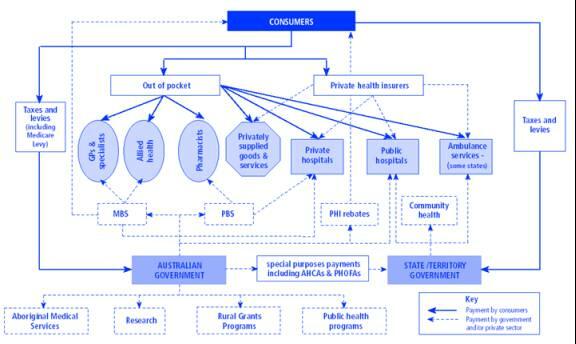
There are many different entities, both government and non-government, that play a role in the size and distribution of resources for AHS and the medical workforce as well as the quality, safety, and affordability of medical services supplied to the community. The Commonwealth government has overall responsibility and ensures that the required outcomes meet people’s needs. The Government’s means of direct influence is however limited, and responsibility and activities are assumed by a number of parties. The roles and functions of various government bodies and non-government agencies are explained below (Pflaum 2001).
- DC – Department of Health and Aged Care: Puts a cap and places a restriction on access by certain types of practitioners to Medicare benefits. This is aimed at putting a positive influence on the quality of medical services and workforce distribution. It also administers and provides funds for initiatives that are designed to improve the accessibility, safety, and quality of care. It also places restrictions on the number of medical schools that are subsidized so that there is no oversupply of medical practitioners (Pflaum 2001).
- HIC – Health Insurance Commission: This body administers Medicare Benefits and other Commonwealth programs. HIC also undertakes education, feedback, and implementing best practice programs with the help of medical professional bodies (Pflaum 2001).
- Professional Services Review Statutory Authority: This is responsible for the investigation of suspected cases of inappropriate practice by medical or other health practitioners, particularly in relation to services that attract a Medicare or Pharmaceutical Benefits Scheme benefit (Pflaum 2001).
- DETYA – Department of Education, Training and Youth Affairs: This body looks after the subsidy of primary medical education and ensures that universities are able to provide the required number of healthcare professionals for future needs (Pflaum 2001).
- GPET – General Practice Education and Training: This body was created in March 2001 as a Commonwealth-controlled company. It provides funds and administers the post-graduate, general practice, and vocational training (Pflaum 2001).
- Department of Immigration and Multicultural Affairs: This body specifies criteria for temporary and permanent entry of overseas trained doctors, designed to contain growth in oversupplied parts of the medical workforce while allowing supplementation of services in areas of shortage (Pflaum 2001).
- State and Territory Governments: These are government bodies that analyze the requirement of funds. They look after the distribution of government funds for community health services, public hospitals, medical services, specialists vocational training. They also undertake the funding of rural medical workforce and infrastructure. These bodies also have involvement in setting up medical registration standards and conditions for qualifications. They also determine through the medical registration boards if practitioners such as overseas trained doctors can be allowed to practice legally and the extent and scope of their practice. These bodies also employ large numbers of practitioners for the hospitals and the community health sector (Pflaum 2001).
- AHMAC – Australian Health Ministers’ Advisory Council: This body uses AMWAC to analyze and recommend adjustments to the size and structure of the workforce, as a basis for Commonwealth and State planning decisions (Pflaum 2001).
- AMC – Australian Medical Council: This is a national standards body for primary medical training, advises and makes recommendations to State and Territory Medical Boards on the accreditation of Australian and New Zealand medical schools and medical courses, and the assessment for admission to the practice of overseas trained doctors. The Council is also developing a system of accreditation of the specialist training and professional development programs run by specialist medical colleges (Pflaum 2001).
- Professional representative groups: There are a number of professional working people groups and they play an active role in shaping the policies and schemes. Some of them are ASMOF – Australian Salaried Medical Officers’ Federation, RDAA – Rural Doctors Association of Australia, Rural Health Association, Australian Medical Association, Australian Medical Students’ Association, and many others (Pflaum 2001).
- Divisions of General Practice: These are based in different geographical locations and help to improve the health outcomes for patients by asking GPs to interact with other health professionals and help to improve the health service delivery in local areas. These divisions obtain funding from the commonwealth government and provide support and services to GPs and meeting the responsibilities for health systems for consumers (Pflaum 2001).
- Rural Workforce Agencies: These are present in all states and the northern territory and increases access to primary health care services through recruitment and retention of GPs (Pflaum 2001).
Strength and weaknesses of the Australian health care system
AHS has very healthy participation and is widely regarded as a good example of how managed care should be administered. The Australian government spends about 79 $ annually on the healthcare system and out of this amount, the government contributes around 45% in the form of subsidies. In 2006, it has provided a safety cover net to 1,532,617 people. These figures show the excellent coverage that the government provides and the service it renders. The life expectancy has increased to 80.1 years (Health expenditure, 2006).
Podger (Podger 2006) has pointed out that the success of healthcare systems is unfortunately not been used for the indigenous people of Australia who continue to suffer. He has also pointed out that with the increase in life expectancy, the number of older people, above 65 people has increased substantially. Such people are actually designated as chronically ill and have ailments related to diabetes, cancer, heart problems, and other diseases and such people avail almost 80% of the healthcare budget. The author further suggests that such people go more times to the hospital than is required and this creates a long list of people who wait for care. The burden of providing sustained care will engulf the resources of AHS. Podger has also suggested that the current policies are targeted more at providing care and little has been done to advise the public about reducing obesity and other problems. The author has also pointed out inefficiencies related to functional aspects and also about the funding provided to different areas of AHS.
Significance of implementing best practice and quality management policies
Fletcher (2000) has pointed out the importance of having quality in healthcare systems and he has suggested that quality needs to be implemented not only with reference to technology and actual medication but also in the whole aspect of the system to improve its efficiency and reduce the waiting time for patients. With increased awareness from patients and international attention with regards to potential harm to the patients with clinical intervention, it has become essential to absorb quality healthcare indicators from US and UK systems. Implementation of quality systems with reference to providing good healthcare comes from the basic ethical concepts of the medical profession where care for the patient assumes the important goal. In addition, patients resort to legal means when they are denied access to appropriate healthcare or when they feel that the care has caused them harm.
The Institute of Medicine gives a widely cited general definition of the quality of health service provision: “The degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge. In June 1995, the Task Force on Quality in AHS released a report that suggested a number of measures and remedies to improve the quality of service. The National Expert Advisory Group of Safety and Quality was established in March 1997 to improve safety and quality. According to the author, the concept of quality is specified with reference to safety, effectiveness, performance appropriateness, and outcome. He has suggested that the quality management systems should answer the following issues:
- Effectiveness – Was it the right thing to do
- Appropriateness – Was the right thing done
- Performance, Safety, and Technical issues – Was the right thing done properly and well
- Acceptability – Was the outcome satisfactory
- According To Fletcher, a framework has been devised to provide for benchmarking against the best practices in UK and US. The framework is made of three critical components and they are:
- Structure of healthcare: This component refers to the conditions in which the treatment to the patient was given and the training that was given to the healthcare professional.
- Care Process: This component refers to the characteristics of the activities performed in receiving and giving care
- The outcome of Care: This component refers to the effect that care has on the health of patients.
The author has provided a quote from another author and this gives the whole meaning to quality and healthcare.
“If we can take any lessons from the stunning progress in safety in aviation and other high risk injuries it is that fear, reprisal and punishment produce not safety but rather defensiveness, secrecy and enormous human anguish. Scientific studies in human factors, engineering, organizational psychology, operations research and many other disciplines make it clear that in complex systems, (quality and) safety depends not on exhortation, but rather on the proper design of equipment, jobs, support systems and organizations. If we truly want safer care, we will have to design safer care systems.”
Conclusion
The paper has examined the structure of AHS and examined key components of the system. Issues related to the strengths and weaknesses of the system have been examined. The paper has also studied the necessity of improving the quality of healthcare systems and examined the recommendations for introducing a framework designed to improve the quality of service and to absorb the best practices related to healthcare systems.
References
- Fletcher Martin (2000), ‘The Quality of Australian Health: health care
- Current Issues and Future Directions’, Commonwealth Department of Health and Aged Care: Canberra, ISBN 0642415900
- Health overview (2006), ‘2006 Health and Ageing Factbook’
- Health expenditure (2006), ‘2006 Health and Ageing Factbook’
- The Australian Health Care System (1992), ‘Historical Origins’, Lessons learned from The Australian Health Care System, Oklahoma Medical Research Foundation, Tulsa, Oklahoma
- Podger Andrew (2006), ‘A Model Health System For Australia’
- Pflaum Monica (2001), ‘The Australian Medical Workforce’, Commonwealth Department of Health and Aged Care, Canberra, ISBN 0642735956