Purpose and Key Objectives in Surgical Practices
Surgical practice is a type of nursing activity where a healthcare provider performs surgery on patients to address their needs. The main objective and purpose of a surgical procedure are to provide a high standard of medical care to address patients’ needs. In exercising their duties, surgeons should complete confidentiality to not leak patients’ details to the public without their consent, working with integrity and impartiality to avoid favoring particular people. In surgical practice, nurses and doctors need to be courteous all the time to evade causing accidents. They should be friendly, approachable, and helpful to create a safe and effective environment. The surgery team should be well trained to make informed decisions based on evidence (Parameswaran & Agarwal, 2018). If gained, such skills and experiences can also enable them to offer patient-centered services through effective communication and good relationships. The group should be well motivated and has to monitor and evaluate patients’ needs to take the appropriate action. All stakeholders should be treated with respect and dignity, while equality and diversity should be embraced.
Role of Nursing Theories in Nursing Practice Development
Nursing theory plays a crucial role in the development of nursing practice, having an influence on different aspects of the profession. Models such as Watson’s caring theory help nurses develop concrete concepts useful in clinical practice. Appropriate application of correspondent theory helps in addressing issues and problems experienced in a clinical realm. Nursing theory provides a framework in which adequate nursing interventions can be promoted and implemented into practice. While training to become healthcare providers, students apply such concepts to develop skills that help improve patients’ quality of life. Basing their work on nursing theories, health practitioners can learn their roles in the healthcare setting and address the issues faced during their practice (McKenna et al., 2015). The principles of nursing are crucial in developing scientific pieces of evidence for decision-making during practice as well as enhancing practitioners’ understanding and appreciation of the values and meaning of their profession.
The Strengths and Limitations of the Application of Theories in Nursing Practice
Nursing theories have various benefits for both healthcare workers and patients in many ways. From the nursing models, health professionals can develop unique knowledge and skills that can be used to address the different needs of patients in a community. They can be tested and added to the professional knowledge that already exists among practitioners. Nursing principles highlight the values and contributions of a given nurse. Theories provide a working consensus among health providers since they enable to development of both practical and theoretical tools that can be applied by all nurses in a given facility (Quinn Griffin & Landers, 2015). The use of a nursing model provides a common language to allow nurses to discuss their practice. Thus, through nursing theories, healthcare workers can agree on a given concept that can be used to address patients’ needs.
Nursing theories also give a set of frameworks that guide the process of training and practice in the field. The design shape and structure the nursing assessment and enable precise identification of nursing problems associated with patient needs. Such an approach helps plan, implement, and evaluate clinical methods, ensuring effective healthcare practice. Nursing models provide for precise interventions while handling patients, thus limiting the chances of making errors because a nursing model gives clear guidance on the knowledge and skills required to deliver care. Lastly, through these theories, patients can receive routine nursing care based on their needs.
However, nursing theories also have some limitations that may hinder the provision of care. They are criticized for the frequent use of jargon and complex concepts that are difficult to grasp. This leads to a wastage of time among practitioners since they have to learn and understand these terminologies for them to be effectively used. Some models use vocabulary that is not easily understood, while some are leading to wrong interpretations. Most nursing theories originate from the United States of America, and therefore, their interventions are majorly applicable in American society (Quinn Griffin & Landers, 2015). Therefore, their applicability, values, and philosophical beliefs do not resonate well with patients’ needs from other regions. Some theories are based on narrow perspectives that do not capture nursing as a whole since they are based on individual authors’ values and beliefs.
Some nursing theories have received criticism for lacking relevance to nursing practice’s reality and have increased the gap between what is believed and practiced. Certain models lack practicality and have remained descriptive and explanatory, thus failing to address patients’ needs. The application of theories based on different disciplines to explain a healthcare problem in another area has proven inadequate. Some ideas have become obsolete due to technological advancements and emerging trends in the healthcare system. Other models majorly focus on improving professionalism among health providers yet give little insight into patient care.
Improving Kidney Transplant Surgery Process
Surgery is a complex process that requires a lot of focus and accuracy to ensure patient care is achieved. The surgeon in charge of any surgical procedure should acquire the needed expertise and experience to avoid complications in the process. Today, some patients are going as far as choosing experts who they feel should operate on them based on their credentials. Life is precious, and nobody would wish to lose it. Therefore, every surgery should be done based on the procedures, guidelines, protocols, and sometimes with a team of experts to monitor any eventuality. Decisions should be evidence-based and made in the best interest of the patient (Patzer et al., 2016). In conducting a kidney transplant, a surgeon needs to be careful from the beginning until the end of the procedure to avoid rejection of the donor organ and other side effects. Since organ transplant is the most complicated surgical procedure, many improvements are needed to ensure minimal risks.
Watson’s theory of care highlights the need to form a good relationship between patient and health provider to have positive health outcomes. It emphasized the need to have authentic care for patients and their family members. Her reasoning borrows a lot from nightingale’s environmental theory, which focuses on providing a conducive healing environment. Watson goes further to explain how social relationships affect health outcomes. When caregivers can develop good relationships with patients, a lot of care would be taken in every medication step, hence minimizing adverse outcomes (Watson & Bohart, n.d.). Rejection of kidney majorly occurs when patients’ blood forms antibodies in response to the donor’s blood. To avoid such, health practitioner needs to conduct tests on both the patient’s and donor’s blood and human leukocyte antigen (HLA). If the donor’s blood type and body tissue match that of the patient, then a procedure can be scheduled.
Therefore, to accurately undertake these tests, a surgeon needs to cultivate caring. The ability to facilitate caring exists only when the nursing practitioner went through a nursing education curriculum embedded in authentic care practice. Such professionals hold values and beliefs that can create an environment for nursing care to be delivered. In other words, he or she can determine the lens that will guide his or her practice. Positive feelings, kindness, and trust must be built between caregivers and patients to report accurate information on the tests honestly. The most appropriate donors are always family members, but sometimes patients may fail to have close relatives who can donate a kidney to them. Therefore, surgeons need to engage their teaching-learning experience to conduct accurate dialysis on potential donors to identify the right match. After surgery, a positive healing environment emphasized by nightingale should be created to enhance patients’ quick recovery. Additionally, nurses should devote themselves to ensuring the patient can heal by providing for their needs. This principle is emphasized in Henderson’s need theory and is vital in ensuring a quick recovery.
Metaparadigm
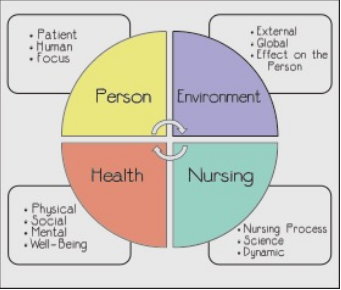
Metaparadigm is a set of theories based on four concepts; person component, health, environment, and nursing. It provides a holistic structure that describes how a given nursing practice, such as surgical development, should function. The person component emphasizes the receiver of care as well as his or her family members. For a positive healthcare outcome to be realized, a patient’s social and health needs must be attained. Everyone is unique and belongs to different cultural diversities; therefore, nurses should treat all patients with dignity by respecting their cultures and languages (Bender, 2018). While conducting a surgical procedure on a patient, the surgeon needs to communicate and handle him or her with respect. The environment component of the nursing metaparadigm centers on how a patient’s surroundings affect health and wellness. Interactions with physical factors such as family, friends, nurses, and social factors such as culture, technology, and economic conditions can affect patients’ healing process.
The health component focuses on the wellness and care services the patient can access. For positive health outcomes, high-quality care should be administered. The lifespan of an individual, emotional, intellectual, and spiritual well-being affects the healing process. In general, these factors affect a patient’s state of well-being; thus, they should be integrated into healthcare. Individual who has undergone a surgical process should emotionally and spiritually be supported to enhance positive health outcomes (Branch et al., 2016). The nursing component emphasizes on delivery of optimal health care based on mutual relationships safety and patients. Therefore, to obtain a patient’s well-being, nurses need to offer a high degree of services by using their skills, knowledge, and available technologies. The best possible scenario in the surgical procedure can be attained when the surgeon collaborates with the patient and applies his or her values and beliefs. Figure 1 below highlights the components of the metaparadigm and the factors that affect them.
Strengths and Lack of Applicability to a Surgical Procedure
Metaparadigm components can be applied in surgical practice in many ways. The person component highlights the patient’s social and health needs, which are vital during the surgical procedure. When surgeons treat patients with dignity and respect, they would be able to involve them in every decision concerning their health. Following such an approach would result in a positive relationship and eventually modify the patient’s environmental factors, hence better health status (Branch et al., 2016). The health component applies to surgical practice since it focuses on the well-being of the patient. For effective recovery to occur, high quality needs to be offered; thus, the health concept emphasizes the need to conduct surgical procedures with due diligence to enhance wellness. The nursing component highlights nurses’ need to use their skills, expertise, and technological resources available while offering care. It can therefore be relevant during dialysis and kidney transplant process to enhance positive outcomes.
However, some factors in metaparadigm concept may not apply to surgical practice such as kidney transplants. First, a person’s spiritual factor may not be applicable during surgery since at this moment only the knowledge, skills, and expertise of the nurse are crucial rather than spiritual beliefs. societal beliefs, values, and expectations in the environment concept may be applicable during the procedure since nursing interventions are specific and may not conform to such factors. Realities of one’s health status may undermine his level of wellness. In particular, one may die during the procedure not because of the doctor’s incompetence but of poor health status based on underlying conditions. Furthermore, due to socioeconomic inequalities, some facilities may lack the necessary equipment to conduct a procedure. In this case, a patient may die due to a system failure as opposed to the practitioner’s inability.
Strengths and Limitations of Nightingale, Watson, Henderson’s Theories
Watsons’ theory of care is essential since it can be used to guide and improve practices. It provides nurses with a satisfying concept for their practice hence holistic care. Caring-love, creative factors, Caritas, and other concepts are easily understood when practiced and experienced. However, the model does not give direction on how to achieve authentic caring-healing relationships. Some of its elements require the application of other models to be understood (Quinn Griffin & Landers, 2015). The Caritas concept takes much time to be incorporated into practice. Nightingale’s theory is straightforward and clear as it gives relationships between nurse, patient, and environment directly. Its environment paradigm is vital since poor sanitation significantly contributes to illness.
The model has some limitations; for instance, it does not mention how to handle dependent or too needy patients. Nightingale’s assumptions that diseases are caused by dirty and ill-ventilation may not be accurate. Henderson’s theory applies to the health of individuals of all ages. Its hypotheses can be tested and assist in increasing the general body of knowledge within the discipline. Nursing practice ideas are well accepted and can be utilized by practitioners to guide and improve their practice. However, it has limitations; particularly, it does not provide a conceptual linkage between physiological and other human characteristics. Henderson’s theory also Lacks an inter-relate of factors and the influence of nursing care.
Measures to Evaluate the Implementation
In evaluating theories, several measures have to be taken into account; for instance, the significance of a model needs to be estimated in comparison to others that may have the same concept. Parsimony, which is the flexibility of a model, can also be evaluated to ascertain if it can be used in different sections of a discipline. Testability is essential to assess the accuracy of a theory. Empirical adequacy and pragmatic adequacy evaluate both the suitability and practicality of models (Niemand & Mai, 2018). Additionally, congruence models are evaluated based on history, fundamental elements, and relational statements.
References
Bender, M. (2018). Re-conceptualizing the nursing metaparadigm: Articulating the philosophical ontology of the nursing discipline that orients inquiry and practice. Nursing Inquiry, 25(3), e12243.
Niemand, T., & Mai, R. (2018). Flexible cutoff values for fit indices in the evaluation of structural equation models. Journal of the Academy of Marketing Science, 46(6), 1148-1172.
Branch, C., Deak, H., Hiner, C., & Holzwart, T. (2016). Four Nursing Metaparadigms. IU South Bend Undergraduate Research Journal, 16, 123-132.
McKenna, H., Pajnkihar, M., & Murphy, F. (2015). Fundamentals of nursing models, theories and practice, with Wiley E-text. John Wiley & Sons.
Parameswaran, R., & Agarwal, A. (2018). Evidence-based endocrine surgery. Springer.
Quinn Griffin, M. T., & Landers, M. G. (2015). Extant nursing models and theories: Grand and middle range theories in nursing. Theories Guiding Nursing Research and Practice.
Patzer, R. E., Serper, M., Reese, P. P., Przytula, K., Koval, R., Ladner, D. P.,… & Wolf, M. S. (2016). Medication understanding, non‐adherence, and clinical outcomes among adult kidney transplant recipients. Clinical transplantation, 30(10), 1294-1305.
Watson, J., & Bohart, A. (n.d.). Humanistic-experiential therapies in the era of managed care. The Handbook of Humanistic Psychology: Theory, Research, and Practice, 585-600.