Introduction
My current job profile requires me to offer my services in the surgical/orthopedic ward. During my current job, I have come across several instances where the lack of pain assessment results in the suffering of the patients having pain. This persistent problem prompted me to choose a research topic that was relevant to my job. I am confident that once my research is over, I’ll be able to understand the actual meaning of pain assessment and management. This research will serve as a guide for my colleagues and other people in this profession.
To have a perfect understanding of their patient’s pain, nurses have to have optimal knowledge of the pain assessing skills and patient attitudes (McNamara et al.2012). At the same time, these must have a thorough knowledge of pain management. Such skills and management should be substantiated by suitable evidence on hand so that the patient doesn’t have to suffer much. Usually, patients are not ready to experience pain once they are under the care of any particular hospital. They are right in this approach because hospitals are meant to give optimum relief to their patients (McNamara et al.2012). Simultaneously, it is not acceptable on the part of nurses to have an insufficient understanding of their patient’s pain. It is an ethical or moral responsibility of nurses to be accountable to their professional job profiles.
The severity of pain assessment and management can be gauged from the fact that the Royal College of General Practitioners, UK, decided to make chronic pain “one of its four clinical priorities for 2011-2013” (Royal College of GPs announces chronic pain as clinical priority 2011). Baroness Gardner’s concern about pain, when she raised the issue in the House of Lords, further escalates the issue of pain assessment and management. Baroness Gardener expressed her concern about the competence of nurses in dealing with chronic pain (Chronic pain discussed in the House of Lords, May 2009 2009). Further, pain has been recognized as the fifth fundamental sign by the ‘Australian and New Zealand College of Anaesthetists’ and the ‘Chronic Pain Coalition, to ascertain “accountability for pain assessment and management” (Chronic Pain Policy Coalition 2007).
Nursing programs may as well add pain as a mandatory segment to educate future nurses about the skills and aptitudes required for handling patients who are experiencing acute pains. This will help them (the nurses) in assessing and managing pain with expertise from the very beginning of their professional careers. As a result, the patients will not have to bear severe pain and the potential risks of continuous pain might be decreased.
It is very critical to assess a patient’s pain encounters to implement pain management efficiently. However, it is not easy to assess the pain encounters of a patient. There are several factors involved in assessing the pain encounters of a patient. The same will be discussed further in this paper.
Nurses need to pay special attention while assessing pain in patients from diverse backgrounds. Pain cannot be measured by any scale since it doesn’t have any standards. Different patients have different perspectives of pain. Moreover, the tolerance level of patients also differs. It is obligatory on the part of nurses to ask their patients about their pain (Attar et al.2009). At the same time, nurses should not arrive at any conclusion simply based on the patients’ verbal description. The health care professionals must watch carefully the patients’ facial jargon and body movements. But again, even facial expressions are sometimes deceitful, as in the case of Native Americans. Native Americans tend to be indifferent to their pain (Munoz & Luckman 2005). They don’t express any emotions of pain. On the other hand, the Mexican Americans display clear indications of pain and agony (Munoz & Luckman 2005).
The above-mentioned points make it very important to research the competence of nurses to assess pain and implement pain management. Several types of research have been done on pain management. However, all these researches have concentrated on a particular aspect like pain assessment in children, pain assessment in elderly patients, pain assessment by military nurses, etc. My research will cover pain assessment and implementation of pain management in a generalized form; all the aspects will be covered. This research will be a guideline for all those who are in the profession of pain assessment and pain management implementation.
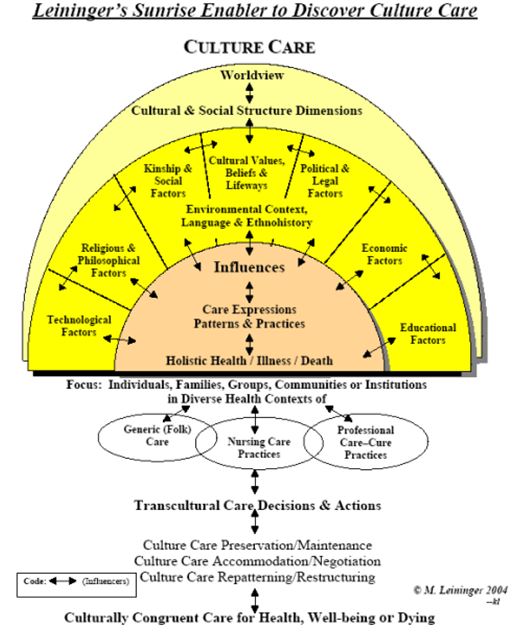
During the research, I have laid stress on the cultural aspect as well because it is also one of the main criteria for pain assessment. It has been observed that culture plays a vital role in the nursing practice. By culture, I mean the difference in ethnicities, language barriers, etc. Sometimes, due to the language barrier, nurses are not able to understand what the patients want to convey. The paper will also delve into this aspect.
Background
Acute pain is the most normal side effect of illness and the most commonly reported problem to specialists. However, perpetual agony can introduce a baffling issue for nurses, which has brought about the prevailing acceptance for the requirement for honed perpetual pain-relieving facilities in various nations. While the results of ceaseless pain are well archived, issues concerning ceaseless pain in certain individuals are not well documented, for instance, Melding discovered that out of the 4000 papers, related to pain, that were published annually, less than 1% pertained to older adults and that a survey of eight geriatric textbooks demonstrated that they just contained 18 out of 5000 pages on pain (Melding 1991). The particular issues of pain management in older adults have just started to be tended to efficiently during the past couple of years. In the context of the UK, the ‘National Service Frameworks’ has raised the importance of addressing constant pain experienced by people.
At the ‘International Association for the Study of Pain’ conference, it was proposed that the time had come for clinicians to make available specialized pain-relieving services to the people. It is astonishing to know that by the year 2020, there will be 2/3rd of older adults, in the total population, suffering from pain (Gibson 2002). Manias et al. (2011) suggest that among all the studies conducted on pain management, only 2.3 percent pertained to people above 65 years of age.
Nurses have a vital role to play in the pain assessment and pain management of their patients. Therefore, they need to have a thorough knowledge of pain assessment and pain management tools. At the same time, it is also equally important for them to have a positive attitude while treating their patients. Appendix 1 and Appendix 2 depict some commonly used pain assessment tools for children and older adults respectively.
Methodology
The researcher prepared a questionnaire that included all sorts of questions related to pain assessment and pain management implementation. The researcher was aware of the previous research done on this subject and its limitations. A lot has been written on pain assessment and management of pain in children, pregnant women, military personnel, etc., but what about pain assessment and treatment in elderly patients? There have indeed been studies about this segment but in my opinion, the same is not enough to understand the pain and its various aspects. These earlier researches concentrated on different groups such as children, pregnant women, military personnel, etc. Even though studies have been conducted on pain assessment and pain management in elderly people, the incidents of such studies are not many. Moreover, such studies are not enough to understand the various aspects of pain in elderly patients. So, to understand the general perceptions of pain assessment and pain management implementation in elderly patients, the researcher aimed the questionnaire at various sectors such as elderly people who earlier suffered from chronic pain, elderly patients presently suffering from chronic pain, and the nurses involved in the treatment of pain in elderly patients. The researcher referred to different scholarly articles and previous literature for this purpose.
The researcher conducted three different surveys. Each survey was directed at a different group of people. The first survey targeted the practicing nurses, the second one targeted the elderly people (65 and more years of age) who had earlier suffered from chronic pain, and the third one targeted the elderly people (65 and more years of age) who were currently suffering from chronic pain.
To know the viewpoint of the elderly patients about the treatment meted out to them during pain, the researcher questioned 112 such people (65 years and above). To ascertain the prevailing mindset of nurses about assessing pain, the researcher interviewed 138 practicing nurses. Out of these, 79 were from the older adults’ ward, and the remaining 59 were from the general ward.
The variety of sectors was included in the research because as is understood, people have different perspectives about their pain and their behavior is also different. So the nurses need to act accordingly while assessing their pain.
After the tabulation of the obtained data, they were analyzed using the SSPS statistical analysis tool. This process is effective when the data is varied and some average conclusion is to be arrived at.
Advantages of this methodology
By following this strategy, the researcher was able to have the point of view of all the concerned parties; the patients and the health care professionals. This helped the researcher in having unbiased results.
In this study, the effectiveness and efficacy of the health services provided by the nurses could be assessed. Also, the problems faced by the patients could be documented.
The biases can be avoided by proper matching of the cases and controls. The controls and the cases may differ in age, gender, occupation, etc, which can cause errors in the outcome. This can be prevented by proper comparability between the cases and the controls. Matching is defined as the selection of cases and controls which have selected variables such as age, gender, etc in common.
Another advantage is the easier analysis of the data. The outcome will be in terms of either positive or negative results. The incidence of result, either positive or negative is then tested for statistical significance.
The disadvantage of this methodology
Although experimental studies are mandatory in the field of delivery of health services, the ethical and logistical considerations often prevent the application of this methodology in studies concerning humans.
Biases are the main disadvantages of this kind of research. Matching and randomization can prevent bias to a certain extent, but cannot eliminate it. The biases are mainly due to errors of assessment by the human element.
Sources of the Information
The literary information for this research was taken from various scholarly articles (listed on the ‘references’ page). The data was collected with the help of three surveys targeted at various sectors such as elderly people who earlier suffered from chronic pain, elderly patients presently suffering from chronic pain, and the nurses involved in the treatment of pain in elderly patients.
Literature Review
The researcher referred to several scholarly articles to conduct this research. Care was taken that the maximum articles were from the UK. Research design is a plan or a framework for a study that guides to collect and analyze the data. It is the conceptual structure in researching with the economy in procedure. It is the blueprint of the work planned by the researcher. It helps the researcher to research in a well-planned manner Based on the problem selected for research the researcher frames a suitable research design.
Research design designates a plan of action that is to be conducted regarding the proposed work of research. The plan provides the guideline to the research and the process of research (Rogers 2010). This plan enables the researcher to keep track of his process, to verify that he is moving on the right path towards his goal. The research design includes the selection and presentation of a research problem, formulating a hypothesis, and methodology, data collection, testing of hypothesis, interpretation, presentation and report writing.
Pain assessment is a very tough job and it is seldom right if the patients’ self-reporting is not considered. Different categories of patients have different kinds of problems like children can’t express their pain exactly due to lack of expressional power, elderly do not express their pain because they do not want to disturb anyone, and especially men don’t want to reveal that they have become weak due to the pain (Harper et al.2007).
Pain Assessment in Older adults
Qualitative Analysis
Pain, being a personal experience, is very complicated to prove. In older adults, where verbal communication has become restricted, the expression of pain becomes very difficult (Harper et al. 2007). As such, the pain assessment becomes all the more difficult. In such circumstances, likely, the patient might not get the required treatment and as a result, the patient might not get the expected relief. It is also understood that patients don’t report pain because they don’t want to create any scene in the absence of any nurse (Harper et al. 2007).
Dewar (2006) suggests that it becomes difficult to assess pain in older patients because of other health problems and the compassion towards the pain-relieving treatment. Another factor that slows down the pain management system in older patients is their beliefs and approach towards the pain-relieving medication. The nurses probably lack knowledge about pain assessment in older patients. There are certain organizational constraints also that slow down the process. All such factors make it complicated for the nurses to offer perfect and timely treatment to older patients. Nurses should collect all relevant data from the older patients such as their physical and mental state and their religious beliefs as well.
Dewar (2006) also suggests that older people may have difficulties in carrying out their activities of daily living (ADL) due to severe pain. It has been observed that in community settings, older people with severe pain feel a great necessity of assistance from the nurses to perform their ADLs. Older people suffering from severe pain also tend to have a loss of hunger and sleep. It is understood that the severe pain experienced by older people has a great impact on their physical performance. But there are other factors also that have an impact on the physical performance like the area of pain, the inception of the pain, the regularity of pain, and the prototype of pain. Like, a pain that is frequent but less severe can be compared to a pain that is very severe but is irregular. If the pain is being experienced in more parts of the body then the patient is bound to face more difficulties in performing his activities of daily living. Sometimes, it becomes important and necessary for older patients to agree to a change in their ADLs.
According to Manias (2011), older people are prone to old age-related diseases like arthritis, bone problems, and backache. It is also very frequent for older people to experience painful situations. Older people have the highest rate of surgery and pain during the surgery. Due to the deficiency of calcium in the bone of older people, the bones become frail and porous. Due to this problem, older people usually have bone fractures. This problem is usually found in people above the age of 65 years.
Al-Shaer et al. (2011) suggest that the approach of nurses towards older patients is also a governing and deciding factor for the execution of the pain management system. Also, the fallacies and perplexities surrounding the pain management system confuse the nurses. Another factor that affects the execution of proper pain management tools is the requisite education level of nurses and their experience in the profession. It is very crucial for nurses engaged in the treatment of pain in older people to have adequate experience in the intensive care units, treatment of tumors, and the emergency wards.
As described earlier, gauging and categorizing pain is the most crucial aspect of pain management. Even today, the researchers report paucity in pain detection. “In a study of postoperative pain management, it was found that elderly persons with cognitive impairment had more documented behavioral indicators of pain than those without, yet were prescribed fewer analgesics” (Frampton 2003).
Several scholars believe that older adults don’t express their pain verbally. They keep on tolerating their pain. Until recently, there had not been any serious efforts or studies on the topic of pain management in elderly persons. Considering the severity of the issue of pain in older adults, The BPS and the BGS issued some guidelines for managing pain in elderly persons. “The guidelines aim to make health professionals aware that the bio-physiological changes that come with aging, the build-up of co-morbidities and co-prescription of medication, frailty and psycho-social changes mean pain should be treated differently in older patients” (Pain Management Guidelines Launched 2013). Professor Pat Schofield believes that, “for whatever reason, older people do not always inform people when they are in pain, while health professionals do not always know how to treat pain when they do report it” (Pain Management Guidelines Launched 2013).
It has been observed and it has become a usual practice of the nurses to administer the basic medicines for older adults having pain. They are not concerned about the variations of pain or its intensity. In other words, the medications given to older adults having pain are never customized (Pain Management Guidelines Launched 2013).
Further, pain assessment in older adults becomes all the more difficult due to their other health issues and their compassion towards pain-relieving prescriptions. A variety of other problems like the patient’s viewpoint and attitude towards pain and pain-relieving prescriptions, nurses’ insufficient information and understanding of chronic pain, and certain professional hurdles intensify the complications and the role of nurses (McNamara et al. 2012). Since pain affects almost all aspects of human life – physical, mental, and spiritual – nurses must collect information on all such aspects. It is also important to know from the patient’s perspective about pain (Dewar 2006).
There have been several serious legal cases against nurses who have neglected to treat elderly patients having pain. “The existence of statutes of limitations and award caps for medical malpractice has contributed to recent charges against nurses for elder abuse in cases of pain under treatment in older patients” (Denny & Guido 2012). Certain guidelines clearly state the instances where adult abuse is committed. There may be various kinds of elderly abuse such as bodily abuse, overlook, or a lack of care that amounts to bodily harm, pain, or mental torture of older adults. Some scholars believe that incompetence in treating pain or under-treatment might also be categorized as elderly abuse. Earlier regulations about pain management suggested that there should be laws that allow the use of opioids in the treatment of pain. The regulations also suggested that the ‘professional codes of ethics and standards of practice’ should include providing pain relief as one of the necessities for nurses. “Although research has given little attention specifically to the inequities in pain care, three categories of barriers to effective treatment of pain in older adults have been identified and include patient, health-care provider, and health-care system barriers” (Denny & Guido 2012).
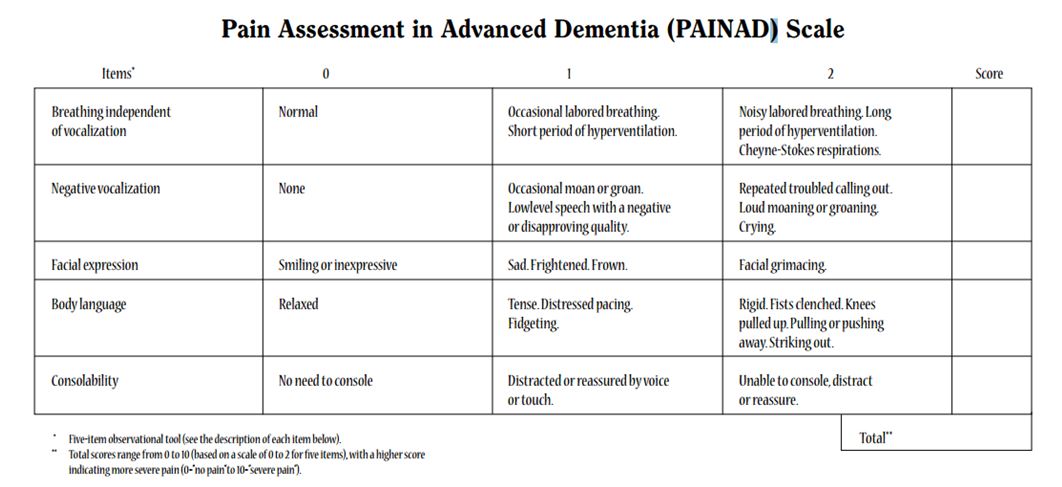
Horgas et al. (2012) ventured a little further in studying pain management in older patients. They researched assessing pain in elderly patients who were suffering from dementia. According to them, the usual pain assessment tools do not yield when dealing with people with dementia. A scale that measures pain in people with dementia is in Appendix 9.
Talking of the hurdles in pain management in elderly patients, Hanks-Bell et al. (2004) believe that the main hurdles transpire due to the patients themselves, the health care agencies, or the community. These three categories have different opinions and beliefs when it comes to the interpretation of pain and its treatment. The table in Appendix 10 depicts the various hurdles in pain management in elderly patients.
Dewar (2006) claims that the unwillingness of elderly patients in complaining about their pain is a great hindrance in offering pain-relieving treatment. Such patients are afraid of getting old because they feel that old age means lots of pain and suffering. They are afraid of taking medicines and are hesitant to undergo other treatments. They feel that once the pain has attacked them, they might not get well. They also believe that reporting their pain would result in the health care professional neglecting them and as a result, whatever social contact and support that they have from the society will also be finished. On the contrary, some researchers believe that reporting pain is often felt easier by elderly patients rather than to report other traits such as solitude, boredom, and inability to do their daily activities.
It is also possible that different people from different cultures might refer to pain differently, using different words such as ache, soreness, sting, twinge, etc. So nurses should carry out a thorough pain assessment round with the patient (Dewar 2006).
Harper et al. (2007) stress more on the cultural aspect. According to them, nurses must consider the culture of patients during the post-operative stage. By doing so, the nurses can typecast patients of varied cultures and deliver services accordingly. Harper et al. (2007) state the example of elderly patients from military backgrounds while discussing enduring behavior during the post-operative stage. If a patient endures his/her pain then it becomes easier for nurses to evaluate the exact pain.
Quantitative analysis
During the past couple of years, there has been a major increase in the percentage of older adults in the population of the world. The United Kingdom is no exception, where the population is becoming aged. There was an increase of 20% in the population of people with 65 and more years of age, from 1985 to 2010. The population of people with 85 and more years of age became twofold during this period. There was a drop of 2% in the percentage of children less than 16 years of age during the same period (UK National Statistics 2013). Pain is a very commonly experienced ailment by older adults. Persistent pain, like chronic pain, affects more than 50% of older adults residing in the community and 80% of those residing in nursing homes (Ferrell et al. 1995). Older adults are more prone to chronic pain than the younger population. The pain experienced by older adults is persistent and is of normal to a rigorous intensity that may continue for several years (Brattberg et al. 1996).
The figures suggested by Dewar (2006) seem to be astonishing. According to him among the people who are above 65 years of age, there is at least 27 percent to 51 percent of people who are suffering from severe pain. The occurrence of severe pain in people who are above 85 years of age is yet more astounding. Reports suggest that at least 70% of people in this age range suffer from severe pain. Well, the figures seem to be really on the higher side even when we hear that there are lots of programs being carried out for the elderly people.
Manias et al. (2011), concerning previous works, suggest that almost 45% to 80% of the people (above 65 years of age) who suffer from severe pain do not receive proper medical attention. It is very strange to notice that sometimes such patients are even subjected to over-treatment.
Flahaerty (2003) found that 25 to 45 percent of elderly people suffer from chronic pain. Out of these, 45 to 85 percent of people complained of not being treated for their chronic pain.
Manias et al. (2011) conducted a survey in which nurses working in the geriatric evaluation and management unit of two hospitals were requested to participate. The results of the survey show that “At post-intervention, the mean SF-MPQ score at rest was 12.91 in the control ward compared with 9.51 in the intervention ward with a mean difference estimate of 3.40 (95% CI 0.17, 6.63)” (Manias et al. 2011).
Flaherty et al. (2012) claim that almost half of the surveyed elderly people agreed they suffered from pain in the previous month. According to them, “Persistent pain has been associated with functional impairment, falls, slow rehabilitation, depression, anxiety, decreased socialization, sleep disturbance, as well as increased healthcare utilization and costs” (Flaherty et al., 2012).
The Importance of Being Culturally Congruent
Culture is a typical kind of characteristic of people having many things in common such as speech, communication style, creed, faith, beliefs, food habits, social traditions, music, arts, etc. These aspects keep on changing with time. Now, what is culturally congruent care? It is the care that is provided by a compassionate, proficient, and culturally perceptive nurse or any other health care provider (Jeffreys 2010). In other words, when the cultural aspects of patients are considered and there is no bias in the treatment, then it is culturally congruent care.
Due to the rapid expansions of multinational companies, there has been an incessant increase in the quantum of migrating populations. The changes in the characteristics of such populations, the unstable fertility rates, and advancements in science and technology have resulted in an overall cultural revolution. Owing to such developments, there has been a need for change in nursing practices worldwide. The current requirement about pain is that the nurses should be taught how to tackle culturally diverse patients. It is the need of the hour that the concept of culture is included in nursing education and the implementation of management skills.
But it is not as easy as it seems, to understand the different cultures and offer treatment accordingly. On the contrary, “A cultural assessment of a patient is crucial to discovering cultural beliefs and practices and providing culturally congruent care that is tailored to the individual client” (Alamah 2011). It’s a huge task to get details from every patient about his/her culture. “Lack of consensus between nurses and patients may result from their different cultural backgrounds and attitudes to pain” (Harper et al. 2007).
Moreover, there are many cultures around the world where the health and sickness of an individual are associated with God and Saints (Baca 1969). “Culture and ethnicity create a unique pattern of beliefs and perceptions as to what ‘health’ or ‘illness’ actually means” (Anderson 2003). Also, there are certain medicines that the nurses might not have heard of before. But it becomes improper to bluntly neglect all such things when such a patient comes for health care assistance. In such circumstances, it becomes very difficult to have the same health care approach for the patients.
Language is yet another very critical problem. “An inability to communicate with a healthcare provider not only creates a barrier to accessing health care but also undermines trust in the quality of medical care received and decreases the likelihood of appropriate follow-up” (Anderson 2003).
As such every one of us is entitled to have health care that corresponds with culture. Observations from some studies indicate that culturally motivated health care and the performance of health care are interrelated (Jeffreys 2010). This means if a health care institution adheres to culturally congruent health care for all its patients then the overall performance of that institution will be appreciable, and vice versa. The astounding number of legal cases claiming improper health care suggests that the legal implications can be serious. The nurses are not only bound morally but legally as well to provide better health care indifferent to culture.
If the moral values are considered by nurses and other health care providers, most of the problems relating to culturally congruent health care will automatically be resolved. If this may be the case, then they will “come simply to perceive the morally relevant aspects of situations and so to adopt a moral perspective on them without deliberation (unless the situation is unusually confusing or unclear)” (Huddle 2005). This is a very practical way of overcoming the problem of culture in nursing. If in any situation the nurses consider moral values, there is no way that they will disregard the problems being faced by patients of different cultures.
Pain Assessment Tools
It was on the 1st of January, 2001, that it was made mandatory for all the health care institutions to follow the pain management regulations while assessing and managing the pain of patients (Facts about pain management 2013, para. 2). Some of the main features of such standards are discussed further. Organizations have to uphold the rights of patients to have a proper review of their pain. The concerned health care professional should do proper screening of the patients’ pain at the time of preliminary check-ups. If the patients complain of pain during the treatment, the concerned health care professional has to redo the screening for pain. Organizations are required to instruct their health care professionals to impart knowledge about pain management to patients and their families.
As per the regulations mentioned in the standards of pain management, certain steps have to be followed while assessing pain in patients. The health care professionals have to inquire from the patients about the intensity of pain, the actual area where the patient is experiencing pain, and the factors that increase the pain. The patients have also to be inquired about any previous pain assessment that they might have done. The health care professional should know from their patients about any previous health problems that might have an impact on the proposed treatment. The history of the patients’ health is also a crucial factor to know. The health care professionals have to inquire from the patient if the pain has led to any mental or social effects. The patients should be asked about the impact of the pain on their daily routine. It is also very important to have an idea about the hopes that the patients and their relatives have from the proposed pain management. An actual assessment of pain should be done to ascertain the source. The patients should be given an assurance that their pain is being taken care of. The patients should be diagnosed for pain; such diagnosis should not lead to an argument with the patients about their pain but on the contrary, it should complement the patients’ assessment. The patients should be advised to inform any transformation (Perron 2001).
The nurses have to face several hurdles, while assessing their patients’ pain, despite taking great precautions and care. Some of the factors that might hamper the assessment process are restlessness of the patient, unconsciousness of the patient, administration of sedatives, etc. (Kompanje et al., 2008). The nurses should follow certain steps before using any tool for pain assessment. The patient should be requested for a self-report. Self-reporting is supposedly the best way to assess pain as pain is considered to be subjective. Moreover, once any tools are started to be used, there might be certain barriers that may hamper self-reporting. The previous history of pain should be known from the patient. The patient’s behavior should be noticed. Facial expressions express a lot about the pain. The body language of the patient also allows the nurses to have an idea about pain. The patient should be administered an appropriate analgesic and the required time should be allowed to pass. The patient’s reaction to the analgesic should be closely monitored. If the patient experiences comfort, it means that the main cause is pain. In such cases, subsequent analgesic medication may be continued for better results. In the case of critically ill patients, the statements of parents, guardians, and/or other family members play a significant role in assessing the patient’s pain. So in such cases, the statements should be given due importance.
Tools for pain assessment
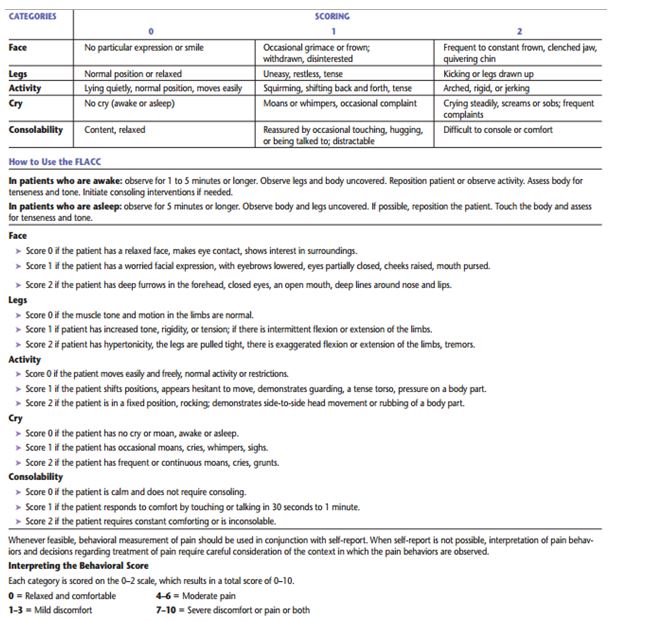
FLACC tool
This particular tool shows best results when used for children from two to seven years of age. The scoring is done from zero to ten. The observer assesses and mentions the scores accordingly. A score of zero means there is no pain, and a score of ten signifies maximum pain. The scoring from zero to ten depends on the intensity of the pain (Royal College of Nursing 2009). The chart in Appendix 4 depicts a detailed description of the FLACC tool.
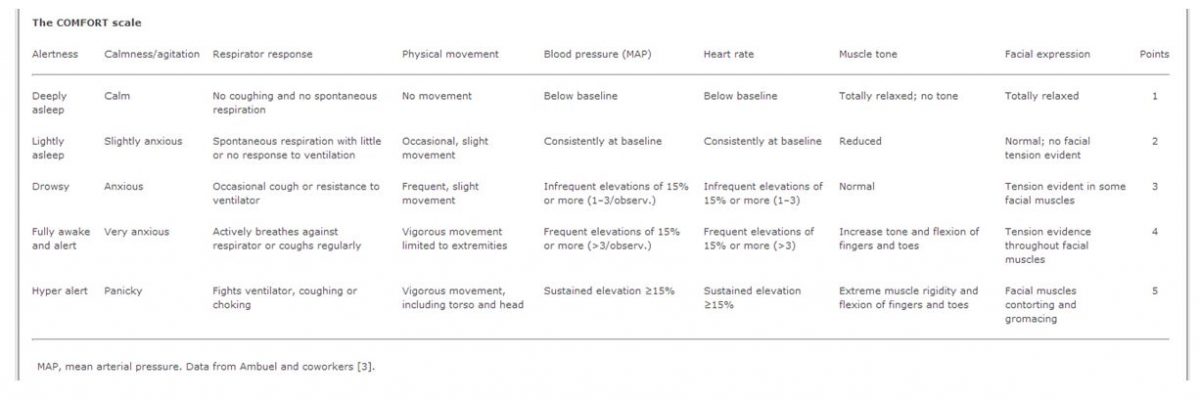
COMFORT scale
The COMFORT scale relates to the behavior of patients. The resultant score varies from eight to forty. Higher scoring means higher levels of uneasiness. The eight behavioral characteristics that are assessed are – Alertness, agitation, respiratory response, physical movements, blood pressure, heart rate, muscle tone, and facial tension (Royal College of Nursing 2009).
This particular scale is considered to be all-inclusive because it allows the observer to assess the behavioral aspects as well as the changes in the vital signs. The scale was originally meant for children but it has proved to be useful in cases where even adults who are under intensive care and cannot self-report their pain. Despite its effectiveness, there have been observed some drawbacks when the comfort scale is used simultaneously with VAS pain. “The variations in correlation between ‘before VAS’ and COMFORT compared to ‘VAS after’ with the COMFORT, might be ascribed to the 2-min observation period of the child” (The Comfort Behaviour Scale – The Thesis, 2013). The chart in Appendix 5 depicts the details of the scoring guidelines.
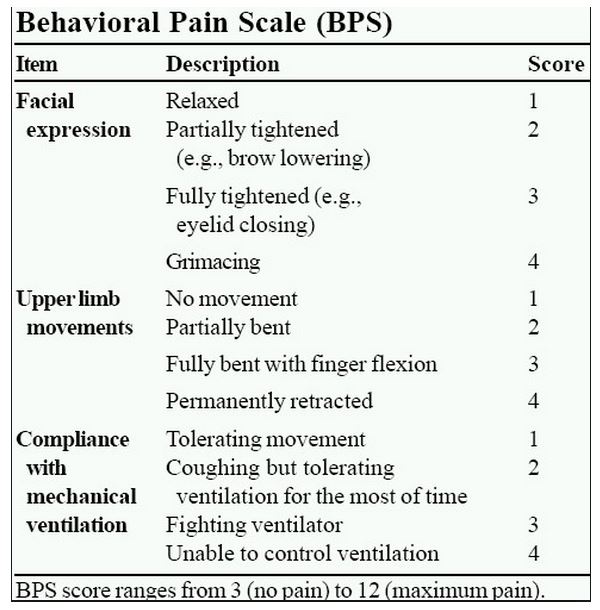
Behavioral Pain Scale (BPS)
In BPS, the behavioral aspects that are observed are Facial expression, upper limb movements, and compliance with mechanical ventilation. This particular scale can be used for patients under sedation. The increased scoring signifies higher levels of pain and agony (Wells et al., 2013).
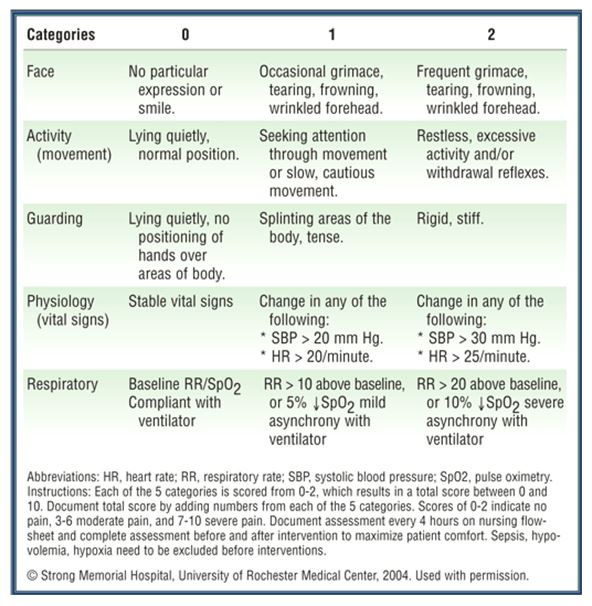
Critical Care Pain Observation Tool (CPOT)
The CPOT tool considers four aspects to assess pain. These are Facial expression, body movements, muscle tension, and compliance with the ventilator. These behaviors are rated from zero to two, where a zero rating signifies no pain and as the rating increases, the intensity of pain also increases (Gélinas, 2006).
According to Imperial College Healthcare, “Different types of outcome measures may also be used to capture adequately the complexity of the pain experience and how that experience may be modified by different pain management interventions” (Imperial College Healthcare 2012). Healthcare professionals should observe the following questions that need to be answered while interacting with their patients suffering from pain: “What is the date and duration of onset? Has there been pre-existing pain before this episode? Where is the pain located? How is it described? What makes it worse or better? Is it constant or intermittent?” (Imperial College Healthcare 2012).
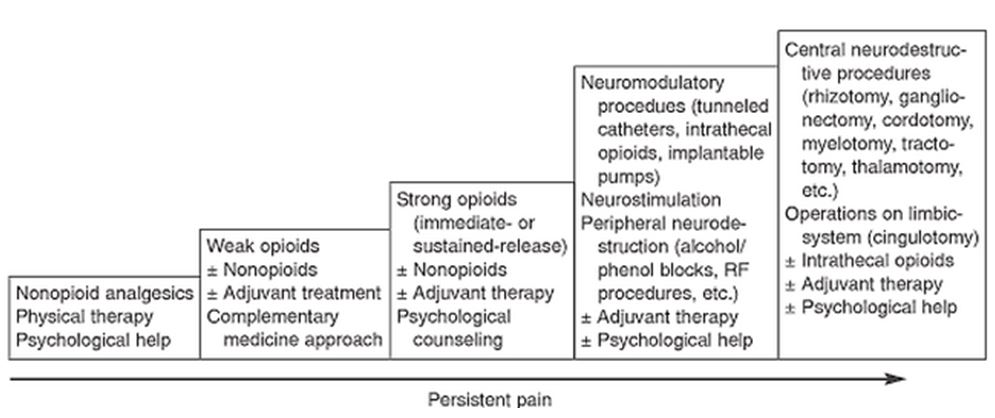
The World Health Organization has worked out an ‘analgesic ladder’ that was originally meant for cancer patients. But it may also be referred in cases of patients suffering from chronic pain. The following are the five steps of the ladder:
- Step 1: Non–opioids
- Step 2: Weak – opioids
- Step 3: strong – opioids
- Step 4: SC / IV / IM opioids
- Step 5: Epidural opioids (Slavin et al., 2004) Refer to Appendix 8.
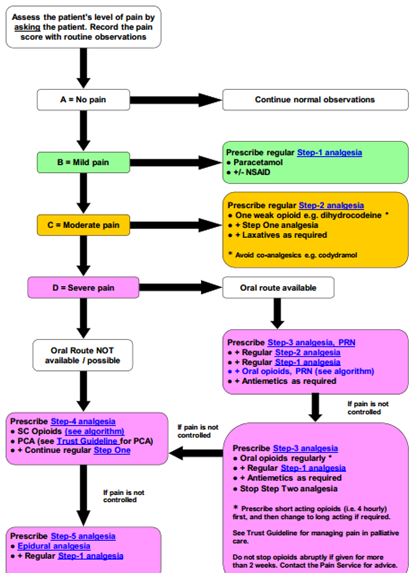
The steps don’t mean that the health care professionals have to start from the first step. Analgesic doses may be administered according to the severity of the pain. The chart in Appendix 7 depicts an algorithm for pain management. It will be beneficial for those in the pain management business.
Conclusion
Pain is considered to be one of the most commonly found illnesses in human beings. Various steps and initiations have been taken by various governments and charity organizations to help people in countering such a menace. But still there remains a lot to be done in this field. The main focus should be on improving the nursing profession. Apart from the educational point of view, the shortage of well-qualified nurses is also a matter of grave concern.
Several decades of research have shown that equity in health and healthcare is of immense societal importance given its ethical and social justice implications (Kim & Fredriksen 2012), and it’s the core philosophical underpinning to service the healthcare needs of all populations in a socially and culturally appropriate way (Neville & Henrickson 2006).
“Nursing management is as much a nursing specialty as any specialty and requires specialty leadership skills. Mentorship/leadership from senior leaders smoothens the transition from clinical roles to formal leadership roles” (Sanford, 2013).
In addition to being knowledgeable, it is equally important to be aware of the legalities involved in the nursing profession. At the federal and state levels, the decisions of legislative bodies are playing a pivotal role to keep an impact on the health care industry. The transition in delivery of health care methods along with the political system and involvement of the politicians in the development of health care and implementation of new policies has led the nursing leaders to act as an influencing factor in the entire procedure. “This type of advocacy necessitates stepping beyond their practice setting and into the less familiar world of policy and politics, a world in which many nurses do not feel prepared to operate effectively” (Political Aspects of Nursing, 2013).
Because nurses work under immense pressure, it is very crucial on the part of health care facilities to keep on motivating them. The nurses should be kept professionally satisfied because there are chances of good nurses being attracted by other health care facilities for higher wages. Nurses should be regularly asked for their feedback about patient care, the working environment, the working hours, etc. They should be allowed to have open discussions on matters concerning their profession. “Ask them what they think about the most frequent nursing challenges they deal with at meetings, through suggestion boxes, with monthly or quarterly surveys and in performance reviews” (Cardenas, 2013). This will make the nurses understand that their existence matters.
Considering all the aforementioned aspects, the nurses must be imparted proper training that covers ethical, professional, and legal aspects. Only then medical professionals can come up with the expectations of patients of all genders and ages.
“Man is a social animal” – according to this quote, we should be happy within our society. On the contrary, the researcher noticed that the elderly living in the nursing homes were more happy and content than those living in the community. The older adults from the nursing homes suggested that they were being taken care of very well. Their pain experience was decreasing day by day and they were having relief from the treatment being given to them by the nurses. They were also happy with the approach of the nurses. Regular visit by the doctors was also a point appreciated by many. On the contrary, the older adults living in the community were not happy with the way they were being treated by the hospital professionals. The researcher noticed that the older adults living in the community were being neglected by the community as well. Why is it that we can’t take care of our parents and elders? A man indeed takes care of his children single-handedly but when he gets old, none of the children can take care of their father. What a pity! But that’s a different topic altogether. We are concerned with the nursing aspect only. The researcher thinks that the reason why the older adults in the nursing homes were more content is probably related to the monetary aspect. Hospitals and clinics earn more from the in-house patients – so more care is given to them.
When the nurses were questioned in this regard, they argued that the older adults who were at the nursing homes were under observation 24 hours a day and as such any minor complication could be noticed and appropriate treatment could be administered. But in the case of older adults living in the community, it was not possible because they visited once in a while and wanted to have medicine for a longer period. So it was not possible to ascertain the results of the treatment. It was only after the older adults visit again that their condition could be gauged. So it was wrong to blame the nurses.
This paper has been a great learning experience for me. It is very important to be aware of the theoretical aspects along with the practical ones. There may be times when having theoretical knowledge might bail you out of critical situations. On completing this paper, I have acquired such theoretical aspects that will be helpful to me in my future pain assessment issues. I also plan to educate my colleagues on the pain assessment requirements. Together, we will ensure that we apply the pain management tools efficiently so that our patients feel relief and are satisfied. I believe that by this knowledge, I will be able to climb the ladder of success in my profession.
References
Al-Shaer, D, Hill, PD & Anderson, MA 2011, ‘Nurses’ knowledge and attitudes regarding pain assessment and intervention’, Medsurg Nursing, vol. 20, no. 1, pp. 7-11.
Alamah, W 2011, ‘The Use of Culture Care Theory with Syrian Muslims in the Mid-western United States’, Online Journal of Cultural Competence in Nursing and Healthcare, vol. 1, no. 3, pp. 1-12, viewed 24 April 2013.
Anderson, M 2003, ‘Culturally Competent Healthcare Systems: A Systematic Review’, American Journal of Preventive Medicine, vol. 24 no. 3S pp. 68-79.
Attar, D, Elhayany, A, Grinstein-Cohen, O, Pilpel, D, & Sarid, O. 2009, ‘Improvements and difficulties in postoperative pain management, Orthopaedic Nursing, vol. 28, no. 5, pp. 232-239.
Baca, J 1969, ‘Some Health Beliefs of the Spanish Speaking’, The American Journal of Nursing, vol. 69, no. 10, pp. 2172-2176.
Brattberg, Parker, MG & Thorslund, M 1996, ‘The prevalence of pain among the oldest old in Sweden’, Pain, vol. 67, pp. 29-34.
Breau, LM, Camfield, CS, McGrath, P, & Finley, A. 2003, ‘The incidence of pain in children with severe cognitive impairments’, Archive of Paediatric Adolescent Medicine, vol. 157, pp. 1219-1226.
Cardenas, H 2013, Strategies to motivate staff nurses. Web.
Chronic Pain Policy Coalition 2007, Our campaign. Web.
Chronic pain discussed in the House of Lords, 2009. Web.
Denny, LD & Guido, GW 2012, ‘Undertreatment of pain in older adults: An application of beneficence’, Nursing Ethics, vol. 19, no. 6, pp. 800-809.
Department of Health 2001, National Service Framework for older people. Stationery Office HMSO London.
Dewar, 2006, ‘Assessment and management of chronic pain in the older person living in the community, Australian Journal of Advanced Nursing, vol. 24, no. 1, pp. 33-38.
Facts about pain management 2013. Web.
Ferrell, BA, Ferrell, BR & Rivera, L 1995, ‘Pain in cognitively impaired nursing home patients’, J Pain Sympt Manage, vol. 10, no. 59, pp. 1-8.
Flaherty, E 2012, Pain assessment for older adults. Web.
Flahaerty, E 2003, Assessing pain in older adults. Web.
Frampton, M 2003, ‘Experience assessment and management of pain in people with dementia’, Age and Ageing, vol. 32, no. 3, pp. 248-251.
Gélinas, C 2006, The Critical-Care pain observation tool (CPOT). Web.
Gibson, S 2002, Pain in older persons, Presentation at the World Pain Congress, San Diego, IASP.
Hanks-Bell, M, Halvey, K & Paice, JA 2004, ‘Pain assessment and management in aging’, The Online Journal of Issues in Nursing, vol. 9, no. 3.
Harper, P, Ersser, S & Gobbi, M 2007, ‘How military nurses rationalize their postoperative pain assessment decisions’, Jan Original Research, pp. 601-611.
Horgas, AL 2012, ‘Assessing pain in older adults with dementia’, American Medical Directors Association, vol. 4, no. 1, pp. 9-15.
Huddle, T 2005, ‘Teaching Professionalism: Is Medical Morality a Competency?’, Academic Medicine, vol. 80, no. 10, pp. 885-891.
Imperial College Healthcare 2012, pain management guidelines for adult patients with acute or chronic pain. Web.
Jeffreys, M 2010, Teaching Cultural Competence in Nursing and Health Care: 2nd Edition, Springer Publishing Company, New York.
Kim, HJ & Fredriksen, KI 2012, ‘Hispanic lesbians and bisexual women at heightened risk or health disparities’, American Journal of Public Health, vol. 102, no. 1, pp. e9-e15.
Koes, B, Tulder, MW & Thomas, S 2006, ‘Diagnosis and treatment of low back pain’, British Medical Journal, vol. 332, pp. 1430-1434.
Kompanje, EJO, Hoven, B & Bakker, J 2008, ‘Anticipation of distress after discontinuation of mechanical ventilation in the ICU at the end of life’, Intensive Care Med, vol. 34, no. 9, pp. 1593-1599.
Lui, L, So, W & Fong, D 2007, ‘Knowledge and attitudes regarding pain management among nurses in Hong Kong medical units’, Journal of Clinical Nursing, pp. 2014-2021. Web.
Manias, E, Gibson, SJ & Finch S 2011, ‘Testing an educational nursing intervention for pain assessment and management in older people, Pain Medicine, vol. 9, pp. 1199-1215.
Maya, J, Ranjit, S & Manias, E 2010, ‘Pain assessment and management practices in children following of the lower limb’, Journal of Clinical Nursing, vol. 19, pp. 118-128.
McNamara, MC, Harmon, D & Saunders, J 2012, ‘Effect of education on knowledge, skills, and attitudes around pain’, British Journal of Nursing, vol. 21, no. 16, pp. 958-963.
Melding, PS 1991, ‘Pain Management in Older adults’, Journal of American Geriatrics Society, vol. 46, pp. 119-121.
Munoz, C & Luckman, J 2005, Transcultural communication in nursing (2nd edition), Delmar Learning, New York.
Neville, S & Henrickson, M 2006, ‘Perceptions of lesbian, gay and bisexual people of primary healthcare services, Journal of Advanced Nursing, vol. 55, no. 4, pp. 407-415.
Oberlander, TF & O’Donnell, ME 2001, ‘Beliefs about pain among professionals working with children with significant neurologic impairment’, Developmental Medicine & Child Neurology, vol. 43, pp. 138-140.
Pain Management Guidelines Launched 2013. Web.
Perron, V 2001, ‘Assessment and management of pain in palliative care patients’, Cancer Control, vol. 8, no. 1, pp. 15-24.
Political Aspects of Nursing – Advocating for Healthcare Policies 2013. Web.
Rogers, E 2010, Participatory action research in learning commons design planning. Web.
Royal College of GPs announces chronic pain as clinical priority 2011. Web.
Royal College of Nursing 2009, The recognition and assessment of acute pain in children. Web.
Sanford, K 2013, Overview of nursing leadership. Web.
Slavin, KV, Tesoro, EP & Mucksavage, JJ 2004, ‘The treatment of cancer pain’, Drugs Today, vol. 40, no. 3, p. 235.
Stallard, P, Williams, L, Velleman, R, Lenton, S, & McGrath, PJ. 2002, ‘Intervening factors in caregivers’ assessments of pain in non-communicating children, Developmental Medicine & Child Neurology, vol. 44, pp. 212-214.
The British Pain Society 2007, Recommended guidelines for Pain Management Programmes for adults. Web.
The Comfort Behaviour Scale – The Thesis 2013. Web.
UK National Statistics 2013, a Topic guide to Older people. Web.
Wells, N, Pasero, C & McCaffery, M 2013, ‘Improving the quality of care through pain assessment and management, Patient Safety and Quality: An Evidence-Based Handbook for Nurses, vol. 1, pp. 469-497.
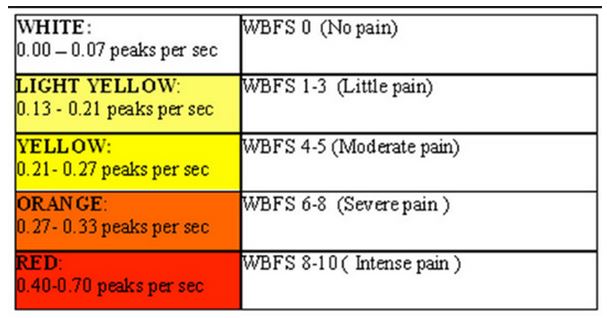
Appendix 1
Appendix 2
Pain assessment tool for elderly patients
Appendix 3
Pain assessment tool for children
Appendix 4
FLACC Behavioural Pain Assessment Scale
Appendix 5
COMFORT Sedation Scale
Appendix 6
Behavioral Pain Scale (BPS). Source. Web.
Appendix 7
Algorithm for pain management
Appendix 8
Five-step ladder for cancer pain. Source: Web.
Appendix 9
Appendix 10
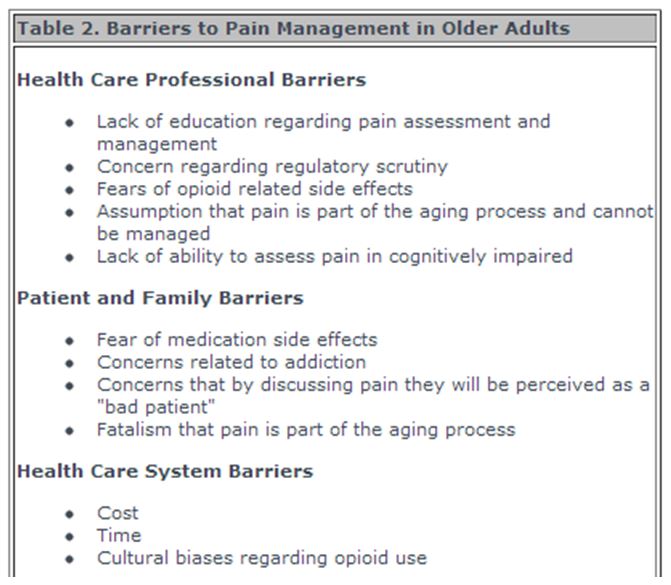
Source: Web.