Introduction
Mycobacterium Tuberculosis or M. tb is a pathogen that causes tuberculosis (TB). It was first discovered a century ago by Robert Koch. TB continues to affect thousands of people in the United States, and there is a plethora of multidrug-resistant TB. M. tb differs from other bacteria in its pathogen properties, nor does it possess the typical virulence factors. This paper will describe M. tb, its morphology, virulence factors, immune response, and other relevant information.
Description of the Microorganism
This is a bacterial microorganism with a unique structure, mainly the coating of M. tb is made of mycolic acid, which causes the coating to be waxy and requires the use of special stain agents, It is an obligate aerobe, which means that the bacteria need oxygen to grow (Chai, Zhang, & Liu, 2018). Compared to other bacteria, M. tb has a relatively slow division process, and it requires from eighteen to twenty-four hours to divide. In terms of morphology, M. tb is a nonmotile bacterium, characterized by large size and rod shape (Chai, Zhang, & Liu, 2018). Typically, the size of an M. tb bacteria is approximately two to four micrometers in length by the width of 0.2 to 0.5 micrometers. The specifics of this microorganism require one to use fluorescent stains instead of Gram staining, as the latter does not affect M. tb due to its impervious coating. The type of microscope one can use to view M. tb is the one with a 100X microscope objective (Chai, Zhang, & Liu, 2018). This pathogen impacts the respiratory system of mammals.
Virulence Factors
Virulence factors are the properties of a microorganism, mainly their ability to produce molecules that will help them colonize a host. Therefore, virulence is the ability of a pathogen to cause disease, which in the case of M. tb is TB (Echeverria-Valencia, Flores-Villalva, and Espitia, 2018). M. tb’s virulence factors depend on the ability of M. tb to evade macrophages. According to Echeverria-Valencia, Flores-Villalva, and Espitia (2018), M. tb does not have the usual virulence factors, and M. tb’s virulence gene codifies enzymes and factors that are responsible for the pathological damage to the host’s health. Hence, M. tb’s virulence factors differ from those of other bacteria, which is a result of an adaptation to the immune response.
Moreover, Echeverria-Valencia, Flores-Villalva, and Espitia (2018) states that M. tb’s virulence is also linked and measured through the transmission. The main factors of virulence include the ability to invade a host and survive the immune system’s response, the damage caused to the hosts’ lungs, and the capacity to be transmitted to another host (Echeverria-Valencia, Flores-Villalva, and Espitia, 2018). When M. tb affects a human host, the alveolar macrophages are most commonly affected by this bacteria. The immune system receives inflammatory signals, causing increased production of additional macrophages and monocytes, and typically, the two become infected as well. The main danger of M. tb is the fact that “the bacteria exploit the host inflammatory signals to spread to other individuals” (Echeverria-Valencia, Flores-Villalva, and Espitia, 2018, p. 1). The cause of this is the adaptation to the immune response. M. tb causes granulomas, which is an attempt of the immune system to protect the host from inflammation.
The specifics of M. tb’s viral factors make it especially dangerous for humans. It should be noted that M. tb can survive some disinfectants and survive dry environments for several weeks. Moreover, the lipids in M. tb, for instance, mycolic acid is perceived to be the virulence factor that allows the bacteria to withstand dry environments, or desiccation (Chai, Zhang, & Liu, 2018). M. tb can be transmitted from one person to another through air droplets. Therefore, virulence factors affect the host are unique when compared to other bacteria. M. tb’s virulence factors affect the host by causing inflammation, production of macrophages, and monocytes that also become infected.
Immunity
A human’s immune system has a defense mechanism against this pathogen. According to Chai, Zhang, and Liu (2018), M. tb bacteria developed highly adaptable structures to avoid the innate and adaptive immune system response, which means that even an otherwise healthy host is not protected from developing TB. When M. tb enters the lungs, the immune response causes the formation of granulomas, the primary purpose of which is to contain the bacteria and reduce lung damage. Upon inhalation, M. tb encounters epithelial cells and phagocytes, which can abort the infection’s development. Specific barriers or cells include “neutrophils, dendritic cells (DCs), natural killer cells (NK), mast cell” which are a part of the innate immune system’s response (De Martino et al., 2019, p. 350). M. tb induces a specific immune response, more specifically, it triggers both innate and adaptive immune responses.
Infectious Disease Information
If M. tb successfully overcomes the immune response of the host, it develops into an infection. Although M. tb is mainly linked to TB, it can also cause other illnesses – “pulmonary complications, autoimmune diseases, and metabolic syndromes” (Chai, Zhang, & Liu, 2018, p. 305). TB typically affects the respiratory system and lung tissue, where granulomas are formatted to protect the body from the infection. Lung tubules are a characteristic of chronic TB, which are nodules in a host’s lungs. TB can be either chronic or latent, and a person with latent TB will not infect others. According to Chai, Zhang, and Liu (2018), “the etiological agent of tuberculosis (TB), is an extremely successful pathogen that adapts to survive within the host” (p. 158). It is an opportunistic pathogen since it causes severe damage to the host’s respiratory system if the immune system is compromised, and it usually can be found in the hosts’ lungs.
Epidemiology
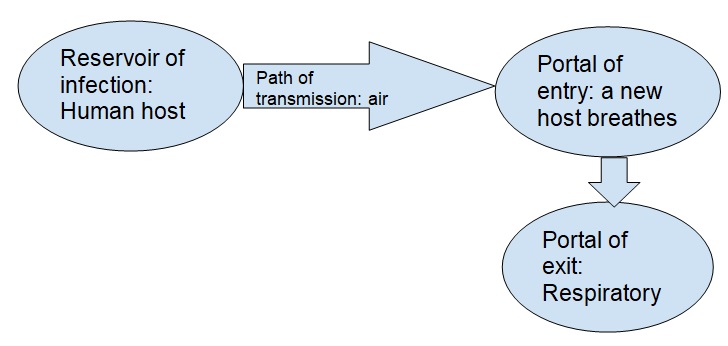
As displayed in Diagram 1, M. tb is transmitted during human to human contact. The reservoir is, therefore, another person, who can transmit the bacteria y coughing or sneezing. The portal of entry is the potential hosts’ respiratory system, and it is the portal of exit as well. It is an airborne bacteria meaning that it can be transmitted through air from one human host to another.
Prevention
Currently, Bacillus Calmette-Guérin (BCG) vaccine is used to prevent the development of TB caused by M. tb. In the United States, it is not administered to children because it does not adequately protect individuals from TB. Risk-groups are people residing in countries where TB is typical or to healthcare workers in contact with a large number of patients with TB. BCG is a live bacteria type of vaccine, which means that its mechanism of action is based on exposing an individual to a small number of bacteria (Pranger et al., 2019). As a result of the immune system’s response, a person should develop immunity to TB.
Treatment
Chemotherapeutic agents recommended for treating TB are isoniazid and rifampin. According to Pranger et al., (2019), the tuberculosis-specific chemotherapy includes two stages, at first, the patient receives multiple drugs. Isoniazid kills the majority of bacteria, though the mechanism of inhibiting the formation of the mycobacterial cell wall (Pranger et al., 2019). Rifampin affects the DNA-dependant RAN by the binding polymerase. These agents are effective against M. tb because they block the bacteria’s ability to survive (Pranger et al., 2019). However, there are drug-resistance forms of TB that cannot be treated with these medications.
Clinical Relevance
There are multi-drug resistant strains of M. tb, and their names are Beijing lineage, and they do not respond to the treatment scheme described above. This is a know health-associated pathogens, and people who have HIV are at the most risk of developing TB caused by this strain. To address the treatment of this strain, second-line therapy involving fluoroquinolones and aminoglycosides is used (Pranger et al., 2019). Since multi-drug resistant M. tb is present in the population, any individual who is immune-compromised may be affected.
Conclusion
Overall, this paper examined the M. tb bacteria, its properties, and the damage it caused to the host. M. tb causes TB, which severely affects the person’s respiratory system and damages the lungs. TB can be transmitted from human to human via droplets from coughing. The bacteria are airborne and can survive extreme conditions, making the risk of being infected even higher. The innate immune system of a person responds to the M. tb bacteria by releasing epithelial cells and phagocytes, that should stop the development of an infection. If TB infection develops, the immune system forms granulomas to contain the bacteria and minimize damage. Currently, the only vaccine against TB is a live bacteria type, meaning that an individual is exposed to a limited amount of M. tb to develop an immunity. There are several types of chemotherapeutic agents used to treat TB, and several agents are applied to treat the multi-drug resistant TB.
References
Chai, Q., Zhang, Y., & Liu, C. H. (2018). Mycobacterium tuberculosis: An adaptable pathogen associated with multiple human diseases. Frontiers in Cellular and Infection Microbiology, 8, 158. Web.
de Martino, M., Lodi, L., Galli, L., & Chiappini, E. (2019). Immune response to mycobacterium tuberculosis: A narrative review. Frontiers in Pediatrics, 7, 350. Web.
Echeverria-Valencia, G., Flores-Villalva, S., & Espitia, C. (2018). Virulence factors and pathogenicity of mycobacterium. Mycobacterium – Research And Development, 1-10. Web.
Pranger, A., van der Werf, T., Kosterink, J., & Alffenaar, J. (2019). The role of fluoroquinolones in the treatment of tuberculosis in 2019. Drugs, 79(2), 161-171. Web.