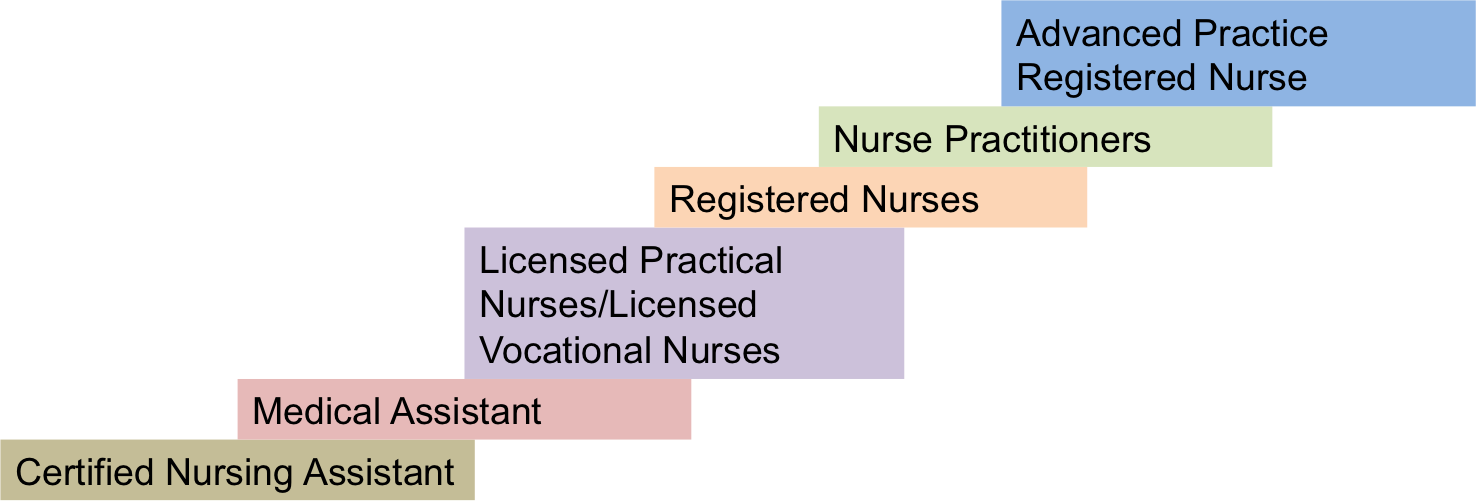
The turnover rate for high-level nurse practitioners, which is considerable, tends to be higher compared to their lower-level counterparts (Shi & Li, 2016). Newly recruited nurses usually exhibit an increased turnover rate due to a poor level of satisfaction with their jobs. Therefore, it can be stated that human resource management in medical communities may experience extraordinary challenges. To tackle this issue, authorities in the United States’ medical community have pioneered a nursing ladder management program. Proposed by Patricia Benner, the ladder was differentiated into five levels of professional experience: novice, advanced beginner, competent, proficient, and expert. Each level is associated with specific corresponding job responsibilities; the classification system provides health-care professionals with a basis for the further development of nursing ladder management (Shi & Li, 2016). Also, medical institutions implement clinical ladder types in three modes: clinical practice, nursing management, and nursing education (Shi & Li, 2016).
A nurse practitioner clinical ladder (NPCL) advancement program has been developed to provide recognition and awards for advanced nursing practice and to encourage nurse practitioner retention at New York University Hospitals Center. According to research conducted by Paplanus, Bartley-Daniele, and Mitra (2013), the NPCL advancement programs contribute to the enhancement of the professional development of nurses, increase performance evaluation effectiveness, and raise the rate of retention of nurses as well as their job satisfaction.
Motivation of Nurse Practitioners and Clinical Ladders in Different Facilities
Research on NPs’ opinions about clinical ladders led to Ginder Weido, BS, RRT-NPS and a clinical leader at Children’s Healthcare of Atlanta at Egleston, a facility in which a clinical ladder has been used for eleven years. Nurse practitioners move up the clinical ladder from the novice to the expert level, and each move up the ladder is accompanied by an 8% wage increase. Weido stated that the facility had had a beneficial experience incorporating the clinical ladder into operations despite the fact that not many nurses have reached the expert level.
Another motivational program for nurse practitioners can be found at the Cleveland Clinic Foundation, where the clinical ladder is made of two layers and is a voluntary process: If practitioners feel content with where they are as professionals, there is no requirement to climb the ladder. According to Donna Tanner, a clinical educator, the facility’s leadership team developed all possible tools for the staff within the department to reach the desired level of the ladder. The requirements for the levels of the ladder are as follows:
- Level I ($0.75-per-hour raise) requires practitioners to maintain their competencies, show rate of call-offs, and get training in a new sphere of expertise.
- Level II (additional $1.50-per-hour raise) requires practitioners to increase leadership involvement in their organizations along with total hours of volunteering, participate in research, become clinical specialists, and earn an advanced degree (“Advancing from within: The value of clinical ladders,” 2017).
The response from nurse practitioners to the incorporation of the clinical ladder is positive, which contributes to motivation for integrating the framework in other health-care facilities. Clinical ladder programs tend to lead to an improvement in practitioners’ satisfaction with their professional position, which points to the effectiveness of the approach. Another example of a clinical ladder can be seen at the University of California San Diego Medical Center, where the program has been in effect for eight years. The clinical ladder at the facility requires practitioners to meet eighteen competencies (steps); each step is accompanied by a 2.5% salary increase. According to the former director of the University of California San Diego Medical Center, Richard Ford, in the beginning, practitioners were predominantly driven to meet new competencies due to the generous salary increases; however, once they had started participating in the programs, the feeling of accomplishment proved to be the highest motivational factor.
Practice Improvement with Current Protocols of Clinical Ladders
The current protocols of clinical ladder incorporation at health-care facilities have shown a potential for improving nurse practitioners’ practice as well as satisfaction with their job. Clinical ladders offer the staff two main benefits that contribute to their practice improvement: recognition of their efforts and a break from mundane tasks that limit their effectiveness. The incorporation of clinical ladder protocols is a practice that gives NPs the opportunity to maintain their practice standards at the highest level possible while having the autonomy to participate in practice improvement procedures.
In addition, clinical ladders encourage management to take responsibility for the turnover of NPs, vacancy rates, and financial management, as well as the metrics associated with patient outcomes. It can also be stated that clinical ladders are tools for retraining experienced workers and improving the outcomes of patients. Helping nurses climb clinical ladders is not only a matter of practice improvement but also an instrument for saving organizational costs and aiming financial resources at important points of spending. Most clinical ladder programs are associated with financial incentives provided for nurse practitioners who either receive a base pay raise or a bonus payment that is awarded at the time of the advancement. It is essential for the management of a health-care facility to carefully weigh the costs paid to NPs against the expenses of paying to replace expert nurses. By doing so, the health-care institution can develop an effective program of career development that will encourage nurses to remain in their positions.
Charts for Clinical Ladders and Job Satisfaction
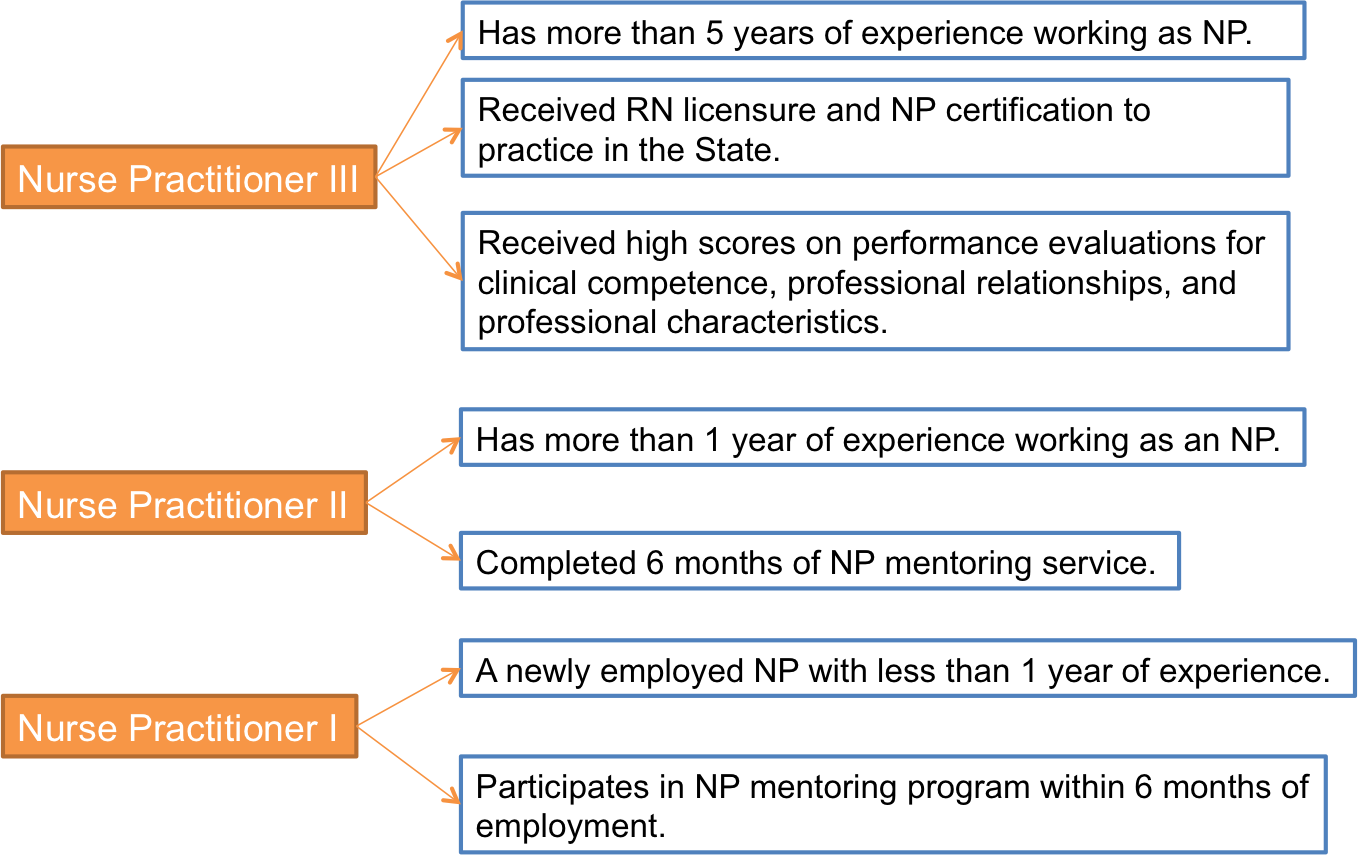
Nurse Practitioner Clinical Ladder
Job Satisfaction of Nurse Practitioners
Nursing Career Ladder
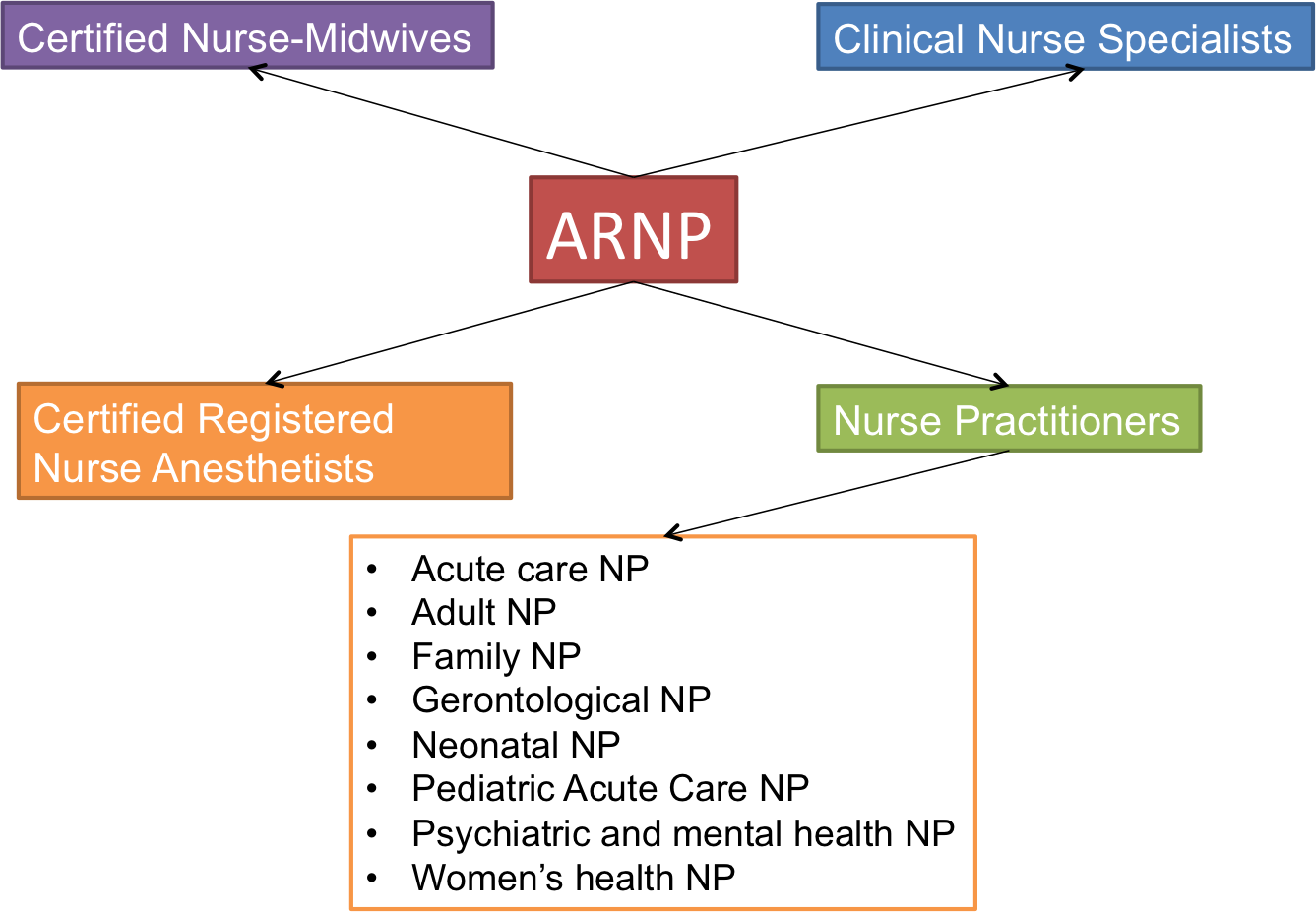
Advanced Practice Registered Nurse Careers
Analysis of Health-Care Facilities with Clinical Ladders
Based on the annotated bibliography of available studies, it can be asserted that health-care facilities that implement clinical ladders tend to show higher rates of employee satisfaction and can be more efficient in implementing change for achieving improved patient outcomes. For this brief analysis section, a review of the clinical ladder program (CLP) carried out in a community hospital based on a proposal by Lee (2015) was chosen. Due to the complete turnover of the executive management team in the facility, the majority of NPs resigned, significantly affecting patient outcomes. Moreover, the NP satisfaction survey showed a low level of staff motivation and lack of effort to maintain a high quality of care. Therefore, there was a strong need to develop a framework for increasing satisfaction and retention of personnel.
The clinical ladder program integrated into the facility comprised five clinical practice steps (novice, advanced beginner, competent, proficient, and expert). It was expected that upon the implementation of the program, the turnover rate of NPs would decrease, which would subsequently contribute to lowering costs associated with recruitment training and spending. The second potential outcome of program implementation was related to empowering NPs to take part in educational advancement lessons for improving their knowledge and skills. Both objectives were achieved. After the incorporation of CLP in the community hospital, NPs reported higher levels of job satisfaction and motivation measured with the help of surveys that involved Likert scales. The annual demographic data collected by the human resource department of the community hospital showed that after program implementation, nurses became empowered to pursue further educational development due to the rewards associated with climbing the clinical ladder.
Overall, the incorporation of CLP in a health-care setting is a beneficial practice that most facilities are currently implementing. However, it is crucial to mention that there is a gap in research associated with studying the impact of CLP for advanced registered nurse practitioners. For this reason, the current analysis of CLP benefits for the motivation and satisfaction of ARNPs is incomplete, which points to the need for future research on this subject matter.
Survey for Job Satisfaction and Clinical Requirements
The table below contains questions and response options for a survey designed to measure nurse practitioners’ job satisfaction and clinical requirements. The survey has been designed from the perspective of a nurse practitioner who has had some experience working in the field and is looking for procedures targeted at practice improvement in a health-care facility. The survey is based on Misener’s Nurse Practitioner Job Satisfaction Scale, which offers the following answer options:
Very Satisfied (V.S.) = 6 points; Satisfied (S.) = 5 points; Minimally Satisfied (M.S.) = 4 points; Minimally Dissatisfied (M.D.) = 3 points; Dissatisfied (D.) = 2 points; Very Dissatisfied (V.D.) = 1 point. The higher the score from answers given by NPs, the higher is their job satisfaction.
The survey presented above will allow for the assessment of nurse practitioners’ satisfaction with their job and discovery of potential areas for improvement. The survey can be distributed to NPs via print or electronic versions, based on their preference. The maximum score for the survey is 114 points, while 19 is the minimum. On average, scores ranging between 76 and 114 show NPs’ higher satisfaction with their job.
Development of Clinical Ladder Based on Research
Based on the research provided in the paper, it is proposed to develop a three-tier clinical ladder for advanced registered nurse practitioners (ARNP).
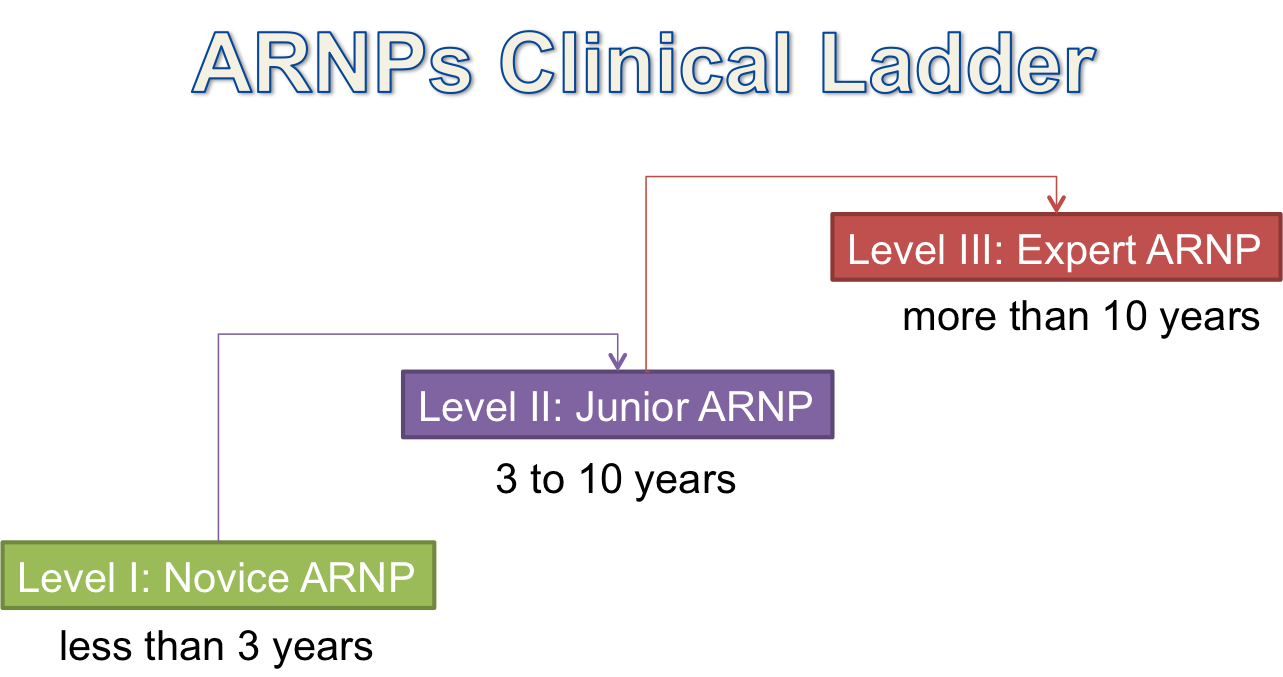
Level 1: Novice ARNP
- Less than three years of experience in the position.
- Practice: maintains necessary certifications for successful performance; reviews current clinical processes to implement required changes for improving patient outcomes.
- Clinical education: participates in staff education; is involved in educational resource development.
- Professional contribution: participates in research projects and attends professional conferences.
- Professional leadership: is a member of a unit committee and a professional specialty organization.
- Community service: participates in community outreach.
Level II: Junior ARNP
- From three to ten years of experience.
- Practice: plays a leading role in certification and quality improvement projects; seeks further certifications for improving patient outcomes.
- Education: mentors staff; is a preceptor of knowledge; develops staff education; provides lectures on enhanced patient care.
- Contribution: plays a leading role in research; plans institutional meetings.
- Leadership: is a member (or leader) of hospital committee; is a leader of a division.
Community service: plays a leading role in community outreach.
Level III: Expert ARNP
- Ten and more years of experience.
- Practice: plays a leading role in review and implementation of quality improvement projects; maintains certifications for enhanced performance and improved patient outcomes.
- Education: is a mentor for lower-level ARNPs, develops educational resources for patients, their families, and staff.
- Contribution: is the main investigator on research projects, authors articles and books on advanced nursing practice.
- Leadership: is a leader of a hospital committee, local committee, professional organizations.
- Community service: plays the role of a leader and planner in community outreach.
The mentioned three levels of a clinical ladder were chosen for their potential to be incorporated in any health-care setting. Finding information on specific stages of ARNP development was problematic due to a lack of research on the practical application of the approach. It is imperative that future research focuses on exploring benefits of clinical ladder programs for the practice of ARNPs in order to formulate a cohesive framework for the approach.
References
Advancing from within: The value of clinical ladders. (2017). Web.
Bahouth, M., & Esposito-Herr, M. (2009). Orientation program for hospital-based nurse practitioners. AACN Advanced Critical Care, 20(1), 82-90.
Barnes, H. (2015). Nurse Practitioner Role Transition: A Concept Analysis. Nursing Forum, 50(3), 137-146.
Bitanga, M. (2012). Climbing the clinical ladder-one rung at a time. Nursing Management, 44(5), 23.
De Milt, D., Fitzpatrick, J., & McNulty, R. (2011). Nurse practitioners’ job satisfaction and intent to leave current positions, the nursing profession, and the nurse practitioner role as a direct care provider. Journal of the American Academy of Nurse Practitioners, 23(1), 42.
Hespenheide, M., Cottingham, T., & Mueller, G. (2011). Portfolio use as a tool to demonstrate professional development in advanced nursing practice. Clinical Nurse Specialist, 25(6), 312.
Lee, A. (2015). Clinical ladder for a community hospital. A doctoral project proposal. Web.
Leggat, S., Balding, C., & Schiftan, D. (2015). Developing clinical leaders: The impact of an action learning mentoring programme for advanced practice nurses. Journal of Clinical Nursing, 24(11), 1576-1584.
MacLellan, L., Levett-Jones, T., & Higgins, I. (2015). Nurse practitioner role transition: A concept analysis. Journal of the American Association of Nurse Practitioners, 27(7), 389-397.
Melnyk, B., Gallagher-Ford, L., & Fineout-Overholt, E. (2014). The establishment of evidence-based practice competencies for practicing registered nurses and advanced practice nurses in real-world clinical settings: Proficiencies to improve healthcare quality, reliability, patient outcomes, and costs. Worldviews on Evidence-based Nursing, 11(1), 5-15.
Paplanus, L., Bartley, P., & Mitra, K. (2014). Knowledge translation: A Nurse Practitioner Clinical Ladder Advancement Program in a university-affiliated, integrated medical center. Journal of the American Association of Nurse Practitioners, 26(8), 424-437.
Pasarn, R. (2012). Nurse practitioner job satisfaction: Looking for successful outcomes. Journal of Clinical Nursing, 22(17), 2593-2604.
Pierson, M. (2010). Twenty years of experience with a clinical ladder: A tool for professional growth, evidence-based practice, recruitment, and retention. Journal of Continuing Education in Nursing, 41(1), 33-40.
Scanlon, A., Cashin, A., Watson, N., & Brycem J. (2012). Advanced nursing practice hours as part of endorsement requirements for nurse practitioners in Australia: A definitional conundrum. Journal of the American Academy of Nurse Practitioners, 24(11), 649-659.
Shi, Y-L., & Li, J-P. (2016). Research progress of hierarchical division in nursing ladder management in China. Chinese Nursing Research, 3(3), 109-112.