Introduction
Nursing education requires one to consider different aspects of personal and professional growth as well as multiple disciplines related to health care. Prospective Masters-prepared advanced practice nurses (APNs) have to achieve many goals before obtaining the ability to practice independently. The objectives set in this course include the full understanding of personal responsibility and accountability for clinical decisions. Moreover, future APNs need to commit to making ethical choices that are informed by patients’ culture and individual needs. The wellbeing of society, as a whole, also cannot be neglected, and nurses need to learn how to think about global and local goals and issues. The multitude of duties that nurses have to perform and the skills that they need to acquire seems overwhelming. Thus, it is crucial for future professionals to approach any learning process with a systemic viewpoint, addressing each aspect of nursing education with principles and competencies in mind.
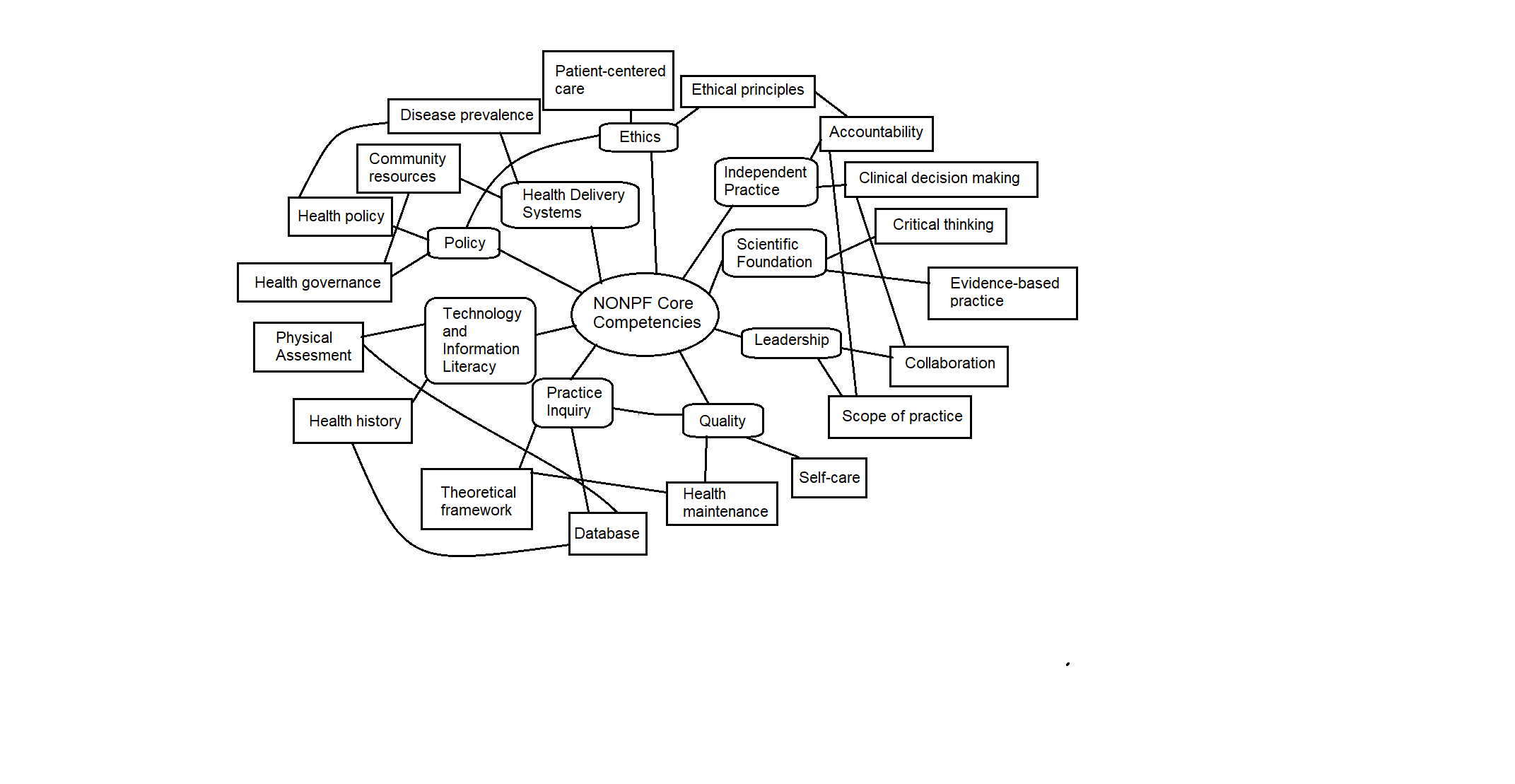
The present research presents an assessment of previously completed assignments, offering their appraisal and connection to the Program’s Outcomes (PO), the American Association of Colleges of Nursing (AACN) Master’s of Science in Nursing (MSN) Essentials, and the National Organization of Nurse Practitioner Faculties’ (NONPF) Core Competencies. The ten presented exemplars describe the most valuable pieces of work that I completed during this course to prepare for my future as a Masters-trained APN. Apart from considering how these assignments allowed me to achieve the competencies required by this profession, I also provide some self-reflection about each project. Reflecting is a vital part of continuous learning, valued in the field of nursing. With this investigation into my previous achievements, I aim to prove that my training has prepared me to assume the title of the APN.
Exemplar # 1: NR 505 Advanced Research Methods: Evidence-Based Practice
Early Mobility in the Intensive Care Unit
Early mobilization therapy issue became an area of concern after researchers discovered the negative consequences of bed rest following a sickness or trauma. These consequences can be versatile and dangerous for a patient’s health condition. The most prominent of them are cardiovascular deconditioning, increased risk of pressure ulcer development, muscle weakness and atrophy, neurological dysfunction. Thus, the given reasons are enough to support the need for developing an EBP project in this area (Patel, Pohlman, Hall, & Kress, 2014).
The nursing issue that has been chosen is the early mobility in the intensive care unit (ICU). Particularly, the advantages and the disadvantages of the early mobility therapy compared to the non-early mobility therapy for patients who are in intensive care will be analyzed. The reason for choosing this particular topic is that it is a significantly important issue in nursing practice. However, the amount of evidence that has studied the early mobilization of seriously ill patients is rather small. A few randomized and controlled researches have been conducted including only several hundred patients which significantly limits the strength of the evidence. Therefore, since the early mobilization therapy is considered safe and feasible, it is important to pay more attention to it (Schaller et al., 2016). Thus, this assignment consists of the following sections: Introduction, The Connection between FNP and Early Mobility Therapy, Nursing Issue, PICO Question, Research Literature Support, Theoretical Framework and Change Model, Research Approach and Design, Sampling Method, Conclusion, and References.
The Connection between FNP and Early Mobility Therapy
The specialty track that has been chosen is the Family Nurse Practitioner (FNP). FNPs are advanced practice nurses who work autonomously or in cooperation with other healthcare professionals to provide family-focused care. They provide a wide range of healthcare services for particular family units on the long-term basis. FNPs’ objective is to promote health, prevent diseases, treat patients, and counsel them across the lifespan. The role of an FNP in the early mobility therapy in the ICU is significant. FNPs look after patients when they are in intensive care.
In this regard, they can help implement the early mobility therapy during the treatment of their patients (Bernhardt, 2017). Thus, depending on the type of illness or injury, FNPs can determine whether to use early or non-early mobility therapy on their patients. Although in general, early mobility therapy helps prevent negative consequences caused by bed rest, in certain cases, it can lead to the relapse of a disease or to the opening of an undertreated wound. Therefore, FNPs’ purpose is to decide whether this therapy will harm a patient in a particular case or improve patient’s health, accelerate the healing process, and help avoid pernicious consequences connected with the non-early mobility therapy.
Nursing Issue
The nursing issue on which this project is focused is the early mobility program in the ICU. There has recently been an increase in the movement to begin research that focuses on the physical therapy utilization within the ICU establishment and the outcomes of the early intervention program with patients within this establishment. Progressive or early mobilization includes a system of movements that increase the activity of a patient beginning with the passive set of movements and ending with the independent ambulation. After the implementation of the early mobility therapy, patients will begin a special movement therapy in 24-48 hours after the mechanical ventilation (Schaller et al., 2016). The early mobility therapy had been implemented until recently. For several years, many researches were conducted in order to identify the advantages and disadvantages of this therapy. Eventually, a couple of years ago, some hospitals started to implement it. Thus, as for the frequency of the occurrence of this therapy, it is not frequent, as it is a new therapy, but those who have started to use it demonstrate chiefly the positive results (Reade & Finfer, 2014).
The initiation of the therapy begins after the establishment of the clearance from a physician or a medical team responsible for the ICU patients (approximately a week) and after the occupational therapy and/or the physical therapy has been consulted. Currently, numerous attempts are being made to launch more trials of the early mobility therapy for the ICU patients in combination with the interruption of sedation during the therapy time. Additionally, the implementation of the early mobilization protocol requires a multidisciplinary approach that includes collaboration between physicians, nurses, respiratory therapists, rehabilitation therapists, and administrators. Thus, this issue will engage all stakeholders, including improvement team leaders, senior leaders, and frontline staff who will be involved in the process of its implementation (Schaller et al., 2016).
Thus, this project will attempt to present evidence on the advantages and the disadvantages of the early mobility therapy in the ICU in contrast to the non-early mobility therapy. The rationale for choosing this particular nursing issue is that it is important and relevant now and requires much attention and effort on the side of all the stakeholders in order to be successfully implemented in nursing practice. Additionally, due to the lack of practical evidence of the positives and negatives of the early mobilization therapy, it is crucial to conduct further research on this issue in order to accelerate its overall implementation. Moreover, this therapy has already proved to be safe and efficacious (Bernhardt, 2017).
PICO Question
Currently, the problem of the implementation of the early mobility therapy in the ICU is relevant. Many types of research have been made since the first attempts to introduce this new program. Recent literature supports the need for this program, stating that it will help avoid the undesirable effects that can be caused by a long bed rest and improve patient’s health (Reade & Finfer, 2014). Based on the identified need for the early mobility therapy development in the ICU and the current relevance of the identified nursing issue the following PICO question is created to guide this project: In severely ill or injured patient in the ICU does early mobilization therapy results in ameliorated functional state and decrease ICU stay as compared to the non-early mobilization therapy? The main criterion for the search was the scholarly or peer-reviewed articles and journals using reliable databases like CINAHL, EBSCO, Medline Complete, PubMed and Google Scholar Search. The key terms used in the literature search were critically ill patients, early ambulation, early mobility, bed rest, intensive care units, physical therapy, quality improvements, rehabilitation, therapy, and mechanical ventilation.
Research Literature Support
Leditschke, Green, Irvine, Bissett, and Mitchell (2012) conducted a quantitative study, with the purpose to find out benefits of early mobilization of critically ill patients in the ICU and identify the frequency of this therapy. The research was a 4-week prospective audit on 106 patients from a mixed medical-surgical tertiary ICU, whose mean age was 60 years, median ICU length of stay was one day, and median hospital length of stay was 12.5 days. They were subject to: 1) active mobilization, which consisted in marching on the spot for more than 30 seconds); 2) active transfer from bed to chair; 3) passive transfer. The researchers collected de-identified data on the number of days the patient was mobilized, the type of mobilization used, adverse factors, and reasons mobilization could not take place. It was found out that participants were mobilized on 176 of 327 days spent in ICU. There were 2 adverse events that occurred during 176 mobilization episodes (1.1%). It was concluded that it was possible to mobilize critically ill patients for the majority of days of their stay in the ICU starting from the first (which supports the PICO of the study at hand). The key strength of the study is its scope and practical recommendations. Its major limitation is that no evidence proves that early mobilization is more effective than non-early therapy. The solution is to perform a similar study to compare the effects of the two approaches.
Engel, Needham, Morris, and Gropper, (2013) performed a qualitative study of the three selected medical centers as for the success of their ICU early mobilization programs. The major purpose of the research was to compare and contrast the impact an early mobility program produced on severely ill patients in three hospitals. The researchers used an interprofessional approach based on teamwork. As a result, the length of stay was reduced both in the ICU and in general care. Moreover, in all the three medical centers, this intervention also managed to lower the level of delirium and practically eliminated the need for sedation for the participants. This allowed concluding that ICU early mobility quality improvement program is capable of improving patient outcomes, which supports the PICO. The strength is that the described program can easily be applied to other types care units. Yet, there are no exact numeric indicators of the improvement, which is a limitation. The solution is to conduct a quantitative study to obtain statistical evidence.
Sricharoenchai, Parker, Zanni, Nelliot, Dinglas, and Needham, (2014) conducted a prospective observational study aimed to identify whether it is safe to use early mobilization therapy interventions in the ICU for reducing impaired physical functioning. The authors of the study explored how often and under what conditions some of 12 kinds of physiological abnormalities and safety risks presented by the implementation of mobilization therapy could appear. As a result of the experiment, 1787 patients with an ICU stay lasting minimum 24 hours, 1110 (62%) took part in 5267 mobilization sessions. All sessions were organized and performed by 10 therapists during 4580 days. A total of 34 (0.6%) of these sessions revealed safety risks or physiological abnormalities. None of these required any additional costs or prolonged stay, which supports the effectiveness of the therapy indicated in the PICO. The strength of the study is its huge sample size increasing liability and validity of the experiment. Its limitation is that only one hospital was involved in the research. The solution is to repeat the experiment in other hospitals which will include the influence of clinical factors as a variable.
Lord et al. (2013) performed a quantitative study, collecting data from articles and from the actual implementation of the program and created their own model of net financial savings. The researchers’ major goal was to evaluate how much annual costs implementation of the ICU early mobilization therapy allows saving. The intervention consisted in financial modelling of results for the implementation of the early mobilization program. The researcher presented the results of using the developed model for ICUs with 200, 600, 900, and 2,000 annual admissions. It was identified that $817,836 of cost savings could be achieved through the implementation of the program in the example scenario with 900 patients per year. These savings were generated through stay reductions of 22% (for ICU) and 19% (for floor). This implies that the program indeed allows saving costs through the amelioration of patients’ condition (which again supports the PICO). The key strength of the study is that a new model was developed that relies on actual experiments of the program implementation. The limitation is that there is hardly any novelty except the implementation of a new tool. The solution would be to apply the same tool to compare the effects of different types of mobilization therapy as this may give unprecedented results.
Theoretical Framework and Change Model
For the purpose of this project, Lewin’s Change Theory was selected as a theoretical framework as it provides a method to successfully implement a planned change (the one occurring by design). The main concepts of the theory are field and force. The former is a system, which means that in case one of its elements changes, the whole body of it is affected. Change is viewed in a disrupted balance of driving and restraining forces. While a driving force initiates movement or shift towards transformation, a restraining force is the one hindering the process. In case of the early mobility issue, the driving forces include: educational programs for staff and patients, evidence-based literature supporting early mobilization, administration support, etc.
Restraining forces are numerous: patients’ reluctance to try early mobilization as a part of general resistance to change, nurses’ unwillingness due to the fear of accident extubation, patients’ delirium, oversedation, lack of specific policies and comprehensive programs, etc. Thus, according to the chosen theory, it is needed to: 1) unfreeze the status quo; 2) gradually introduce changes; 3) freeze the change making it durable by assimilating in the system. Success and sustainability of the project intervention will be ensured by the capability of the framework to allow better understanding of patients’ needs and fears and developing an implementation plan in accordance with these factors. An education program will be required to integrate early mobilization into practice since it cannot simply be imposed upon ICU patients if they opt for non-early intervention or no mobility at all. Lewin’s framework will make it possible to change the entire system through an individual change.
The implementation of the proposed change will be guided by Logic Model for Program Development since it allows planning the desired outputs, outcomes, and the general impact of the change in advance. The model also makes it possible to measure both patients’ and nurses’ knowledge concerning the benefits of early mobilization in the ICU in order to assess what training will be required (Chen, 2014).
Research Approach and Design
Since the research goal is to answer whether a severely ill or injured patient will have an ameliorated functional state and a decreased stay in hospital with the realization of the early mobilization therapy compared to the non-early mobilization therapy, it would be reasonable to opt for a quantitative approach. The design is going to be experimental. It will test a hypothesis through an intervention, the impact of which will be the major focus of the study. Furthermore, the experiment is required to look for the ways to improve condition of real patients. The choice of this approach is accounted by the fact that it allows controlling the study conditions using precise measures and strict regulations of all variables. The major advantage of the quantitative study is that it is possible to generalize the results from a sample to a larger group of the population. Yet, there is also a disadvantage: The research design does not allow discovering anything new since it is purely deductive.
Sampling Method
The target population that the study is going to address will include severely ill or injured patients from 25 to 65 years of age undergoing treatment in the ICU. Non-probability sampling will be used, which is supported by the fact that only patients of a particular age group who currently suffer from acute diseases or injuries will be eligible to participate in the research. This type of sampling was selected due to the fact that it allows researchers to focus on a particular group of patients (as it would be wrong to involve patients from the general care unit in the same experiment).
The following steps will constitute the sampling procedure:
- establishing eligibility criteria;
- choosing a random sample of patients from 25 to 65 undergoing treatment in the ICU;
- informing the participants about the goals of the research and obtaining their informed consent;
- collecting background information about the participants in order to decide on variables;
- dividing the patients into the control (receiving non-early mobilization therapy) and intervention groups (undergoing early mobilization); each group will include approximately 50 participants.
The two major advantages of this sampling procedure is that: 1) non-probability sampling implies that only patients meeting the criteria will be able to participate–therefore, the intervention will be thoroughly controlled and the results will be precise; 2) at the same time, randomized trial will eliminate bias. Yet, there is also a disadvantage: Non-probability samplings practically do not take into account extraneous variables, which can be influential.
Institutional Review Board help researchers protect participants’ rights relying on the following principles:
- obtaining an informed consent;
- respecting confidentiality and privacy;
- discussing the limits of confidentiality (informing participants what data will be made public and how it will be used) and preventing their violation;
- informing participants about federal and state laws that protect their rights.
Conclusion
It has long been unclear whether early or non-early mobilization therapy is preferable for patients in the ICU as the former might lead to aggravation of the patient’s condition whereas the latter is usually less effective. The role of FNPs is crucial since they must decide whether the selected therapy will harm a patient or improve their overall health.
However, according to the results of the experiments conducted by other researchers, it was found out that early mobilization therapy brings about the expected improvements in most cases, which means that the outcomes for this project proposal will be positive.
PO #4: Integrate professional values through scholarship and service in health care (Professional identity)
This program outcome was met because, in this assignment, I gathered data about the research question and evaluated it to introduce evidence-based knowledge into practice. The suggestion for implementing early mobility interventions was based on previous findings, thus showing my ability to integrate scholarship into the field of health care. It is notable that the program outcome considers one’s ability to use scholarship a professional identity, thus highlighting the need to understand the scientific foundations of any practice activity. By examining an initiative and comparing its results with those of other programs, I have supported my professional identity.
AACN MSN Essential I: Background for Practice from Sciences and Humanities
This essential was addressed in the paper since the topic of my study was focused on drawing knowledge from various areas of health care research. The investigation into the outcomes of introducing an early mobility initiative to an Intensive Care Unit (ICU) utilized a theoretical framework of Lewin as well as previous findings about the effectiveness of similar projects. As a result, I was able to combine specific information from different disciplines for practice improvement.
NONPF Core Competency 4: Practice Inquiry
The present research paper followed and met the objectives set by the fourth NONPF competency. I investigated previous scholarly research, introduced a theoretical framework for the project, utilized my skills in searching medical databases, and presented the results of my investigation. Moreover, I analyzed the consistency of my findings with the existing scholarship and reflected on their impact on future investigations.
Concepts and Reflection
A theoretical framework is the first concept introduced in this assignment. It is a foundation for research papers, created to support the structure of an investigation. Authors can choose a framework to guide their examination and inform their selection of participants, data gathering methods, and analyzing tools. A theoretical framework’s choice can determine the path which a researcher may take when exploring a posed question.
The second concept is a database which is reviewed in relation to medical publications. It is a collection of books, journal articles, and clinical guidelines that present the latest findings in the field of health care. Nurses have to understand how to search for relevant information using these databases and how to appraisee the selected sources to choose the most reliable data and integrate it into their research.
The present exemplar allowed me to exercise my critical thinking and investigate a problem that exists in health care right now. I used various databases and gathered the information that helped me to evaluate the usefulness of early mobility programs for patients in the ICU. The in-depth consideration of the issue revealed that the current research of it was lacking. However, the available findings supported the notion that a change in mobility initiatives could improve patients’ health. As an outcome, this assignment informed my opinion about activities that could be introduced to ICUs and led to me forming a program for practice change.
I also examined the connection between Family Nurse Practitioners (FNPs) and early mobility therapy, assessing their role in improving care in the ICU. I understood that the initiative for launching more trials to test early mobility programs requires FNP’s participation since they have an opportunity to build strong relationships with their patients. The choice between early and non-early therapy is often dependent on nurses’ decisions. Thus, the ability to consider research data is a vital skill that increases nurses’ quality of care.
Exemplar # 2: NR 506 Health Care Policy
Significance of the Problem
A public health policy issue I am interested in concerns depression among high school students. Only about 40 years ago, depressive disorders in adolescents were largely neglected since most physicians doubted that the problem could exist at such an early age. However, it has been proven depression may not only appear in teenagers but also increase associated morbidity and mortality rates. Therefore, the importance of the issue is hard to overestimate as plenty of human lives are at stake.
The proposed policy is to introduce depression screening at schools to detect the problem in time. The immediate target of the policy is local level. Later, the issue will have to be discussed at the state level since it is not enough to solve the problem only locally. There is a necessity to develop universal guidelines for screening that would be applicable in all schools across the state. This will considerably facilitate the procedure of policy implementation via standardization. The legislator that is to be contacted first is Janice Kerekes, Clay County Board Member Representative, District 1.
Analysis of the Problem/Empirical Evidence
The specific problem surrounding the issue of depression among adolescents is the absence of timely diagnosis as the first step to depression management. More than 30% of depressed adolescents are not recognized and do not receive treatment, while the clinical spectrum of their condition may vary from simple sadness to bipolar disorder, which can be irreversible if not detected in due time. The research shows that approximately 9% of school students at the end of adolescence meet criteria for depression whereas 20% of them state that they suffer from the condition since early childhood (Allison, Nativio, Mitchell, Ren, & Yuhasz, 2014).
Currently, there is no regulation that would oblige schools to conduct screening that would allow detecting the condition in high school children. Thus, in order to improve the situation, it is necessary to introduce changes to regulatory issues. Mandatory annual screenings for adolescents are recommended as the most effective option. Nurses will be for conducting them in high schools. This necessity is supported by the fact that depression is now the major cause of psychosocial impairments, increased hospitalization, alcohol and drug abuse, antisocial behavior, and suicide. There is also evidence that more than 50% of cases of negative mood changes in adolescents can be eliminated through social therapy that makes it possible to monitor and modify distorted thinking by encouraging social activities and resolving conflicts (Allison et al., 2014). This helps prevent severe impairments of the psyche caused by clinical depression. In case of a more serious condition, early intervention makes it easier to do without antidepressants or tranquilizers and mitigate the effects with psychotherapy only.
Impact and Importance to Nursing
There is evidence showing that screening with standardized and validated questionnaires lead to early recognition and treatment, which is more effective than waiting for more severe symptoms to be apparent, resulting in lower cost and better outcomes. The costs include psychiatric hospital admissions, emergency visits, total mental health costs, poor school attendance for the teen and work absences for parents. The Patient Health Questionnaire Modified for Teens (PHQ-9 Modified) is a well-accepted, standardized, validated questionnaire, used by many providers for patients between the ages of 11 and 20 and takes less than five minutes for them to complete. It can also be administered and scored by a school nurse for screening depression among high school students. Since the problem have long-term consequences and lead to poor school performance, family relations, and state of health, neglecting it may mean that in future, nurses will have to deal with the population, suffering from a whole spectrum of mental conditions therefore annual screening is crucial for schools to introduce.
Analysis of the Policy Issue
Context
School is the main place outside home where teenagers spent the majority of their time. Therefore, detecting behavior deviations and providing preventive measures is the primary responsibility of a school nurse. Despite the fact that there are two acts regulating suicide prevention (the Youth Suicide Prevention Act of 1987 and public Health Service Act of 1990), there are not universal guidelines for screening and follow-up. Having no elaborated plan of action, school superintendents often have to decide for themselves how to manage the problem. Researchers have found that no program of those that have been developed has been tested in randomized trial, which means that none of them are evidence-based.
Goals/Options
The ultimate goal of depression screening it to create a list of depression indicators on the basis of the observed cases for teachers and parents to be able to identify the problem at an early stage. In addition to creating other learning conditions to those whose depression is getting aggravated owing to the unfavorable environment a nurse could provide a referral for psychotherapy to teenagers suffering from various forms of depression based on the gravity of the condition. Lastly, ensuring follow-up and cooperation with parents are maintain for continuity of care.
There are three major options for schools to choose from: 1) to include problem education into the curriculum programs; 2) to provide training for teachers; 3) to introduce regular screening.
Evaluation of Options
Although the first option has been studied more profoundly, its effectiveness is still doubtful. On the contrary, there is extensive evidence that curriculum programs do not prevent depression or suicidal behaviour in high school students. They do not feel that theoretical education is connected with their real-life condition (Prochaska, Le, Baillargeon & Temple, 2016). Moreover, many of them try to conceal it out of fear of bullying.
The second option, in-service training for teachers can potentially assist them in identifying students that are at risk. However, there is little research on the efficacy of the measure, which does not allow making inferences about its superiority over the other two (Cunningham & Suldo, 2014). Besides, the assessment of a person without medical education can be rather subjective.
Finally, the third option involves comprehensive evaluation of students’ psychological state including self-reported data, results of various psychological tests, and interviews (Prochaska et al., 2016). This measure is more preferable since it can be applied in all schools regardless of the curriculum and provide more objective results.
Recommended Solution
It is recommended to issue a new regulation for schools obliging them to introduce a depression screening program for high school students. At the first stage of the program, students will need to complete an evaluation form, the major goal of which is to identify those who are at elevated risk. At the second stage, the risk group is assessed via computer tests. At the final stage, a school nurse interviews those students whose results raise concerns to be able to diagnose their stage of depression.
Policy makers have to provide schools with psychometrically validated screening tools that must be tested as per their sensitivity (the ability to detect students with depression), specificity (the ability of identifying those who do not have any related conditions), positive predictive value (the relation between whose who screen positive and who are actually positive), and negative predictive value (the relation between whose who screen negative and who are actually negative).
Status Updates
American Academy of Child and Adolescent Psychiatry provides updates on this and other topics related to mental health of children and teenagers. The website of the organization features numerous annual reports and recommendations for all stakeholders involved. Furthermore, there are also strict pharmaceutical guidelines for every mental disorder. The academy has a 60-year history in the field and therefore can serve as a reliable source of information on policy and other psychological conditions.
Conclusion
There is a nationwide problem with detection, treatment, and prevention of teenage depression. For nurses, it means that the quality and nature of care delivery may be negatively affected by the wrong diagnosis. Since the problem is fraught with long-term consequences and lead to poor socialization, performance at work, family relations, and state of health, neglecting it may mean that in future, nurses will have to deal with the population, suffering from a whole spectrum of mental conditions. Thus, due-time screening is crucial for schools to introduce.
AACN MSN Essential VI: Health Policy and Advocacy
The assignment discussing depression prevention among high schoolers helped me examine the ideas of health policy and advocacy. This essential is concerned with the ways in which nurses can impact health care through policy development and systemic change. I investigated the current approach to high school programs for depression detection and prevention and designed a policy proposal for a change on a local level. I explored strategies for disseminating the information about my proposition to appropriate legislators. Furthermore, I learned how to present the data about the problem to demonstrate why new policies are necessary. For instance, the finding that no regulations for depression screening in educational facilities exist shows that children’s mental health is not prioritized enough in health and educational policies. New approaches to screening regulations can improve depression detection and allow health care professionals to treat students on time.
NONPF Core Competency 6: Policy
The sixth competency was met in the assignment about depression among high school students. It requires nurses to demonstrate a high level of understanding of connections between policy and practice (NONPF, 2017). Here, the link is apparent – regulations for screening would improve nurses’ reach to the population of young students and their health. Moreover, it would change the view of depression and possibly reduce rates of negative consequences, including self-harm and suicidal ideations. As evidence suggests, advocacy for depression evaluation can increase children’s access to psychotherapy, preventing deterioration and necessity of pharmacological intervention. The assignment evaluated the proposed policy to support its goal of creating a safe and healthy practice for students. As an outcome, I was able to see how policy leads to positive change and contributes to global issues’ solution.
Concepts and Reflection
The first explored concept is health policy- a set of actions and plans that are created to achieve specific health-related goals through health care. A policy can set target goals for organizations and communities to reach in a specific time period. Moreover, it may describe a particular vision with which entities should align their initiatives. It also determines priorities and assigns roles to stakeholders, informing all involved persons.
Health governance is another concept – it is a set of actions taken by a government body to improve the health care sector (de Leeuw, 2017). It includes the creation and assessment of health policy, also considering financial, social, and political aspects of each decision. Governance ensures that policy responds to the emerging trends and issues and furthers the state of national health. Furthermore, it regulates policy implementation and assessment and establishes tools for accountability.
The investigation into the problem of undetected depression in students showed me the extent to which health policy can benefit large groups of people. The impact of health policy is substantial – it can prevent various population-wide issues and change the course of health care. However, its development is challenging as it requires one to consider how the national system operates currently and what changes are possible. The lack of regulation, for example, raises concerns and shows that policy should incorporate clear instructions for schools to adopt. While completing this assignment, I understood that policy has to provide solutions that are not only beneficial to people but also well-researched, stable, and practical. Multiple approaches are reviewed in the paper, including problem education, teacher training, and regular screening. The analysis shows that the third option is the most reliable, thus being a potential foundation for policy change.
Exemplar # 3: NR 503 Health, Epidemiology & Statistical Principles
Chronic Obstructive Pulmonary Disease in Florida
Chronic obstructive lung disease (COPD) is cited among conditions contributing to the pulmonary cancer etiology (Aldrich et al., 2015). Consequently, there has been an urge to intensify research to determine the interrelationships between the two disorders to invent improved strategies for reducing their impact on society. Lung cancer causes the highest number of cancer-related deaths in the United States, while COPD is the third primary cause of general mortality, and the combination of the two creates an immense public health burden, causing significant disability, morbidity, and mortality (Aldrich et al., 2015). The average total annual cost of COPD for the year 2010 was $49.9 billion, and the chances of being employed plunged by 8.6% for those with the COPD linked disability (Doney et al., 2014). The statistics released in 2015 from the Behavioral Risk Factor Surveillance System (BRFSS) indicated a 9.6% countrywide incidence rate for the self-reported COPD cases in grownups aged 40 years or more (Aldrich et al., 2015). It also showed that a regional variation of the disease across the USA with Southern States recording the highest prevalence rates (Aldrich et al., 2015).
Background of the Disease
COPD is a manageable and curable lung disease with some important non-pulmonary effects that may contribute to the severity in individual patients (Reid & Innes, 2014). The pulmonary constituent of the sickness is typified by an almost irreversible breathing limitation that is gradual and accompanied by an unusual allergic reaction of the lungs due to noxious gases and particles (Reid & Innes, 2014). Accompanying diagnoses include chronic bronchitis, chronic obstructive bronchitis and emphysema. Chronic bronchitis is characterized by the persistent copious mucus production into the bronchioles with the presence of a cough most of the time for no less than three consecutive months in two successive years (Holt et al., 2015). In contrast, emphysema is the permanent hyperinflation of the alveoli at the end of terminal bronchioles accompanied by damage to the alveolar walls without obvious fibrosis (Reid & Innes, 2014). The stimulation of the inflammatory cells (neutrophils, macrophages, and CD+ lymphocytes) by exposure to noxious particles and gas causes the cells to release several chemical mediators –tumor necrosis factor α, interleukin 8, and leukotriene B4 – that bring about the irritation (Reid & Innes, 2014).
In addition, the impairment of the alveoli may be due to overproduction of proteases, and oxidants activity. These conditions result in difficult breathing (dyspnea), wheezing, cough, sputum production, airway obstruction, decreased blood O2 concentration and high blood CO2 levels (Doney et al., 2014). Also, this blend of weakened pulmonary function and repeated exacerbations promotes a medical condition characterized by the reduced endurance to exercise and physical activity, and deconditioning; factors that translate into disease progression, poor quality of life, disability and eventually premature death. Potential complications of COPD include respiratory infection, pulmonary hypertension, malnutrition, pneumothorax, corpulmonale, polycythemia, acute and chronic respiratory failure, arrhythmias, depression, nocturnal hypoxia, and disordered sleep (Doney et al., 2014).
COPD takes 120,000 American lives every year (Srivastava, Thakur, Sharma, & Punekar, 2015). However, the 2014 statistics indicated a reduction in age-adjusted death rates from 1999’s 57 per 100,000 for men and 35.3 per 100,000 persons for women to 44.3 and 35.4 respectively (Holt et al., 2015). The death toll from COPD in Florida in 2014 was estimated at 34.7-38.7 per 100,000 people. The state prevalence rate was 6.5 – 7.6%. The 2014 average prevalence rates for counties in Florida were 3.3 – 17.7%, while the congressional district ranges were 3.4-14.0% (Holt et al., 2015).
Surveillance Methods
To evaluate the state-level and national prevalence of COPD, the impact on the population’s value of life, and use of health care resources by patients, the CDC and the State Departments of Health use data from the BRFSS (Holt et al., 2015). For instance, the Florida Department of Health uses the Florida BRFSS State Data to obtain the state-specific, population-grounded estimates of COPD prevalence and associated risk behaviors among the residents (Holt et al., 2015). The data are useful for ascertaining issues of health of primary importance and pinpointing populations at risk of ailments, disability, and death (Holt et al., 2015). The information also supports the development and evaluation of prevention programs, community, and policy maker training about disease prevention and the reinforcement of community policies that encourage health and prevent disease (Holt et al., 2015).
BRFSS is a “state-run random-digit-dialed phone assessment of the non-institutionalized, US civilian grownups aged 18 years and above” that is conducted yearly by the CDC health divisions at the state level in homes accessible via phone calls (Holt et al., 2015, p. 8). The response rate for BRFSS is computed using specific criteria or response formula and is the proportion of the number of people who complete the survey to that of the eligible persons (Holt et al., 2015).
Descriptive Epidemiology Analysis
Disease prevalence is related to multiple health and socioeconomic factors. It has been approximated that 10 -16 million persons in the US have been diagnosed with COPD and that 14-16 million more cases go undiagnosed (Doney et al., 2014). That is due to under-reporting or under-diagnosis, predominantly those cases with mild to moderate disease. In addition, self-reports of the disease may be inaccurate, making it difficult to ascertain the actual prevalence of COPD in the state (Aldrich et al., 2015). The incidence, morbidity, and mortality of this disease are increasing with the aging of the US population (Doney et al., 2014).
Risk factors for acquiring COPD include tobacco smoking (>95% of cases), biomass fuels use, occupational (coal mining or prolonged contact with cadmium), and air pollution (Reid & Innes, 2014). Other factors that predispose individuals to COPD include repeated infections and diseases such as adenovirus and HIV, low socioeconomic status, cannabis smoking, poor nutrition, genetic factors like α1-antiproteinase deficiency, and the respiratory system hyperactivity (Reid & Innes, 2014). Children with pulmonary growth and functional impairment due to low birth weight and childhood or maternal infections are at higher risk of suffering from the disease. Apparently, smoking cessation can halt the progress of COPD.
From the state data in table 1 above, it is evident that the Hispanics are less prone to COPD than the non-Hispanic Whites and the non-Hispanic Blacks (3.7% compared with 9.7% and 5% respectively). Women have a higher incidence of COPD than men (8.8% compared to 6.4%). Persons below the high school level of education often report higher disease incidences than those at advanced levels of training (13.2% in comparison to 8.3% for high school and 5.8% for college). Also, unmarried couples are more susceptible to COPD than married people (8.8% to 6.5%). Similarly, employment status correlates with reported COPD cases. Disease incidences are prevalent among the physically impaired, unemployed or retired than among the students, house makers and the employed. Verified COPD cases drop with growing household income from 11.5% among those with an annual family income <$25, 000 to 3.7% for those with annual income ≥ $50,000. Persons who have been smoking for a longer duration have a higher incidence rate for COPD than former smokers and non-smokers. The asthmatic patients are also likely to suffer from the disease as compared to the non-asthmatic persons.
Exacerbations and disease severity of COPD are accompanied by health-related quality of life and economic drain. Other critical parameters connected with increased burden are increasing age, female gender, and the presence of co-morbidities. The impact on population outcomes can be estimated by observing the overall health condition, psychological well-being, functional status, fatigue, and life quality (Srivastava et al., 2015). Drainage of economic resources occurs when patients seek treatments. Therapy is by the use of bronchodilator drugs. Further, patients with COPD often require prolonged oxygen therapy, and antibiotics are frequently used to treat exacerbations caused by bacterial infections (Reid & Innes, 2014).
Diagnosis of COPD
Diagnosis is based on medical history, physical examination, and the results from the pulmonary function tests. However, differential diagnosis is essential to discriminate COPD from diseases such as chronic asthma, tuberculosis, bronchiectasis, and congestive heart failure (Reid & Innes, 2014). The patients exhibit atypical pulmonary function test values, e.g., a lower FEV1 (Reid & Innes, 2014). The maximum volume of air that can be inhaled forcefully per second (FEV1) and FVC are essential prognostic indicators in a patient, with the average rate of FEV1 decline being an important objective measure to assess the COPD progression (Reid & Innes, 2014). FEV1 is excessively reduced in airflow obstruction conditions, leading to FEV1/FVC ratios of less than 70% (Reid & Innes, 2014). The average rate of decrease of FEV1 in healthy, nonsmoking persons due to aging is 25-30mL annually (Reid & Innes, 2014).
For smokers, the rate of decline is higher, being steepest in heavy smokers. The more severely diminished the FEV1 at diagnosis, the steeper is the rate of decline. Also, the more the number of years of smoking and the number of cigarettes smoked, the steeper the decreases in lung function. The diagnosis is through spirometry and confirmation is made when the post-bronchodilator FEV1 is below 80% of the projected figure and that the FEV1/FVC <70% (Reid & Innes, 2014). If the FEV1/FVC <70% and FEV1 is more than 80%, this may be a typical finding in adult patients or an indicator of the mild disease (Reid & Innes, 2014). The seriousness of COPD is defined according to the post-bronchodilator FEV1 as a proportion of the projected value of the patient’s age (Reid & Innes, 2014). An FEV1/FVC value of <70% and FEV1 of ≥ 80% would indicate mild disease, while an FEV1/FVC figure of <70% and FEV1 of 50-79% would suggest moderate disease (Reid & Innes, 2014). The diagnoses for severe and serious COPD include FEV1/FVC is <70% and FEV1 of 30-49% and FEV1/FVC<70% and FEV1 <30%, respectively (Reid & Innes, 2014).
Measurement of lung volumes aid in the assessment of hyperinflation and is performed either by the helium dilution technique or body plethysmography (Reid & Innes, 2014). In this case, a low gas transfer factor suggests the presence of emphysema. In addition, the exercise tests are essential in evaluation of exercise tolerance and provide a baseline on which to judge the response to bronchodilator therapy or non-pharmacological treatments (Reid & Innes, 2014). Notably, although there are no reliable radiographic signs that correlate with the gravity of airflow obstruction, a pulmonary x-ray is essential to rule out other diagnoses – cardiac failure, lung cancer or presence of bullae (Reid & Innes, 2014).
As mentioned above, spirometry is the gold standard test for diagnosis of this disease. It is a painless breathing test. In some healthcare units, this screening test is administered freely. It is an essential step to ensure an accurate diagnosis and guide medication. The international COPD guidelines – the GOLD criteria – provide recommendations for screening, disease severity classifications, medical treatment, and prescription. Guideline-based care has been shown to improve patient outcomes in COPD (Holt et al., 2015).
Plan for Action
The prospective benefit of epidemiologic knowledge is realized when it is transformed into health policy and later prototyping and implementation of disease control programs. The health planning phase involves the following key steps: assessing disease frequency, identifying the causes, evaluating the efficacy and efficiency of existing treatment, implementing interventions, monitoring activities and measuring the progress. To determine the outcome of the interventional measures or actions, it is crucial to re-measure burden-of-illness parameters, analyze trends in population groups at risk of disease, and ascertain the acceptance of various interventions after disease awareness program.
In my case, I plan to promote awareness of GOLD guidelines among GPs through training and underscore the need for adherence to them. Also, I plan to educate, inform and empower the Florida community by identifying gaps in the current public information about COPD. I intend to research more on health hazards and risk factors of COPD given the current economic, environmental and lifestyle dynamics that impose health and psychosocial strain on the people. As appropriate, I will emphasize the importance of smoking cessation; encourage attending a smoking cessation program and/or asking the treating clinician about medication, nicotine patches or gum, and counselling to promote smoking cessation. Further, I purpose to diagnose and investigate COPD in Florida to identify emerging threats and mobilize the public to implement distinct preventive, diagnostic, rehabilitation and support plans. The outcomes of these endeavors can be measured by the approaches mentioned above.
Conclusion
COPD is an epidemiological disease with serious health implications for the people of Florida. It has both humanistic and economic side effects. Statistics on the disease are obtained through surveys conducted by the Florida BRFSS, etc. Diagnosis and treatment of the disease follow the GOLD guidelines. Treatment for the disease involves both preventive and pharmacotherapy approaches.
PO #2: Create a caring environment for achieving quality health outcomes (Care-Focused)
The second program outcome was met in the assignment investigating chronic obstructive pulmonary disease (COPD) in Florida. The goal of this outcome is to teach nurses how to establish and maintain a setting that supports quality improvement. This assignment urged me to create an in-depth plan for dealing with COPD, including tools for disease surveillance, epidemiology and background information for the condition, and strategies for awareness promotion. As a result, this plan can serve as a foundation for nurses’ further research into COPD and its treatment.
AACN MSN Essential VIII: Clinical Prevention and Population Health for Improving Health
The assignment was focused on evaluating the health of the population in Florida in relation to COPD. The aims of the project were to accumulate data about COPD and its effects on the people living in the state. The details about COPD’s prevalence as well as its annual costs allowed me to see how I, as an advanced practice nurse, can address the disease’s prevention and management on a community-wide scale. As a result, I integrated the essential of population health into my skills.
NONPF Core Competency 7: Health Delivery Systems
This competency requires one to develop health care systems that acknowledge the needs of diverse populations (NONPF, 2017). The present research showed that smoking, air pollution, occupations such as coal mining, low socioeconomic status, and other factors increase the risks of people to develop COPD. Therefore, I was able to highlight the needs of specific groups and their increased exposure to the dangers of this condition.
Concepts and Reflection
Disease prevalence is the first identified concept – it is the percentage of people who have a condition in comparison to the whole population (De Nicola & Zoccali, 2015). Prevalence is related to population health research in that it helps one determine how pressing is the issue (disease). The specific prevalence rates in different communities also demonstrate which characteristics may be connected to people acquiring the condition. In this case, the prevalence of tobacco smokers among people diagnosed with COPD is apparent, and one can note a link between these aspects.
The second concept is community resources, sources of education for residents about the hazards of a particular condition (Hagan, Schmidt, Ackison, Murphy, & Jones, 2017). These resources are meant to raise awareness about the condition and improve population health by aiming to disseminate pertinent information about prevention, diagnosis, treatment, and lifestyle changes. Nurses create materials for communities, using simple language and EBP information to ensure high levels of understanding and adherence.
The examination of COPD among residents of Florida assisted me in understanding how population health is evaluated. I obtained statistics about the state’s communities and saw that some groups were more vulnerable than others, finding several risk factors that should be addressed. As an outcome, I approached the health of patients on from an individual but a group perspective, finding strategies for systemic change and organizational improvement. I also saw how interprofessional collaboration could be used to manage the health of many people at once. Data collection, patient education, transition between different health care delivery mechanisms require medical professionals to work together to raise awareness and cover all aspects of people’s lives.
Exemplar # 4: NR 510 Leadership and Role of the APN
APN Professional Development Plan
Advanced practice nurse (APN) is a position characterized by one’s independence, leadership skills, and professionalism. Nurse practitioners in Florida are certified to perform a variety of activities, including patients’ assessment, treatment, and drug prescription. To apply for a job in the field of AP nursing, one has to evaluate the regulations and guidelines of the state, in which the APN is planning to work. One should assess his or her qualities and skills to establish the level of experience and readiness for the job. Finally, it is vital for students and recently graduated nurses to learn various networking strategies and marketing techniques which can help find a suitable job and impress the employer before, during, and after the interview. This paper analyzes the scope of practice for the APN in the state of Florida, provides a personal assessment of the author based on the Benner’s Self-Assessment Tool, includes an example of a possible Curriculum Vitae (CV), and discusses some networking and marketing techniques for successful employment.
APN Scope of Practice
Florida’s regulations allow APNs to perform a broad range of activities. Sastre‐Fullana, Pedro‐Gómez, Bennasar‐Veny, Serrano‐Gallardo, and Morales‐Asencio (2014) note that the level of autonomy of APNs has greatly increased over the years. However, some practices remain unavailable or limited for nurses in Florida. The scope of practice for APNs is outlined in the Nurse Practice Act of the state. APNs can administer and dispense drugs and controlled substances, if they possess necessary training related to the area of expertise. HB 423 ARNP/PA Controlled Substance Prescribing bill authorizes physician assistants and advanced registered nurse practitioners to prescribe controlled substances under current supervisor standards for PAs and protocols for ARNPs beginning January 1, 2017 (Florida Board of Nursing, 2018).
Under the bill, an ARNP’s and PA’s prescribing privileges for controlled substances listed in Schedule II are limited to a seven-day supply and do not include the prescribing of psychotropic medications for children under 18 years of age, unless prescribed by an ARNP who is a psychiatric nurse. Prescribing privileges may also be limited by the controlled substance formularies that impose additional limitations on PA or ARNP prescribing priveleges for specific medications. An ARNP or PA may not prescribe controlled substances in a pain management clinic (Florida Board of Nursing, 2018). APNs can also choose and start specific therapies for patients, order labs and medication and diagnose and treat medical condition. However, it is vital to remember that all procedures of an APN should be recorded in a special supervisory protocol, which should be available to the department upon request.
APNs also have different specialties which further expand their scope of practice. For example, certified registered nurse anesthetists may perform anesthetic services and order various diagnostic procedures and preanesthetic medication, participate in preanesthesia care, and treat them during postanesthesia recovery (Florida Board of Nursing, 2018). Certified nurse midwives have a different set of available activities, which are also covered by the Nurse Practice Act. The healthcare facility at which these specialists work should have an established protocol for procedures that midwives can perform. For instance, some minor surgical procedures and management of obstetrical patients are possible for these nurses. Furthermore, a psychiatric nurse can prescribe psychotropic substances for treating patients with mental disorders. All in all, the actions of an APN should all be outlined in a protocol with a managing physician, who supervises the practice of nurses.
Personal Assessment
The significance of personal evaluation in the process of entering the job market cannot be overstated. It is clear that nursing students need to have a set of professional skills to succeed in their search for a suitable position. However, one’s training is not the only part that should be accounted for before applying for opened positions. Nurses should understand their level of preparedness and expertise in various areas of this profession. For example, the Benner’s Model views self-assessment as a range of experiences in different situations that can happen in the workplace (Lima, Newall, Kinney, Jordan, & Hamilton, 2014). One’s competence is also related to confidence, preparedness, and understating of self.
Self-assessment can include different categories of preparedness and one’s thoughts about the future. According to Lima et al. (2014), the competence of graduate nurses is hard to measure due to the lack of work experience. While most students usually work while receiving their education, their current experiences differ from their future occupation. Barnes (2015) points out that such a transition between roles complicates the process of self-assessment and often yields misleading results.
First of all, it is necessary to ask oneself, which career elements seem the most valuable and appealing to the nurse (DeNisco & Barker, 2015). For instance, I would like to focus on progressive adult care as I already possess significant knowledge about telemetry care, emergency departments, and acute care. I feel comfortable and confident in my experiences in this area of work. Therefore, it seems significant to me to progress by learning more about these spheres of care. Second, one should assess his or her expectations of the new position. I look forward to having more autonomy over my actions and being able to participate in patient care more actively.
The occupation of an APN can open new possibilities for long-term commitments and goals. However, I am also nervous about assuming a role with more responsibilities. Currently, one of my weaknesses is the inability to manage my time. While my experience with acutely ill patients gives me an advantage in the situation of emergency, my new position may pose challenges that could be hard to overcome. Thus, my main weakness should be addressed for me to succeed at the job.
Furthermore, one should discuss some ways to deal with stress. For example, I cope with excessive stress by trying to look at the complicated situation from a different angle. By distancing myself from the initiators of stress and perceiving the problem from a different point of view, it becomes easier for me to search for the source of the negativity. Finding the stressor can greatly reduce its impact. Taking some time to relax is also essential in dealing with stress. Finally, communicating your feelings to other people and finding support in them are also viable techniques for coping with stressful situations.
By analyzing past experiences and existing skills, one can establish the level of competence for the current or future position. My work has given me the opportunity to test my abilities and improve my understanding of the profession. While the role of an APN will be new for me, my knowledge of the practice setting and extensive experience in a particular sphere of patient care make me a proficient nurse. I would place myself on the fourth stage of the Banner’s Model, as I still have many opportunities for growth.
Networking and Marketing Strategies
Job searching may become difficult for nurses who are not used to their new level of training. It is hard to realize one’s preparedness for new tasks. Moreover, one may feel as though he or she does not possess enough information about the details of finding a good job. While the role of nursing is said to become more significant in the future, ANPs can still struggle to find a position that will allow them to implement the full scope of acquired knowledge. Employment opportunities may seem scarce for individuals who do not know how to research their local job market.
It is crucial to remember that many vacancies are not published online or in print sources (DeNisco & Barker, 2015). Therefore, people get access to these open positions through referrals and connections. In this case, networking can significantly improve one’s chances of finding a suitable job opening. Nurses should engage with their local community of peers and other medical workers to acquire insight about other organizations. Professional memberships can also contribute to one’s networking, as they provide one with more information about the state of the job market. Nurses need to stay in touch with their professional contacts to maintain the relationships. Engaging in conversations and inviting people to casual and formal meetings can open vacancies that are not published elsewhere. For instance, one can start a discussion about a new study and encourage other persons to participate. Communication can happen both online and in real life.
National and local organizations encourage networking and provide their members with better opportunities for employment. For example, the AANP Job Center (2018) is an initiative of the American Association of Nurse Practitioners, which allows employers and future employees to communicate through their website. The description of vacancies on this website reveals some marketing techniques. For example, many hospitals highlight their location, describing the local landscape. Many employers discuss the high standard of living for the residents and offer various non-financial benefits to the future employees. It is possible that these strategies are meant to entice nurses to choose their job not only for the position but also for the community and location.
Conclusion
To create a viable APN professional development plan, one should acquire information about different areas of his or her future career. First of all, knowing the scope of practice is crucial as it provides one with an outlook of the future responsibilities. APNs in Florida work according to the Nurse Practice Act, which explains their duties and responsibilities. Florida has a restricted practice for nurse practitioners. One’s assessment is also essential in developing a plan for the future. In my opinion, my knowledge and range of occupations make me a competent nurse. My Curriculum Vitae showcases my skills. However, my experiences are not enough to find a successful job. It requires communication and collaboration with others. Organizations often promote networking to connect students, employees, and employers.
Curriculum Vitae (CV)
- Name: Liza R Byatt
- Home Address: 2501 Sunny Creek Dr, Fleming Island, Florida 32003
- Phone: 904-424-3744
- Email Address: [email protected]
Education
Bachelor of Science in Nursing
1995
Laguna College of Nursing
San Pablo City, Philippines
Professional Employment
2005-present
Orange Park Medical Center (Orange Park, Florida)
Staff Nurse, Relief Charge Nurse, Preceptor, Medical/Surgical Telemetry Nurse
Description: Support for patients in critical condition, monitoring of patients’ vitals and overall condition, education of other nurses based on the past experiences, administrative support.
Al Adan Hospital (Kuwait)
Staff Nurse in the Neonatal Intensive Care Unit (NICU)
Description: Care for prematurely born infants and newborns with possible medical complications.
Los Banos Doctors Hospital (Los Banos, Philippines)
Staff Nurse in the Emergency Department
Description: Administrative tasks, assessment of patients’ vitals and overall condition, medication administration, patient monitoring.
Licensure and Certifications
Registered Nurse in State of Florida
License No. – RN9226322
Validity – July 2018
PCCN – Progressive Care Certified Nurse
Certified by the AACN Certification Corporation
Validity – December 2019
ACLS – Advanced Cardiovascular Life Support
Certified by the American Heart Association
Validity – December 2019
Memberships
ANA – Member of the American Nurses Association
Public/Community Service
The Way Free Medical Clinic Inc.
Nonprofit organization providing free healthcare for the uninsured residents of Clay County Florida.
PO #3: Engage in lifelong personal and professional growth through reflective practice and appreciation of cultural diversity (Cultural Humility)
The advanced practice nurse (APN) professional development plan contributed to my skills of self-reflection and interpersonal communication. This outcome was achieved as I created a plan for my future and evaluated my current abilities, knowledge, and experience as a nurse. I acknowledged my weaknesses, such as my fear of growing responsibilities, and highlighted my strengths, including my vast practice experience and preparedness for stressful situations.
AACN MSN Essential VII: Interprofessional Collaboration for Improving Patient and Population Health Outcomes
This essential became a part of my education since I understood the role of interprofessional collaboration for personal growth and patient health. My skills are not only a personal asset but also a contribution to a bigger system of medical expertise, and team work and communication lie at the basis of creating environments for increase care quality. Thus, my individual plan recognized the importance of establishing strong relations with other members for my achievements as well as the future of health care.
NONPF Core Competency 2: Leadership
I met the objectives of this competency by acknowledging that reflective thinking is one of the ways to improve one’s personal and professional qualities. I also voiced my opinion on the current state of the job market and the necessity of contributing to professional organizations. I showed that participation in interprofessional collaboration required initiative and could help individuals and the sphere of health care as a whole.
Concepts and Reflection
Scope of practice is the set of responsibilities, actions, and procedures that a health care professional (such as an APN) can have or perform. The scope is determined by state license standards and is regulated by national organizations. In Florida, APNs work under the Nurse Practice Act, and this document defines the duties of each nurse. The practice’s restrictions in this state are vital in the discussion of my professional plan because they determine my future opportunities and training aims.
Collaboration is an important concept in nursing practice that influences patients, professionals, and the system as well. It is a meaningful interaction among health care providers that implies information exchange, experience sharing, and contribution to care delivery. Collaboration is also beneficial for job searching, systemic change, and self-improvement. Nurses who engage in team work and networking can reach out to other medical professionals, creating channels for knowledge dissemination.
The creation of my professional development plan helped me to engage in self-reflection and consider my future path in health care. I realized that I had some weak points that had to be addressed. I also saw which strengths I could use in my practice. By analyzing the scope of practice for APNs in Florida, I appraised the responsibilities and problems that I might face. Furthermore, I chose progressive adult care as the focus of my education and practice since I already possessed significant knowledge in this area. This assignment revealed my leadership competencies and underlined the role of collaboration in nursing. I used self-reflection as a tool for personal and professional improvement, connecting the knowledge about myself to the objectives and characteristics of the current practice standards.
Exemplar # 5: NR 507 Advanced Pathophysiology
Discussion
A five-month-old Caucasian female is brought into the clinic as the parent indicates that she has been having ongoing foul-smelling, greasy diarrhea. She seems to be small for her age and a bit sickly but, her parent’s state that she has a huge appetite. Upon examination you find that the patient is wheezing and you observe her coughing. After an extensive physical exam and work-up, the patient is diagnosed with cystic fibrosis.
What is the etiology of cystic fibrosis?
Cystic Fibrosis (CF) – An inherited autosomal recessive disorder caused by mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene. CFTR gene is located on chromosome 7 and regulates the hydration of epithelial cells throughout the body by controlling chloride and sodium transport. Katkin (2017) states that there are more than 1,900 possible gene defects that are further divided into six classes with differing severity with classes one through three being more severe and classes four through six being found with milder pulmonary diseases. The Cystic Fibrosis Foundation (2018) state CF is attributable to 90% of all childhood pancreatic diseases and can affect other organs, but the most common cause of death is related to lung disease. CF affects 1 in 3,000 Caucasians, 1 in 9,200 Hispanics, 1 in 10,900 Native Americans, 1 in 15,000 African Americans, and 1 in 30,000 Asian Americans (Katkin, 2017). The mean survival rate of CF is 40 years of age (Van Biervliet et al., 2016).
Describe in detail the pathophysiological process of cystic fibrosis
The “cystic fibrosis transmembrane conductance regulator (CFTCR or CFTR) gene mutation results in the abnormal expression of cystic fibrosis transmembrane conductance regulator protein, which is a cyclic adenosine monophosphate (cAMP)-activated chloride channel present on the surface of many types of epithelial cells including those lining the airways, bile ducts, the pancreas, sweat ducts, and the vas deferens” (McCance et al., 2014, p. 1311). Abnormalities with the transportation of electrolytes across the cell membrane, affects the secretion of chloride and sodium in the sweat and abnormal thick secretions in the lungs, pancreas, and reproductive organs (Lawton & Schub, 2015).
McCance et al. (2014) also state the goblet cells and submucosal glands which are the mucus-secreting airway cells and increased in size and number and that an increased chloride excretion and sodium absorption bring about dehydration of the airway mucus that enhances the thick mucus that adheres to the epithelium making it hard to cough up the secretions and thusly encourages growth of bacteria. McCance et al. (2014) also report inflammation as evident by increased amount of IL-1 and Il-8 and state long-term damage is done to the respiratory system due to substantial amounts of neutrophils releasing oxidants like proteases which breaks down proteins like elastin and entice airway cells to produce IL-8 which attracts more neutrophils which means more inflammation and a vicious cycle. This protease also destroys IgG and components necessary for opsonization and phagocytosis and stimulates the mucus cells to make more mucus (McCance et al., 2014). Every individual has two CF genes called the cystic fibrosis transmembrane conductance regulator (CFTR) and that person must receive two copies of the CFTR mutated gene to have CF (CCF, n.d.).
Identify hallmark signs identified from the physical exam and symptoms
The patient is 5 months old (the median age at diagnosis is 6 months), is experiencing greasy, foul-smelling diarrhea, poor weight gain even though there is a good appetite, coughing, and wheezing, which are classic symptoms of CF. Patients may also display a variety of symptoms from salty-tasting skin, dyspnea, clubbing, and stools can range from greasy to difficulty in having bowel movements (CFF, n.d.).
Describe the pathophysiology of complications of cystic fibrosis
Most commonly the CF genetic mistake is the DF508 protein that results in hypochloremia that progresses to lung issues related to thick mucus which inhibits proper air exchange that leads to infections, lung damage, and ultimately respiratory failure (CFF, n.d.). The CFF (n.d.) state CF is attributable to 90% of all childhood pancreatic diseases and can affect other organs, but the most common cause of death is related to lung disease. CFF (n.d.) state the malnutrition and poor growth issues with CF patients are due to the mucus build up in the pancreas that interferes with food and nutrient absorption; therefore, treatment is aimed at therapy to clear airways, and pancreatic enzyme supplements to improve absorption of nutrients. There is also a high risk of chronic endobronchial infection with children. Bacteria such as Staphylococcus aureus, Pseudomonas aeruginosa and Burkholderia cepacia are prone to colonize in the lung which makes antibiotics difficult to reach them. Chronic problems related to CF include; bacterial infections in the lungs, obstructive pulmonary disease due to decreased mucocillary clearance, malnutrition from pancreatic insufficiency and failure to thrive.
What teaching related to her diagnosis would you provide the parents?
Cystic fibrosis treatment and teaching depends on the stage of the disease. I will advise the parents the importance of breathing exercises, percussion and postural drainage techniques. I will also review the need to avoid known respiratory irritants such as smoke and air pollutants and persons with upper respiratory infections. The child may have trouble breathing when she lies flat, so I will instruct the mother to elevate the child’s head when she sleeps and use a cool mist humidifier to increase air moisture in the home. This may make it easier for the child to breathe and to cough up mucus. An enriched diet with vitamin and enzyme replacement to help maintain body weight will be added to her plan of care. And as far as medication, I will encourage the parents to continue giving the Antibiotics to treat and prevent lung infections and medicines to thin the mucus.
PO #1: Provide high quality, safe, patient-centered care grounded in holistic health principles (Holistic Health & Patient-Centered Care)
The first Chamberlain program outcome is concerned with nurses’ ability to engage in patient-centered care. The assignment discussing the case of cystic fibrosis gave me an opportunity to examine the condition and provide the patient’s parents with knowledge about the diagnosis. Thus, I focused on the information that is important to them and their child, informing them about possible treatments and ways to alleviate the patient’s pain and discomfort. The holistic care approach urged me to address the patient’s specific needs, especially her young age which complicated the diagnosis and treatment processes. Thus, I addressed the parents and described the signs of cystic fibrosis that could be understood without the patient’s contribution (which could be helpful in adult patient situations).
AACN MSN Essential IX: Master’s-Level Nursing Practice
To meet the ninth essential of Masters-level practice, I aimed to employ my knowledge in practice for this assignment. I considered my experience with cystic fibrosis cases as well as available theoretical information to come to the diagnosis. Then, I researched the ways in which the most vital information should be delivered to the parents. The ability to understand how patients may interpret information is a part of Masters-level nursing skills. Indirect care components included m research about the signs of cystic fibrosis and the review of the condition’s pathophysiology. Direct care in this assignment was performed through patient and caretaker education. My understanding of nursing, relevant sciences, and communication strategies assisted me in completing this assignment.
Concepts and Reflection
Teaching is a combination of facts, practices, and approaches that APNs often need to relay to patients or their caretakers to ensure their understanding of an issue. Nurses often teach patients and their relatives to recognize the signs of worsening, treat symptoms, or prevent complications. Teaching may include general tips for a lifestyle change, ways to take medications, diet suggestions, and other strategies to improve one’s health.
Pathophysiology is a process of a disease’s progression that demonstrates how a condition develops and evolves in one’s body. The understanding of the pathophysiology is vital for diagnosis and treatment since it explains the responses of the body to different factors. In this case, the pathophysiology of cystic fibrosis showed which signs point to the correct diagnosis. In infants, the knowledge of pathophysiology is essential to one’s ability to detect a problem since young children cannot describe their feelings. Thus, it contributes to a nurse’s duty of providing high-quality care.
The assignment investigating the case of a young child with cystic fibrosis helped me to integrate my theoretical knowledge, communication skills, and practical experience to deliver patient-centered care. I had to consider the different levels of information available to me as an APN. I integrated a variety of sciences and discussed the pathophysiology of cystic fibrosis as a part of making a diagnosis. I also needed to translate my academic knowledge into practice and teachings for the patient’s parents. Nurses’ duties include educating patients and their caretakers about their health. Thus, the skill of explaining complex data in simple terms is a part of Masters-level nursing practice as much as the ability to use theory in practice.
Exemplar # 6: NR 508 Advanced Pharmacology
Advanced Pharmacology: Claudia’s Case
26-year-old Claudia asks for professional help to prevent her pregnancy after giving birth to two children. In the past, she used condoms and oral contraceptive pills. Now, she wants to use a more reliable birth control method, avoiding sterilization. She has a mild hypertension history during her first pregnancy. This time, she needs effective treatment with clear goals and methods being identified.
Treatment Goals
Today, millions of women aim at controlling and preventing their pregnancies. For example, in the USA, more than 50% of unintended pregnancies with 40% of them ended in abortions and other unpredictable health problems (Birgisson, Zhao, Secura, Madden, & Peipert, 2015; Curtis & Peipert, 2017). Claudia wants to avoid such problems. The main treatment goals for Claudia today may vary. They include learning the options concerning pregnancy prevention, taking tests to check the current condition of the body, and evaluating her emotional state to make sure that no panic or anxiety disorders influence her decision. It is also important to gather clinical and social information about the patient (Gavin et al., 2015). Finally, the necessary goal is to choose a method that does not provoke any allergies or other health changes in the patient.
Contraceptive Methods
Contraception is not only a method to avoid pregnancy. According to the guidelines given by the Center for Disease Control and Prevention, it is a good chance for women and men to place and space birth, prevent unwanted health conditions, and reduce the number of abortions (Gavin et al., 2015). Possible contraceptive methods for Claudia are the use of an intrauterine device (IUD) or oral contraceptive pills. The rationale for IUD is the possibility to control birth without the partner’s participation and the necessity to visit a doctor just once for the device to be implanted. As a rule, 100% guarantee to avoid pregnancy is given. Among the existing variety of methods, IUDs remain the most cost-effective options for millions of women. Though IUDs are 20 times as effective as pills (Curtis & Peipert, 2017), oral contraception is still an option for Claudia. This method can be approved as it is a good chance to regulate menstruation and relieve menstruation-related pain. Many women find it comfortable to use pills. Finally, the use of pills may reduce the risk of having inflammation processes.
Patient-Centered Teaching Points
In case Claudia chooses IUDs, she has to be ready for several important lessons. First, a medical worker should inform her about the presence of hormonal and non-hormonal types of IUDs. The second teaching point is the length of its possible usage. As a rule, hormonal devices have to be replaced in 3-5 years, and non-hormonal in 10 years. The next important issue is that IUDs do not protect against sexually transmitted diseases. Therefore, the patient has to take care of her health with the help of condoms. Another lesson is based on its location. It is placed directly in the patient’s vagina and can slip out. Finally, menstrual cramps may be either increased or decreased, depending on her health peculiarities. A doctor has to inform about these possible changes beforehand.
Contraceptive Choice for a Smoker
In case the patient smoked 10-15 cigarettes per day, it would be suggested to avoid any contraception methods that contained estrogen or other hormones that could increase risks of blood clot complications. Heart attacks and strokes can be other unpleasant outcomes of birth control for smokers (Gavin et al., 2015). The best alternative can be a non-hormonal IUD.
AACN MSN Essential II: Organizational and Systems Leadership
The case of Claudia assisted me in exercising my leadership skills in relation to ethical practice and safe patient care. Nurses’ leadership opportunities arise in all areas of practice, including the decision-making process. Claudia’s situation raised the question of the most suitable contraception strategy that would preserve the patient’s health, avoiding dangerous and unreliable methods. Therefore, as a nursing leader, I had to use my expertise to provide the patient with potential solutions. I also acknowledged the patient’s personal risks (smoking) as a factor in informing her about available options. Exercising my knowledge and my leadership skills, I was able to suggest the most cost-effective, reliable, and safe option for the patient.
NONPF Core Competency 8: Ethics
The competency area of ethics implies that nurses assess the consequences of all healthcare-related decisions and consider ethical solutions for problems (NONPF, 2017). In advising the patient, I reviewed previous research about different contraception approaches. I addressed the risks of each method and the consequences that the patient might encounter using each of them. As a result, my decision to recommend a non-hormonal IUD was informed by clinical studies and available data. The consideration of the patient’s past experiences, personal wishes, and future changes also affected my choice. My attitude towards the patient’s decision and my care were influenced by my commitment to ethical principles of care. Furthermore, my suggestions were in line with the legal statutes. I also acknowledged the patient’s culture and needs in discussing contraception, as this question may be sensitive for some communities.
Concepts and Reflection
Patient-centered care is a concept that lies at the foundation of contemporary nursing. According to the standards of this approach, patients’ views on their wellbeing as well as their faith, wishes, fears, and culture have to be acknowledged in the process of care delivery. Thus, patient-centered treatment does not always depend only on the decisions of medical professionals, and patients have a level of authority in choosing treatment options.
Ethical principles in nursing constitute a number of rules that any nurse should consider when making decisions and exercising authority. Some of these principles are autonomy, nonmaleficence, beneficence, and justice. For instance, nonmaleficence implies that nurses should do no harm to patients. In this case, the correct choice of a contraceptive method had to be selected on the base of minimal risks and side effects.
Apart from widening my experience with adult patients, this assignment also helped me to exercise ethical decision-making. Patient-centered care implies that the patient’s specific needs have to be addressed while allowing this person to have a level of independence and freedom of choice. Thus, I had to focus on informing Claudia about the ways in which her issue can be solved to reduce negative consequences. As an APN, I had knowledge that patients do not usually possess, and it was my duty to frame it in a way to help the patient make a decision. Here, my leadership qualities and experience supported my care delivery and guided my actions. I also applied the principles of ethical nursing to the case in order to provide safe care.
Exemplar # 7: NR 509 Advanced Physical Assessment
Respiratory System Assessment: A Case Analysis
Respiratory System: Description
The human respiratory system (RS) is known as the system of organs that allows obtaining oxygen from air, delivering it to the necessary organs, and exhale carbon dioxide (CO2). The RS consists of lungs, which maintain the continuous flow of oxygen and remove gaseous products from the human body (Kon & Rai, 2016). The RS also contains the airways, which are categorized into lower and upper ones, and which serve the purpose of pumping air, whereas the oxygen that it contains is delivered to specific organs with the help of red blood cells (Kon & Rai, 2016). Despite the clockwork mechanism of the system, the RS is rather fragile since its performance can be disrupted once airways are blocked. The resulting experience of problems breathing and even possible suffocation may cause severe consequences from oxygen deprivation to death (Kon & Rai, 2016). Therefore, the case under analysis, which involves seemingly minor concerns, particularly, cough, needs an in-depth analysis.
Physiology: Structure and Function
The upper respiratory tract consists of the nasal cavity, nostrils, pharynx, epiglottis, and larynx (Boore, Cook, & Shepherd, 2016). The lower respiratory tract, in turn, is composed of trachea, esophagus, pulmonary vessels, intercostal muscles, left and right lungs, heart, bronchioles, pleural membrane, alveoli, and the diaphragm (Boore et al., 2016). During the process of breathing, oxygen (O2) is converted into CO2. The latter, in turn, is transformed to HCO3 when transported from tissue cells to lungs (Ward, Ward, & Leach, 2015). The process of HCO3 creation occurs as CO2 emitted from lungs is combined with H2O to produce carbonic acid (H2CO3). The latter decomposes into HCO3 and H+ ions. The specified process is known as peripheral control, which is opposed to the central control.
Relevant Health History Questions
The current information concerning the health status of the patient does not allow making clear assumptions and diagnosing the problem. Therefore, a detailed assessment of the patient’s health history will be required. It is currently known that the patient is eight years old boy and that he has had a cough for five days. However, the root causes of the specified symptoms may vary from a minor respiratory inflammation caused by an infection to the early stage of asthma development. Therefore, further steps will have to be taken to determine the cause of the patient’s current condition. To define the factors that may have caused the cough, one may need to ask the patient or his mother the following questions:
- Does the child have any known allergies?
- Has the child been diagnosed with respiratory diseases such as asthma?
- Has the child been exposed to cold recently?
- When did the cough start?
- What was the child doing when the cough started?
- How can you describe the cough?
Objective Data and Expected Findings
Apart from relying on the evidence provided by the patient, a therapist will also have to perform several tests to locate the actual cause of the cough. For this purpose, the characteristics of cough must be defined. For example, it will be necessary to check whether the cough is dry or productive. In addition, chest X-ray will allow determining whether the problem is caused by lung obstruction. Pulmonary function tests (PFTs) can be useful in case the problem turns out to be chronic (Sharafkhaneh, Yohannes, Hanania, & Kunik, 2017). Bronchial challenge testing and sinus imaging will have to be deployed if other methods of determining the problem prove to be futile. It is expected that the results of the patient assessment will point to a respiratory inflammation possibly caused by an infection.
Physical Assessment Examination Techniques
As stressed above, a physician may need to run several tests to determine the factors that may have caused the issue. However, apart from the specified strategies, one will also need to use specific examination techniques. For example, the vital signs of the patient must be assessed. In addition, a physician will have to revise all of the patient’s systems to ensure that the cause of the cough has been determined correctly and that no other factors affect its development. The specified step will have to be followed by the examination of the patient’s Head, eyes, ears, nose, and throat. In addition, a therapist will need to examine the patient’s neck and cardiovascular system to locate possible factors that may cause the cough.
Finally, chest examination as the most important step in the specified assessment process will be performed. The therapist will inspect and palpate the patient’s chest to locate the reasons for the cough to take place. The nurse practitoner will also have to evaluate the percussion of the lung fields along with the possible auscultation of the lungs. The specified checks will allow identifying the presence of wheezing, chest vibrations, and other characteristics of pulmonary obstruction that will allow defining the problem.
Physical Assessment Skills
To conduct the assessment, the nurse practitonert will have to use basic skills associated with the management of respiratory issues. Specifically, active observation will have to be used to identify the presence of a problem and explore its nature. In addition, a therapist will require the ability to calculate the respiratory rate of the patient, examine his nasal cavity, and locate the presence of breathing problems such as wheezes and forced exhalation. The specified skills can be used to accommodate the needs of infants by taking the fact that their airways are smaller into consideration. To manage the needs of pregnant women, one will have to assessing abdominal muscle thickness as well. Finally, to address the health concerns of geriatric patients, one will need to consider the issues of comorbidity and frailty. Thus, a comprehensive assessment will be conducted.
Disease That Can Affect the Respiratory System
As stressed above, there is a range of diseases and disorders that may have caused the cough that is currently observed in the patient. Among the most common causes of the cough, one should mention asthma, common cold, and chronic obstructive pulmonary disease (COPD). The latter represents a combination of health issues that cause breathing issues (Boore et al., 2016). Therefore, the RS may have been affected by a vast variety of factors, and further tests will help to locate the actual cause of the cough.
Expected Abnormal Findings
The tests are most likely to return the results that will signify the presence of an infection, a common cold, or an allergic reaction that the patient must have suffered recently. The exposure to allergens may have triggered the fast development of the disease and, thus led to an unceasing cough. However, other causes of the problem may also be discovered in the course of the assessment since the current information is far too scarce to state the problem with certainty.
Summary
The case of a cough that was analyzed above lacks the data that could help define the presence of a particular issue straightaway. Thus, a nurse practitoner must perform further assessments to locate the cause of the issue and suggest the medications and treatment techniques that will help the patient. It is believed that the patient may have developed a common cold, asthma, allergic rhinitis, or another respiratory issue that may have caused the problem to emerge. In any scenario, a detailed assessment of the patient’s health history and a profound analysis of test results are required.
AACN MSN Essential V: Informatics and Healthcare Technologies
In this assessment of the respiratory system, I reviewed the importance of health care technologies and communication technologies in delivering care. I noted the lack of previous data about the patient, which further highlighted the importance of using contemporary resources for care. I highlighted that the evaluation of various tests is necessary for a correct diagnosis, which can be assisted with electronic resources and medical records. The present scenario, similarly to any other situation, requires a close examination from an APN. Here, the technology that captures and preserves data is valuable since it allows one to get access to previous records.
NONPF Core Competency 1: Scientific Foundation
Danny’s case required one to know the specifics of assessment and testing for various respiratory conditions. As a result, I had to utilize my knowledge of different methods in order to gather enough data to come to a definitive diagnosis. The basics of physical assessment techniques were helpful in investigating the patient’s condition. I had to integrate the objective data into diagnostics to understand what findings I should expect.
NONPF Core Competency 5: Technology and Information Literacy
The assignment demonstrated that the technical information from diagnostics and available scientific information play a significant role in developing treatment plans for patients. Thus, it is one of the nurse’s duties to translate this data into practice and tailor it to patients’ needs. I achieved this competency by perfecting my information literacy skills and supporting the integration of technologies for data management.
Concepts and Reflection
Physical assessment is the set of procedures that health care professionals perform to collect information about the patient’s current condition and determine particular issues that require attention. Physical assessment is an integral part of any office visit, and it contributes to diagnosis and treatment development. It also serves a purpose in data gathering – the results of assessments can be recorded in a database for future appointments and patient statistics.
Health history is all information available to the practitioner about the patient’s wellbeing. It may include previous illnesses, surgeries, medications, pregnancies, births, and vaccinations. Moreover, nurses can collect additional data about patients during examinations by asking questions and recording the results of diagnostics. Health history contributes to clinicians’ diagnosing process and determines the arguments supporting one condition over others. In this case, the lack of health history prevented me from coming to a conclusive diagnosis, presenting a multitude of possible conditions instead.
The examined case showed the value of information literacy in nursing. As an APN, I should recognize the importance of data and previous findings as well as the potential for gathering more information about each case for improving care. The lack of data can significantly impair the quality of nurses’ performance, and its collection is an essential part of patient treatment. Thus, one can highlight the role of technology in health care. The failure to recognize the need for sufficient knowledge about patients can lead to incorrect diagnoses and missed care.
Exemplar # 8: NR 601 Primary Care of the Maturing and Aged Family Practicum
Diabetes Management
The purpose of this paper is to analyze the provided subjective and objective information to diagnose and develop a management plan for the patient in the case study. The paper intends to apply national diabetes guidelines to the management plan. The mastery of SOAP note writing will also be demonstrated.
Assessment
Primary Diagnosis
Type 2 diabetes mellitus (E11.9). Pathophysiology
Type 2 diabetes is an endocrine and metabolic disorder that arises due to acquired resistance to insulin action or loss of function of pancreatic beta cells that produce insulin, which is responsible for the metabolism of glucose. Inadequate regulation of blood sugar levels causes hyperglycemia that often leads to the manifestation of the classical symptoms of diabetes mellitus, including include polyphagia, polyuria, and polydipsia (American Diabetes Association [ADA], 2018).
Pertinent positive findings
The patient reports that she has experienced increased fatigue for the last 12 weeks, frequent urination and weight gained despite her efforts to exercise. She also experiences extreme thirst and hunger after exercise, which complicates her weight loss process. Therefore, the patient presents with the classical symptoms of diabetes mellitus: polyphagia, polyuria, and polydipsia, which confirms this diagnosis (Acuna, Labinson, & McDermott, 2017).
Additionally, the laboratory tests are indicative of type 2 diabetes. The urinalysis shows glycosuria, whereas the blood glucose level is elevated at 130mg/dl, which is a symptom of hyperglycemia. Hemoglobin A1C level is 6.8 %, which is a symptom of type 2 diabetes (Chatterjee, Khunti, & Davies, 2017). Normal levels of glycated hemoglobin should be 5.7% and below, whereas hemoglobin A1C between 5.7% and 6.4% show prediabetes (American Diabetes Association [ADA], 2018).
Pertinent negative findings
Urine tests are the most reliable way of detecting ketones and microalbumin. The urinalysis did not indicate the presence of ketones or protein, which are usually present in severe hyperglycemia (Fayfman, Pasquel, & Umpierrez, 2017).
Rationale for the diagnosis
ADA (2018) recommends that type 2 diabetes should be diagnosed based on the three classical symptoms of diabetes with additional backing from laboratory tests. The diagnosis was made based on the presenting symptoms (polydipsia, polyphagia, and polyuria), high fasting blood glucose levels, the presence of glucose in urine, fatigue, and unexplained weight gain despite exercise. BMI of 31.17 is an indication of obesity, which is a known risk factor for type 2 diabetes mellitus. These findings confirmed the diagnosis of type 2 diabetes.
Secondary Diagnosis
Hyperlipidemia (E78.5). Pathophysiology
Hyperlipidemia refers to the presence of high levels of lipids in the blood, which arises from the consumption of food items that are rich in fats thereby increasing the amount of lipids that are circulating in the blood (Navar Boggan et al., 2015). Hyperlipidemia does not have any distinctive symptoms and can only be diagnosed by conducting a lipid panel.
Pertinent positive findings
Total cholesterol of 215 mg/dl (less than 200 ng/dl is desirable), LDL of 144 mg/dl (less than 100 mg/dl is optimal); VLDL 36 mg/dl (normal range is 2 to 30 mg/dl); HDL 32mg/dl (levels of 40 mg/dl is desirable), and triglycerides 229 (200 mg/dl and above is considered high) (ADA, 2018).
Pertinent negative findings
The patient had normal blood pressure values despite having elevated lipid levels. Cholesterol could accumulate in the inner walls of the blood vessels thus elevating blood pressure in the affected individuals (Rafieian Kopaei, Setorki, Doudi, Baradaran, & Nasri, 2014). However, in the case study, the patient had normal blood pressure values. In addition, hyperlipidemia could occur due to the consumption of a high-fat diet and hypothyroidism. However, the thyroid function test as indicated by the TSH and free T4 values were within the normal range. TSH was 2.31 (normal range is 0.35 to 5), whereas the free T4 was 0.9 ng/dl (normal range 0.7 to 1.9 ng/dl).
Rationale for the diagnosis
The lipid profile showed elevated levels of cholesterol, LDL, VLDL, triglycerides, and low levels of HDL, which are the main indicators in hyperlipidemia diagnosis (Rafieian-Kopaei et al., 2014).
Differential Diagnosis
Metabolic syndrome (E88.81). Pathophysiology
Metabolic syndrome is an array of risk factors attributed to insulin resistance. The typical symptoms include abdominal obesity, elevated fasting blood glucose, high triglyceride levels, high blood pressure, and low levels of LDL (Furukawa et al., 2017).
Rationale for the diagnosis
The patient presents with all these symptoms except high blood pressure, which is why this disorder is considered a differential diagnosis (Furukawa et al., 2017).
Adjustment disorder with depressed mood (F43.21)
Pathophysiology
Depression is a psychological disorder that is attributed to numerous causes and interaction of factors that interfere with the balance of essential neurotransmitters such as dopamine, serotonin, and norepinephrine or significant changes in the life of an individual (O’Donnell et al., 2016). The indications of depression may include fatigue, changes in appetite, mood changes, feelings of disappointment and frustration, and disturbed sleep.
Pertinent positive findings
Mrs. Wu is frustrated about her weight gain and the need to pass urine frequently, which affects her sleep. She was recently diagnosed with knee arthritis and has had to deal with pain and difficulties walking, which can be considered a significant life change (O’Donnell et al., 2016).
Pertinent negative findings
Mrs. Wu does not have a significant hormonal change. She underwent menopause 4 years ago and has currently adjusted to the hormonal modifications associated with menopause, which rules out the likelihood of hormonal involvement in depression (Albert, 2015).
Rationale
This diagnosis was chosen because Mrs. Wu experiences fatigue and weight gain despite her efforts to lose weight, which could contribute to depression. Her attempts to exercise are frustrated by her hunger and thirst pangs, particularly after exercising. She is also unhappy about the fact that she has to use the bathroom more than usual, which at times interrupts her sleep. This diagnosis may not be adequate to account for the observed signs and symptoms. However, it should be considered when treating the patient (O’Donnell et al., 2016).
Plan
Diagnostics
Spot urinary albumin-to-creatinine ratio
Rationale: For additional assessment of renal function. The test should be conducted every year together with eGFR. Diabetes mellitus, which is associated with high blood glucose levels, damages kidneys over time and causes diabetic nephropathy (ADA, 2018).
HgbA1C test
Rationale: Hemoglobin A1C test is used to measure the average blood glucose levels over 3 months to determine the effectiveness of glycemic control. The findings help clinicians to decide whether there is a need for adjustments in the patient’s treatment (ADA, 2018). This test should be conducted every three months until normal levels are attained.
Annual fasting CMP
Rationale: This test assesses fasting blood glucose and electrolyte levels. Assessment of liver functioning should be done yearly because Metformin is contraindicated in instances of decreased liver function (ADA, 2018).
Foot exam
Rationale: To evaluate foot health because diabetic foot ulcers are among the most common complications in diabetic patients. Persistently elevated blood glucose levels often lead to vascular and nervous problems, which in turn lead to peripheral neuropathy and foot ulcers (Armstrong, Boulton, & Bus, 2017). A thorough foot exam is required for the patient and should include a detailed skin inspection: checking for foot defects, neurological assessment using a 10-g monofilament and a temperature or pinprick exam. The monofilament test should be conducted yearly. Additionally, a vascular evaluation of the feet should be done. Mrs. Wu should have a brief foot inspection at every subsequent to facilitate the prompt diagnosis of peripheral neuropathy and avoid the need for amputations in the future (ADA, 2018).
Lipid profile
Rationale: Repeat lipid profile tests should be done t least three months following the commencement of statin therapy to monitor the efficacy of the treatment. The lipid profile would also ascertain that Mrs. Wu is receiving the correct dosage of atorvastatin dosage and prompt necessary adjustments as the need arises (ADA, 2018).
Becks Depression Inventory
Rationale: Depression and diabetes mellitus are two commonly co-occurring disorders in primary care. Healthcare providers in primary settings are mainly responsible for the diagnosis and management of these two disorders. Consequently, affected patients do not get the opportunity to receive specialized care. The occurrence of depression in diabetes has a negative effect on glycemic control and is linked to the development of diabetic complications (Semenkovich, Brown, Svrakic, & Lustman, 2015). Nonetheless, it is often untreated, which could be attributed to the fact that most symptoms of depression such as changes in appetite, excess weight loss or gain, fatigue are often associated with diabetes. Therefore, it is not easy to confirm whether these symptoms are due to diabetes or depression. Diabetes patients should undergo screening for depression to enable the commencement of well-timed intermediations.
Health maintenance
Advancing age is a risk factor for many diseases in women, including type 2 diabetes mellitus, breast cancer, and colorectal cancer. The United States Preventive Service Task Force [USPSTF] (2016) recommends that women between the ages of 50 and 74 years undergo annual mammograms. Since Mrs. Wu’s last annual mammogram was normal, she should be reminded to schedule her next appointment. ADA (2018) recommends that diabetic patients should be vaccinated against influenza, Hepatitis B, and pneumococcal diseases. The patient’s immunizations are up-to-date. However, she should be reminded to honor her upcoming vaccinations.
Medications
Type 2 diabetes mellitus
- Metformin 500 mg tablets (Extended-release)
- Sig: Take 1 (one) tablet twice every day with food. Disp: #30. RF: 0
- Diabetic Lancets
- Sig: Test blood glucose BID, more frequently as needed. Disp: 200 (2 boxes). RF: 2
- Glucometer
- Sig: Test blood glucose BID, more frequently as needed. Disp: 1 kit. RF: 1
- Glucagon Emergency Kit
- Sig: Inject 1mg IM as directed. Disp: 1 kit. RF: 2
- Test strips
- Sig: Test blood glucose BID, more frequently as needed. Disp: 100 (1 box). RF: 2
- Multivitamin (over-the-counter)
- Sig: Take 1 (one) tab daily
Rationale
Mrs. Wu will receive a prescription of oral Metformin, which is the recommended first-line pharmacological treatment for type 2 diabetes in symptomatic patients with HbA1C levels less than 9% and eGFR that is greater than 99 mL/min/1.73 (ADA, 2018). Metformin works by lowering hepatic production of glucose, increasing the uptake of glucose in the small intestines, and enhancing insulin sensitivity, which ultimately boosts the uptake and utilization of peripheral glucose. An additional benefit of metformin is the capacity to reduce LDL cholesterol, which could help in weight loss and hyperlipidemia. The initial dose of extended-release metformin will be 500 mg, which can then be increased to an upper limit of 2000 mg daily until the desired blood glucose level is attained.
Sometimes, the management of blood glucose levels may lead to inadvertent hypoglycemia, which may be life-threatening. Emergency glucagon kits are important for diabetics for such eventualities (ADA, 2018).
The management of blood glucose levels in diabetes involves obtaining regular measurements of blood glucose. Therefore, Mrs. Wu will require a glucometer, lancets, and test strips. Studies show that the long-term use of metformin in the management of blood glucose results in vitamin B12 deficiency, which manifests as peripheral neuropathy in approximately one-third of patients using this drug (Niafar, Hai, Porhomayon, & Nader, 2015; Aroda et al., 2016). Therefore, it is necessary to avoid this consequence by administering multivitamins to patients on metformin (ADA, 2018).
Hyperlipidemia
Atorvastatin 10mg tablets.
Sig: Take 1 (one) tab daily. Disp: #30. RF: 0.
Rationale
ADA (2018) recommends statins as the drug of choice in the reduction of blood cholesterol levels as well as cardioprotection in diabetic patients. Atorvastatin is the most commonly used drug for this purpose. However, its effectiveness in reducing LDL levels depends on the dose administered. At doses of 40 to 80 mg, high-intensity therapeutic effects are observed by at least 50% reductions in LDL cholesterol levels. However, at doses of 10 to mg, moderate effects are noted in the form of 30 to 50% reductions in LDL cholesterol. In this case, a 30 to 50% reduction would bring down the LDL cholesterol levels to the normal range.
Osteoarthritis
Acetaminophen 500 mg tablets (over-the-counter).
Sig: Take 1 (one) tab every 4-6 hours when needed for pain. Do not exceed 4000mg in 24 hrs.
Rationale
Arthritis is a long-term condition without a permanent cure. Therefore, its management involves the management of associated symptoms such as pain and swelling, as well as improving mobility. Nonsteroidal anti-inflammatory drugs (NSAIDs), analgesics, corticosteroids, and hyaluronic acid are commonly used to manage pain and inflammation in arthritis (Arthritis Foundation, 2018). Acetaminophen is an endorsed first-line medication for the pharmacologic management of osteoarthritis of the knee, which may be desirable for diabetic patients on metformin because acetaminophen has minimal gastric effects. Alternative medications will be considered if she no longer obtains relief when using acetaminophen.
Education
Diagnoses
Type 2 diabetes
The management of type 2 diabetes mellitus encompasses a combination of pharmacological and non-pharmacological interventions. Therefore, the patient should receive education on these two aspects. The effectiveness of these interventions depends on the patient’s adherence to the treatment regimen. There is a need to provide self-management education in addition to problem-solving skills for all facets of diabetes management (ADA, 2018).
The medical provider should consider the patient’s preferences, values, and goals when developing a diabetes management regimen. Pharmacological interventions in type 2 diabetes include taking medications as recommended, whereas non-pharmacological intermediations include healthy diets, regular exercise, and blood sugar monitoring. Mrs. Wu should be educated on checking her blood sugar levels, including how to use the prescribed test kit, lancets, and glucometer. For insulin-independent diabetes, the frequency of blood sugar checks is less than in type 1 diabetes. The initial recommendation based on ADA (2018) is to check blood sugar at least twice a day (in the morning and before going to bed). She should also strive for HbA1C levels of 5.7% or less, fasting blood glucose of 80 to 130 mg/dL, postprandial blood glucose less than 180 mg/dL, and bedtime levels of 90 to 150 mg/dL (ADA, 2018). It is also important for the patient to be aware of the impact of stress and dehydration on her blood glucose levels and the need to check the sugar levels at those times.
Hypoglycemia is a possible complication in diabetes. Therefore, Mrs. Wu should be educated about the symptoms of hypoglycemia, for example, irritability, wobbliness, tachycardia, confusion, and hunger. She should be advised to check her blood glucose whenever she experiences these symptoms and act appropriately. For instance, blood glucose readings of 70 mg/dl or below warrants the intake of 15 to 20 g of glucose. Readings less than 54 mg/dl necessitate the use of glucagon. There is a likelihood that she may become unconscious once her blood sugar reaches these levels. The patient should recheck her blood glucose level following 15 minutes of oral glucose or glucagon injection and act accordingly based on the previous recommendations. Once her sugar levels have been stabilized, she can eat a meal or a snack to aver another incident of hypoglycemia. It is important to educate the patient about possible triggers for hypoglycemia, for example, intense exercise, fasting, and delayed meals. Small snacks and sweets are handy in such situations.
The patient should also be educated on important aspects of foot care, for example, regular examination of her feet for any signs of injury. She should seek medical treatment promptly for treatment if she notices any injury. Diabetic retinopathy is a possible complication in diabetes. Therefore, the patient should report any alterations in vision and see an optician regularly (ADA, 2018).
The patient should receive education on the interactions between hypertension and renal function in diabetes. Hyperlipidemia also increases her risk of cardiovascular events. Even though her current blood pressure was within the normal range, she should strive to maintain it that way to reduce her risk of chronic renal disease and cardiovascular disease (ADA, 2018).
Hyperlipidemia
Mrs. Wu should be educated about the importance of lowering her cholesterol levels. Hyperlipidemia predisposes her to the development of atherosclerosis and other cardiovascular diseases. Apart from taking her medications as recommended, the patient needs to watch her diet by cutting down the consumption of fatty foods, reduce her caloric intake, and exercise regularly. She should strive to attain LDL levels less than 70 mg/dl (ADA, 2018).
Depression
Mrs. Wu was educated about the signs of depression and advised to seek medical assistance if she experienced those symptoms. She was informed that it was normal to feel overwhelmed by the new diagnosis. She would be required to make significant modifications to her lifestyle. These factors would increase her risk for depression, which would hamper her glycemic control goals if not addressed (ADA, 2018).
Medications
Metformin
The patient was informed about the mode of action of metformin and advised to take it with food, especially in the evenings to prevent hypoglycemia. She was also informed about the side effects of the drug, which include queasiness, weight loss, and diarrhea. She should not be alarmed by these symptoms and should continue taking the drug because gastrointestinal indications would resolve on their own (McCreight, Bailey, & Pearson, 2016).
Glucagon
Mrs. Wu was taught how to use the glucagon kit. She was also asked to educate her family and close friends on how to do the same in the event that she fell unconscious due to hypoglycemia. She was asked to have the kit with her at all times and discard it if it expires. She was also informed about the correct storage of the kit, which was at room temperature away from extreme temperatures.
Atorvastatin
Atorvastatin can cause side effects such as muscle weakness and myalgias (Ramkumar, Raghunath, & Raghunath, 2016). The patient was informed about these possibilities and asked to seek medical help promptly if she experienced them.
Acetaminophen
The patient was asked to ensure that she did not exceed the maximum daily limit of acetaminophen. She was advised against taking other medications that contained acetaminophen, for example, over-the-counter drugs for cold and flu. An overdose of acetaminophen could cause liver toxicity (Kheradpezhouh, Ma, Morphett, Barritt, & Rychkov, 2014).
Diet
ADA (2018) recommends that diabetic patients should take the Mediterranean diet. Mrs. Wu was asked to watch her diet by reducing the consumption of foods rich in saturated and trans-fats. She should also reduce her carbohydrate portions but increase the intake of omega fatty acids and fiber. This diet would help in the glycemic control and reduction of cholesterol levels.
Exercise
The patient was advised to increase her physical activity to 30 to 60 minutes at least 4 to 6 times a week (ADA, 2018). However, given her knee arthritis, she was advised to engage in mild to moderate exercise. She was asked to check her blood glucose after exercising.
Warning signs for diagnoses and medications
Apart from the indications of hypoglycemia that have already been mention in the previous sections, the patient should also watch out for the indications of hyperglycemia. They include blurred vision, difficulties concentrating, extreme fatigue, and blood sugar that exceeds 180 mg/dl (ADA, 2018). Other warning signs include tingling and numbness of feet as well as slow healing of cuts and wounds. She was also asked to seek urgent medical help if she developed intense abdominal pain, respiratory distress, and malaise, which could be because of lactic acidosis.
Referral
Nutritionist
Rationale: Mrs. Wu explains that her weight has increased despite her efforts to exercise. Therefore, she needs the help of a dietician to develop a customized diet plan that will provide her with adequate calories, help with glycemic control, reduce body weight, and reduce hyperlipidemia (Powers et al., 2017).
Podiatrist
Rationale: Diabetic foot ulcers and amputations are common problems that contribute to the morbidity and mortality of patients with diabetes. Therefore, it is important to refer the patient to a podiatrist for specialized foot care (Thompson, 2018).
Eye specialist
Rationale: Since diabetes is associated with retinopathy, the patient should visit an eye specialist for regular eye checkups to prevent this occurrence (Powers et al., 2017).
Follow up
Mrs. Wu should return to the hospital after one month for a reassessment of her condition. The follow up will also evaluate the efficacy of the treatment options and the appropriateness of pharmacological interventions (ADA, 2018).
Medication Costs
The cost of 30 pills of extended-release metformin 500 mg is $13.58 at most pharmacies using the Drugs.com discount card. However, if the dose is increased to 2000 mg a day, a total of 120 tablets will be needed, which will bring the overall cost to $13.54 (Metformin prices, coupons and patient assistance programs, 2018). The price of the cheapest glucagon kit is about $144.58 (Glucagon prices, coupons and patient assistance programs, 2018). On the other hand, the cost of 30 pills of 10 mg atorvastatin in pharmacies using the Drugs.com discount card is $17.73 (Atorvastatin prices, coupons and patient assistance programs, 2018). The cost of diabetic supplies for one month will be 2 boxes of lancets (200 pieces) at the cheapest cost of $10, glucometer at $8.99, and test strips at $126 at a rate of 12 strips a day, each costing $0.35 (Glucose meter cost, 2018). The monthly supply of acetaminophen at the maximum dose of 4000 mg a day will be approximately $3.5 for a bottle containing 250 pills at Walmart (Acetaminophen, 2018). The monthly cost of multivitamin tablets would be $12.99 for 50 tablets of multivitamins (One a day women’s menopause formula multivitamin, 2018).
The total monthly cost for the drugs and medical supplies will be $337.33, which can be reduced further if the patient takes advantage of coupons offered on various drug websites. However, the glucometer will only need to be bought once. If Mrs. Wu buys a quality glucometer and takes good care of it, she should be able to use it for a long time. Therefore, the total cost of drugs for the subsequent months will exclude the cost of the glucometer and come down to $328.34. Furthermore, the glucagon kit is meant to be used only for emergencies. If the patient adheres to the treatment recommendations, it is possible to avoid extreme hypoglycemia thus eliminating the need to use the glucagon kit. Therefore, it is recommended that the patient buys a kit with the farthest possible expiration date to stretch its usability. In such a case, it is possible for the patient to afford her subsequent medications on a monthly budget of $192.75 or less. Depending on the patient’s insurance plan, some or all of these costs can be covered without the need to pay out of pocket.
The cost of diabetic care may prevent effective glycemic control for uninsured patients with low incomes. To prevent such occurrences, healthcare providers need to educate patients on cost-cutting strategies such as using coupons. However, in type 2 diabetes, effective glycemic control through healthy diets and regular exercise can lower the cost of diabetic care significantly.
Conclusion
Type 2 diabetes mellitus is a longstanding illness attributed to defects in insulin function. Poorly managed diabetes can result in various complications, including diabetic nephropathy, retinopathy, and neuropathy, which may cause kidney disease, eye problems, and diabetic foot ulcers. These complications contribute to morbidity and mortality in diabetes. Attaining optimal glycemic control is the goal of diabetes management, which is possible through a blend of pharmacological and nonpharmacological intermediations. Therefore, healthcare providers should empower patients through comprehensive patient education that covers all aspects of care.
Clinical Chart SOAP note
Patient Information: W, 59, female, Asian.
S: Chief Complaint
Increased fatigue, weight gain, polyuria, polydipsia, and polyphagia.
HPI: Mrs. W, a 59-year-old Asian female presents to the clinic with complaints of increased fatigue over the last 12 weeks. She exercises regularly but still gains weight. She experiences increased hunger and thirst, especially after exercise. She also experiences increased urination during the day as well as at night for the last 3 months. Mrs. W requires weight gain advice and evaluation for fatigue.
Current Medications: Tylenol 500 mg 2 tabs in AM knee pain.
Allergies: Bactrim, cats, and pollen.
PMHx: No chronic illness. German measles as a child. Right knee arthritis 3 months ago. All vaccines up to date.
PSHX: None.
Health screening: Colonoscopy WNL 4 years- repeat in 10 years, ASCUS pap 1998, all further Paps WNL, mammogram last year-benign
Soc Hx: Divorced, works from home as an administrative assistant, 1-2 glasses wine daily, former smoker, quit 10 years ago, no illicit drug use, exercises twice a week.
Fam Hx: Parents are deceased, child alive and well, no siblings.
ROS: General: female in no acute distress, alert, oriented and cooperative.
Musculoskeletal: Reports reduced pain.
O: Physical Exam
BP: 112/76; HR 80; RR 16; Hgt: 5’1.5″; Wgt: 165 lbs; BMI: 31.17
General: Female in no acute distress, alert, oriented and cooperative.
HEENT: head normocephalic. Hair thick and distribution throughout the scalp. Eyes without exudate, sclera white. Wears contacts. Tympanic membranes gray and intact with light reflex noted. Pinna and tragus nontender. Nares patent without exudate. Oropharynx moist without erythema. Teeth in good repair, no cavities noted. Neck supple. Anterior and posterior cervical lymph nontender to palpation. No lymphadenopathy. Thyroid midline, small and firm without palpable masses.
Skin: Warm dry and intact. No lesions.
CV: S1 and S2 RRR without murmurs or rubs.
Lungs: Clear to auscultation bilaterally, respirations unlabored.
Abdomen: soft, round, nontender with positive bowel sounds present; no organomegaly; no abdominal bruits. No CVAT.
Musculoskeletal: Full ROM both knees. Nontender to palpation bilaterally. Gait normal.
GU: bladder nontender upon palpation
Diagnostic or Lab results
CBC: WBC 6,300/mm3 Hgb 12.8 gm/dl Hct 42% RBC 4.6 million MCV 93 fl MCHC 34 g/dl RDW 13.8%
UA: pH 5, SpGr 1.010, Leukocyte esterase negative, nitrites negative, 1+ glucose; negative protein; negative ketones
CMP: Sodium 136, Potassium 4.4, Chloride 100, CO2 29, Glucose 130, BUN 12, Creatinine 0.7, GFR est non-AA 99 mL/min/1.73, GFR est AA 101 mL/min/1.73, Calcium 9.4, Total protein 7.6, Total Bilirubin 0.5, Alkaline phosphatase 72, AST 25, ALT 29, Anion gap 8.10, Bun/Creat 17.7, Hemoglobin A1C: 6.8 %
TSH: 2.31, Free T 4 0.9 ng/dL
Cholesterol: TC 215 mg/dl, LDL 144 mg/dl; VLDL 36 mg/dl; HDL 32mg/dl, Triglycerides 229
Primary Diagnosis: Type 2 diabetes mellitus (ICD-10 E11.9).
Secondary Diagnosis: Hyperlipidemia (ICD-10 E78.5)
Differential Diagnoses
Metabolic syndrome (ICD-10 E88.81).
Adjustment disorder with depressed mood (ICD-10 F43.21).
P: Diagnostics
- Spot urinary albumin-to-creatinine ratio
- HgbA1C
- Annual fasting CMP
- Foot exam
- Lipid profile
- Becks Depression Inventory
Medications
- Metformin 500 mg tablets (Extended-release)
Sig: Take 1 (one) tablet twice every day with food. Disp: #30. RF: 0
- Diabetic Lancets
Sig: Test blood glucose BID, more frequently as needed. Disp: 200 (2 boxes). RF: 2
- Glucometer
Sig: Test blood glucose BID, more frequently as needed. Disp: 1 kit. RF: 1
- Glucagon Emergency Kit
Sig: Inject 1mg IM as directed. Disp: 1 kit. RF: 2
- Test strips
Sig: Test blood glucose BID, more frequently as needed. Disp: 100 (1 box). RF: 2
- Multivitamin (over-the-counter)
Sig: Take 1 (one) tab daily
- Atorvastatin 10mg
Sig: Take 1 (one) tab daily. Disp: #30. RF: 0
- Acetaminophen 500 mg (over-the-counter)
Sig: Take 1 (one) tab every 4-6 hours when necessary for pain. Do not exceed 4000mg in 24 hrs.
Education
- Discussed diabetes self-care, including blood glucose monitoring and glucagon administration.
- Reviewed medications
- Recommended diet change and exercise
- Becks Depression Inventory: advised to call the hospital if signs of depression are experienced.
Referrals: Nutritionist, dietary advice
- Eye specialist, eye care
- Podiatrist, foot care
Follow up: Return to office in 1 month.
AACN MSN Essential IV: Translating and Integrating Scholarship into Practice
The paper about diabetes management helped me to meet the fourth MSN essential because I used existing evidence as a source of the proposed treatment plan. The analysis of subjective and objective information was supported by previous findings about diabetes, and my rationale for the diagnosis was informed by health care scholarship. For instance, I used test results to rule out differential diagnoses and discuss the patient’s current needs. I had to consider the literature about various tests to establish which of them were reliable. The urine test used in the assignment usually presents trustworthy results which can determine the development of diabetes. Moreover, I introduced GOLD standards for care, thus translating the developed guidelines into practice.
NONPF Core Competency 3: Quality
When evaluating the wellbeing of the patient, I relied on the most trustworthy and examined tests and measures to come to a diagnosis. Nonetheless, my assessment of the case was not limited to simply diagnosing the patient with diabetes and explaining my decision. I also provided the patient with a follow-up plan and suggested medications and lifestyle changes. Furthermore, I analyzed the costs of drug therapy for patients with diabetes, discussing the accessibility of treatments under the established system. The evaluation of the relationships between the cost of drugs and patient health is a prerequisite for quality improvement. I evaluated what could I, as an APN, achieve to make access to medication easier for patients with diabetes. The reflection on these subjects helped me to achieve competency in the field of quality care.
Concepts and Reflection
Health maintenance, the first considered concept, is the principle that is based on the belief that disease prevention is more effective and sustainable than its treatment (Steptoe, Deaton, & Stone, 2015). It opposes the ideas that conditions should be treated after they develop. In contrast, it emphasizes the importance of preventive practices that stop diseases from occurring in the first place. The main arguments for health maintenance are cost-effectiveness, lower levels of complications, and the elimination of risks connected to population health.
Self-care is a combination of different procedures and actions that people can perform to maintain their physical and mental health (Chen et al., 2014). Self-care can be a part of preventive and healing care, helping to avoid risks and alleviate symptoms of the disease. For example, self-care for patients diagnosed with diabetes is focused on blood glucose monitoring, foot care, and timely administration of medicine. Moreover, exercising and a healthy diet are elements of self-care for people with and without diabetes.
The assignment about diabetes management allowed me to perfect my skill of translating theoretical evidence into practice. I reflected on the state of drug therapy accessibility for patients who require medication for long periods of time. Diabetes is a condition that demands constant monitoring, and the diagnosis often changes the ways people with it have to live. Therefore, it is vital for nurses to focus on improving the quality of care for these patients to shift away from symptoms’ management to health maintenance. This change may positively affect the numbers of people diagnosed with diabetes as well as these people’s access to necessary treatments and diagnostic procedures. The field of self-care is also connected to quality competencies because it promotes a culture of autonomy and patient participation.
Exemplar # 9: NR 602 Care of the Childbearing and Childrearing Family
Clinical Case Presentation
Infectious diseases are dangerous since they spread freely and affect not only adults but also children. There are special ailments that are commonly referred to as pediatric illnesses because patients suffer from them, as a rule, at an early age. Their danger is that in case of serious complications, they can be fatal. In addition, a number of associated symptoms make the course of treatment more difficult and worsen patients’ well-being. In order to describe the typical features of the examination and assessment of patients, a special pediatric case will be considered. As an assessment tool, a standard analysis scheme will be utilized. Following all examinations, including diagnostic tests, growth and development parameters, and other valuable data, it is possible to receive the comprehensive picture of the health problem. The clinical analysis of the disease, which is performed through the assessment of various indicators of the body, makes it possible to eliminate differential diagnoses and determine a specific issue as accurately as possible.
Object of Outpatient Checkup and Primary Analysis
The object of the outpatient study is a 10-year-old white boy whom his parents have brought to their family doctor. The child has had a fever for two days and feels muscular weakness. The parents confirm the symptoms and note that the son has always been an active child. However, over the course of two days, he manifests apathy and fatigue and complains of cough and runny nose. Also, the parents are worried about the rash that appeared on the boy’s chest and stomach. According to the results of the initial examination, it has been decided to conduct a deep examination to test all the crucial indicators of the body.
Subjective Data Analysis
As an initial examination method, subjective data will be used. Based on conversations with the parents and the boy, valuable data may be obtained regarding the key symptoms of the proposed disease and related complications. The guideline presented by Davidson et al. (2017) describes the stages of complaint assessment and other important information that medical professionals need to take into account when providing family-centered care. As the main analysis tools, such factors will be considered as chief complaints (CC) and the history of present illness (HPI), and the information will be received from both the parents and the child.
Chief Complaints
Based on CC, the 10-year-old patient has consistently high body temperature, a runny nose, cough, and muscle weakness. Also, the parents note that their son has not slept well during the last two nights. As an additional concern, the boy shows a red rash on his chest, stomach, and parts of his neck. Over the past day, new foci of redness have been found on his hands. The child denies a sore throat and argues that the bright light makes him more sensitive. All these facts may be used to conduct further examinations. According to Griffey et al. (2015), the complexity of the assessment and interpretation of chief complaints is the lack of informational standardization, and specific data obtained directly from patients can be misunderstood. However, in this case, the boy’s symptoms are confirmed by his parents, and it is possible to exclude the wrong interpretation of sensations. Therefore, this information will become part of the further examinations and analysis of the patient’s body indicators.
History of Present Illness
The child notes that he felt the first symptoms of the disease three days ago when he returned from school. He argues that two of his classmates did not attend school at the moment, and they have the same symptoms as he did. The boy says that the rash of his friends today is more extensive than his. Also, the child’s mother and father confirm that they communicated with the parents of the sick children, and the course of their illness is identical. The patient assesses his current condition as worsening and notes that photophobia has been added to permanent headaches.
Objective Data Analysis
Based on the information obtained through the subjective analysis of data, the epidemiological nature of the child’s disease can be noted. Wendorf, Kay, Ortega-Sanchez, Munn, and Duchin (2015) remark that the “outbreaks of infectious diseases in ambulatory care” is a common phenomenon, and a tendency to increase in the number of patients may indicate a virus coverage growth. In order to make sure that the symptoms suggested by the child are correct, it is essential to perform the review of systems, conduct physical examinations, and identify diagnostic findings. Also, a growth chart will be compiled for height, weight, body mass index (BMI), and tanner staging.
Review of Systems
In accordance with the review of the eyes system, there are noticeable reddening of whites and the increased susceptibility of pupils to light, which may cause headaches. The ENT system (ears, nose, and throat) corresponds to the initial description of the patient, and the signs of inflammation are observed. Cardiovascular analysis shows increased fatigue and low stamina, which is noted by the child. Based on the review of the respiratory system, cough is observed. Constitutional symptoms indicate rash, as well as the loss of sleep and appetite.
Physical Examinations
The child shows lethargy and weak activity, indicating a breakdown. Based on the survey, the boy often plays sports, but due to the illness, he does not have the desire to perform any physical activity. Muscle tone is weak, and constant joint pain is confirmed. Due to high temperature and blood pressure, it is not possible to check the parameters of endurance on special equipment.
Diagnostic Findings
To obtain the most accurate clinical picture, an appropriate diagnosis should be made. According to the study by Hübschen et al. (2017), it is necessary to take swabs from the throat and nose, as well as blood and urine tests. Based on the results of the diagnostics, a specific virus can be identified, and an appropriate treatment plan may be prescribed. However, while the results of the tests are not obtained, it is impossible to draw unambiguous conclusions.
Growth Chart Percentiles
In order to obtain accurate and visually convenient information regarding patient growth data, a corresponding chart with necessary parameters will be compiled. Figure 1, Figure 2, Figure 3, and Figure 4 present the key indicators that need to be taken into account – height, weight, BMI, and tanner staging. All these data can be used as the valuable aspects of the child’s physical development, which is to be considered when making a diagnosis.
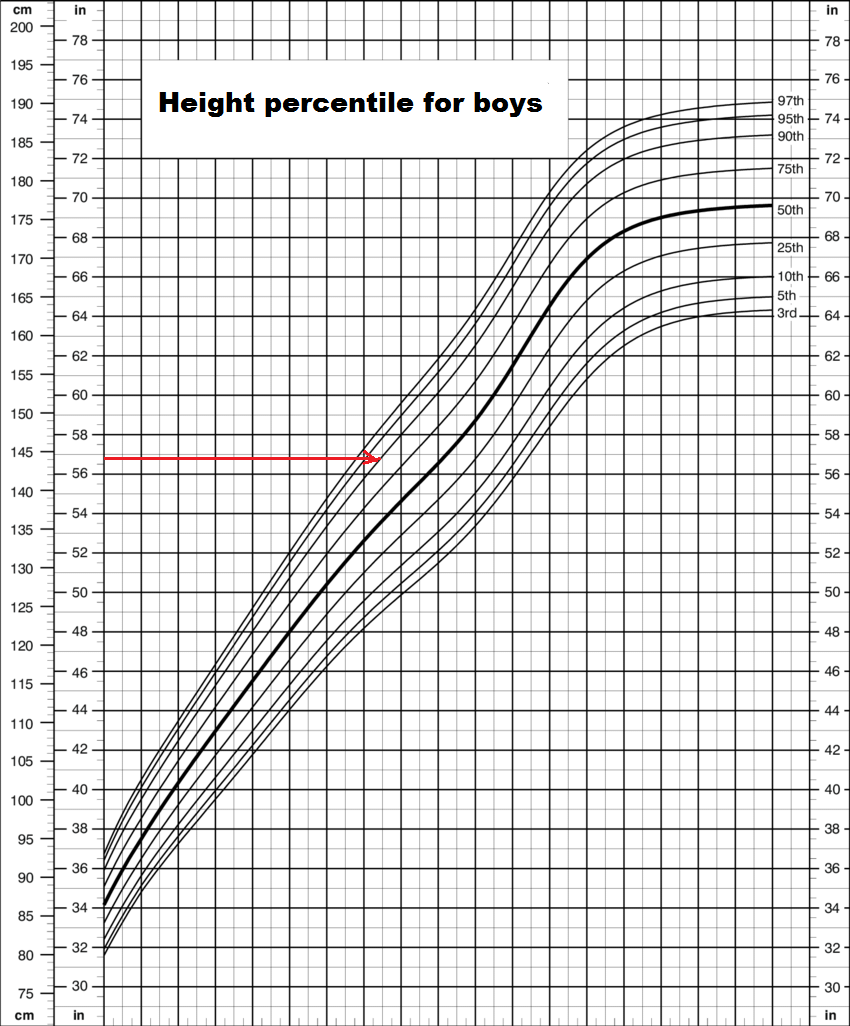
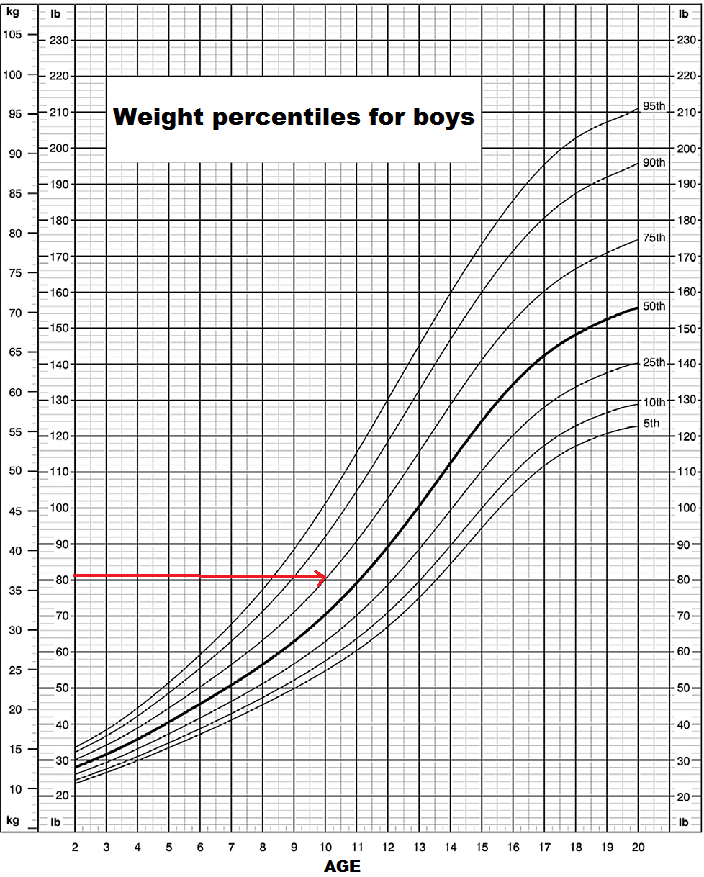
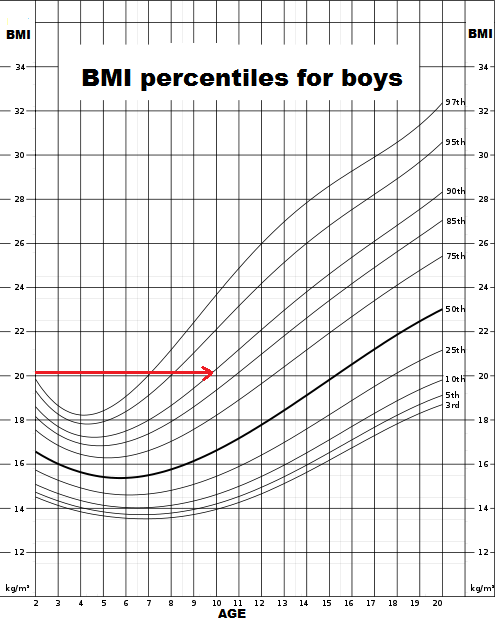
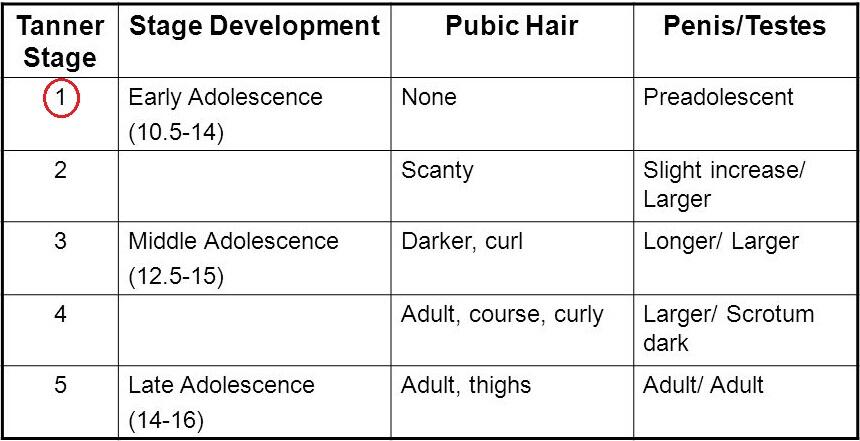
Conclusion
The comprehensive assessment of the patient’s condition by using current examination techniques allows identifying the main problems and eliminating differential diagnoses. The subjective and objective analysis of the information makes it possible to establish the true cause of the disease and identify the symptoms and complaints in detail. By utilizing the key checkup techniques, including the review of systems, physical examinations, and diagnostic findings, it is possible to determine the typical features of a particular illness.
AACN MSN Essential III: Quality Improvement and Safety
The third MSN essential requires nurses to apply quality principles in practice and use tools and methods that improve patient care. In this case, I used appropriate instruments to arrive at the diagnosis and determine the central issue. The patient’s situation was addressed using standard procedures that support safe and high-quality care and reduce any potential of incorrect diagnosis. As a result, my comprehensive assessment was defined by quality principles and key techniques that lead to successful and reliable conclusions. It is imperative to use methods that are approved by previous research and contribute to patients’ health in the most effective ways.
NONPF Core Competency 1: Scientific Foundation
The competency of scientific foundation implies that a practitioner will analyze evidence and data to improve their practice. Moreover, the implementation of data from previous research discussed above is also considered a part of this skill. Therefore, I believe that I achieved competency in the sphere of using previous research for practice and future projects, combining the knowledge of various sources for enhancing the state of health care provision. The use of previous methods in physical assessment helped me to build a foundation for diagnosing the patient. For instance, I utilized percentiles for height, weight, and BMI to establish the patient’s consistency with age-related development stages. I also relied on EBP data to determine which diagnostic tests would be appropriate for the patient. The combination of subjective and objective data analysis and diagnostics based on existing scholarship allowed me to provide comprehensive care to the patient.
Concepts and Reflection
The first concept is evidence-based practice (EBP) – a process where a practitioner uses data to create new and improve existing processes in health care (Melnyk, Gallagher‐Ford, Long, & Fineout‐Overholt, 2014). Nurses and other medical professionals need to use such information as results of clinical studies, quantitative and qualitative researches, and other types of healthcare-related knowledge in their practice. Here, the EBP information was used to determine the patient’s developmental progress.
The second concept is critical thinking – the ability to evaluate and analyze an issue and all related ideas to form judgments and make decisions (Kong, Qin, Zhou, Mou, & Gao, 2014). To engage in EPB meaningfully, nurses need to apply the skill of critical thinking when examining health care research and choosing the best available knowledge. Nurses have to consider the strengths and weaknesses of each finding or argument to improve the quality of care.
The investigation into the clinical case of a young patient improved my use of scientific evidence in practice and contributed to my commitment for safe and high-quality care. The case required me to consider the standards for children’s development and to review such aspects of assessment as health history, review of systems, and physical examination. My interpretation of diagnostic findings and other information was dependent on my experience and theoretical knowledge. Therefore, I applied critical thinking to connect the information from previous studies and approved standards and the case’s findings. All information that is derived from office visits such as the one described in the case can contribute to diagnosing, and its’ importance cannot be overstated. The completion of the assignment also supported my reflection of quality-improving practices and the focus on safe care for patients.
Exemplar # 10: NR 603 Advanced Clinical Diagnosis and Practice Across Life Span
Soap Note
Patient Information: M.G., 40-year-old female, race unknown, insurance unknown.
(S) Subjective
Chief Complaint (CC): “I think I may have a cold. I’ve been having a hard time breathing on and off lately.”
History of present Illness (HPI): This is a case of a 40 y/o female that presents to the clinic with shortness of breath occurring mostly while at work and subsides by the time she gets home. No episodes of shortness of breath on a weekend, but symptoms recur after a few hours at work. Patient claimed to have visited an urgent care clinic a few months back for shortness of breath which she was given a breathing treatment of some kind and was sent home with antibiotics. She denies having any productive cough, new allergy triggers, or heartburn. She is here today requesting antibiotics.
Current Medications
- Multivitamin
- Zyrtec
Allergies: Strawberries-Rash; erythromycin- severe GI upset.
PMHx: Michelle G. reports her overall health as good. Has seasonal allergies that is worse in spring. Managed by allergy specialist 10 years ago and received allergy shots for 5 years with great results, now only takes Zyrtec when needed.
Past Surgical History (PSurg Hx): Tonsillectomy, Cholecystectomy.
Childhood Illnesses: eczema as a child.
Immunization Hx: up-to-date on all vaccinations.
Hospitalizations: childbirth x 3.
Social History (Soc Hx): Married, lives with husband and 3 children. Worked in advertising up until 18 months ago when she got laid off. In order to help with the household finances, she took a job as a Baker’s assistant at an Artisan Bread Bakery. She arrives at 4 a.m. every morning to begin baking breads/pastries for the day. Drinks alcohol socially, smoked 1 pack per week for 3 years in her 20’s. Denies illicit drug use. Sleeps 6 to 7 hours a night. Exercises four to five days per week.
Family History (Fam Hx): Children are healthy- daughter currently has a sinus infection. Parents are deceased. Mother died at age 80 from congestive heart failure. Father died at age 82 from lung cancer, diagnosed when metastasized to brain. PGM: died from unknown causes, PGF: Stroke at age 82. MGM: died at 83, had HTN, atherosclerosis and many heart attacks. MGF: died at 71 from complications of COPD.
Review of Systems (ROS)
Constitutional: No reports of fever, chills, weight loss. Report sick contact-daughter has sinus infection.
HEENT: None reported.
Skin: None reported.
Cardiovascular: None reported.
Respiratory: Shortness of breath at work. Denies sputum.
Gastrointestinal: Denies heartburn.
Genitourinary : None reported.
Neurological: None reported.
Musculoskeletal: None reported.
Hematologic/lymphatic: None reported.
Psychiatric: None reported.
Endocrine: None reported.
Allergies: Erythromycin, strawberries and seasonal allergies. Eczema in childhood
(O) Objective
- Vital signs: B/P 130/70, T 98.0, HR 75, RR 18 Sao2 98% RA.
- Height: 5’10”, weight: 140 pounds, BMI: 20.1
Physical Exam
General: 40-year-old Caucasian female appears stated age in no apparent distress. Alert, oriented, and cooperative. Able to speak in full sentences and does not appear breathless.
HEENT: Head normo-cephalic. Hair thick and distribution even throughout scalp. Eyes: Sclera clear. Conjunctiva: white, PERRLA, EOMs intact. Ears: Tympanic membranes gray and intact with light reflex noted. Pinna and tragus non-tender. Nose: Nares patent with thin white exudate noted. Mucosa appears boggy and pale. Deviated septum noted. Sinuses non-tender to palpation. Throat: Oropharynx pink, moist, no lesions or exudate. Tonsils 1+ bilaterally. Teeth in good repair, no cavities noted. Tongue smooth, pink, no lesions, protrudes in midline. Neck supple. No cervical lymphadenopathy or tenderness noted. Thyroid midline, small and firm without palpable masses.
Lungs: Lungs clear to auscultation bilaterally. Respirations unlabored. Slight wheezing noted on inspiration and on forced expiration. Wheezing does not clear with forced cough.
Heart: Heart S1 and S2 noted, RRR, no murmurs noted, no displaced PMI. Peripheral pulses equal bilaterally, no peripheral edema.
Abdomen: Abdomen round, soft, and non-tender. Bowel sounds active in all four quadrants. No organomegaly noted.
Skin: Skin warm, dry, and intact. Skin color is pale pink, no cyanosis or pallor.
Diagnostic results
CXR Report: normal CXR 11/7/2016.
This is a PA and lateral chest radiograph on Ms. Michelle X, performed on 11/7/16. Clinical information: low grade fever, productive cough, malaise.
Findings: Cardio-mediastinal silhouette is normal. B/L lung fields are clear. There are no effusions. The bony thorax appears normal. No opacities or fluid. Diaphragm normal.
Impression: Normal chest radiograph without pathology.
Pulmonary Function Testing:
Pre-Bronchodilator Challenge- FEV1/FVC 60%, FVC decreased.
Post Bronchodilator Challenge- FEV1/FVC 75%.
Seasonal allergies, spring is her worst season. Was seen by an allergy specialist ten years ago.
(A) Assessment
Primary Diagnosis: Occupational asthma (J45.909)
I diagnosed Michelle with Occupational asthma. Her severity of symptoms falls under the classification of mild persistent. My diagnosis of occupational asthma is partially based on Michelle’s exacerbation of symptoms when she is at work. Physiologically, asthma is characterized by bronchial hyperresponsiveness, the tendency of airways to narrow excessively in response to a variety of stimuli that provoke little or no bronchoconstriction in persons without airway disease (Global Initiative for Asthma, 2018). Underlying airway inflammation (which involves cellular infiltration, edema, nerve irritation, and vasodilation) results in constriction of airway smooth muscle, increased production of mucus, and airway hyperresponsiveness. (Buttaro,Trybulski,Polgar-Bailiey & Sandburg-Cook, 2017).
The airflow limitation associated with asthma is caused by a variety of changes in the airway, all of which are influenced by airway inflammation. The “classic” signs and symptoms of asthma are intermittent dyspnea, cough, and wheezing (Fanta, 2017). Another part of her subjective data that help me establish my diagnosis is the fact that Michelle’s symptoms did not start until she started her job at the bakery. Michelle’s PTF results (pre-bronchodilator FEV1/FVC 60%, FVC, and post-bronchodilator challenge FEV1/FVC 75%) were also key for an asthma diagnosis. An FEV/FVC ratio less than 70% is indicated of an obstructive defect, and an increase in FEV or FVC after bronchodilator of more than 12% is an indication of a reversible disease (Johnson, & Theurer, 2014). Asthma is an obstructive and reversible pulmonary disease.
The patient’s flare-ups are affecting her activity level, for example: she noted shortness of breath at work, but not at home. The asthma symptoms are most likely trigger by the flour that she is on contact with at her new job since she was not having these issues at her previous job.
Secondary Diagnosis: Allergic Rhinitis (ICD 10 J30.9)
My diagnosis of allergic rhinitis is based on Michelle’s history of seasonal allergies, the presence of thin white discharge, and the pale and boggy mucosa on Michelle’s physical examination. Pale and boggy mucosa is due to swelling of the mucosa that occludes the passage and extends the inflammation, characteristics of allergic rhinitis (Srivastava et al., 2016).
Zhong, Lai, Zheng, and Li (2018) defined Allergic rhinitis (AR) as chronic inflammation of the nasal mucous membrane, typically induced by immunoglobulin E- (Ig E-) mediated sensitization to environmental allergens. The nose contains a large surface area where inhaled particles are trapped before they can flow into the lower respiratory structures. Most allergens are large and become trapped in the mucous membranes of the nasal tissue. In the mucous membranes, there is an initial reaction between the allergen and intraepithelial mast cells, which proceeds deeper to the perivenular mast cells, both of which are sensitized with specific IgE (Buttaro,Trybulski,Polgar-Bailiey & Sandburg-Cook, 2017). AR is diagnosed when two or more of the following sign and symptoms are present for at least 1 hour/day and persist for at least 2 weeks: sneezing, rhinorrhea/runny nose, nasal blockage/congestion and itching of the nasal and sinus area (Zhong et al., 2018).
(P) Plan
Albuterol (ProAir HFA) 90 mcg per actuation
Rx: Abuterol MDI: 90 mcg/puff, 200 puffs/canister.
Sig: 2 puffs 5 minutes before exercise, 2 puffs every 4-6 hours as needed for symptoms.
Dispense: #1, Refills: 1.
This is the first-line treatment for a patient with mild persistent asthma. It is a short-acting beta-agonist (SABA) and is considered a rescue inhaler and highly effective for quick relief of asthma symptoms such as shortness of breath, chest tightness, and wheezing by relaxing the smooth muscle within the airway walls. SABAs are the best option for acute bronchospasms and exacerbations associated with asthma because it relaxes bronchial smooth muscle by action on beta2 receptors (Ortega & Pennington, 2017).
Fluticasone (Flovent HFA) 110 mcg/actuation
Rx: Fluticasone.
Sig: 2 puffs inhaled twice a day, rinse mouth after each use.
Dispense: #1, Refills: 0.
Inhaled corticosteroids (ICS) are proven the most effective in long term management and control of asthma. Ortega and Pennington (2017) stated that ICS is indicated for long-term suppression, control, and reversal of inflammation and symptoms thus improve asthma outcomes such as lung function, symptoms, and exacerbation.
Montelukast 10 mg tablet
Rx: Montelukast 10 mg tab.
Sig: take one tablet daily at bedtime.
Dispense: #30 tabs, Refills: 0.
Montelukas sodium is a selective and active leukotriene receptor antagonist which prevents airway edema, smooth muscle contraction and other respiratory inflammation. The leukotrienes are also released from the nasal mucosa after allergen exposure where montelukast sodium may inhibit symptoms of allergic rhinitis. It is used to treat asthma and allergic rhinitis. Patients with asthma should take dose in the evening (Haarman, Hunsel, & Vries, 2017).
Continue: Multivitamin.
Discontinue
Zyrtec.
Non- Pharmacologic Management
Peak flow meter
Use three times a day once in the morning, once in the afternoon and once in the evening. Use for two weeks three times a day.
Education
Creating an Asthma action plan tailored for Michelle and it is imperative to adherence. Teaching them the correct techniques for inhaler use and the reason for its use, side effects, seeking medical care as necessary, recognizing the signs and symptoms of asthma attacks/episodes and to distinguish and avoid environmental factors and irritants (Espinoza, Espinoza, Wilson, & Delton, 2018). Encouraged Michelle to rinse her mouth right after using the inhaler to avoid developing oral fungal infection. Avoiding exposure to allergens/triggers has significantly influenced allergic nasal improvements. Instruct Michelle on how to track triggers with a log to find out exactly when they are happening such as time, date, symptoms and how the symptoms were relieved, or prevent exacerbations. Minimize the need for the emergency room. Self-monitoring by using peak flow meter twice a day until reevaluation in 2 weeks.
Use of peak flow meter:
- Stand up or sit up straight.
- Make sure the indicator is at the bottom of the meter (zero).
- Take a deep breath in, filling the lungs completely.
- Place the mouthpiece in your mouth lightly bite with your teeth and close your lips on it. Be sure your tongue is away from the mouthpiece.
- Blast the air out as hard and as fast as possible in a single blow.
- Remove the meter from your mouth
- Record the number that appears on the meter and then repeat steps one through seven two more times.
- Record the highest of the three readings in an asthma diary This reading is your peak expiratory flow (PEF).
To ensure the results of the peak flow meter, be sure to use the meter the same way each time you take a reading. Peak flow values are best if they are checked at the same time each day, preferably once in the morning and again at night. The “personal best” peak expiratory flow (PEF) is the highest peak flow number you can achieve over a two to three-week period when asthma is under good control. Good control means feeling good and do not have any asthma symptoms. Yearly flu shot is very important (Asthma and Allergy Foundation of American, 2015). Lastly, instruct Michelle to return to the clinic or nearest ED if shortness of breath, wheezing, cough, or chest tightness worsens.
Asthma/Allergy: Reduce exposure to allergens, dust mites or pet dander, frequently wash beddings in hot water. Reduce moisture in damp areas while maintaining low humidity. Use HEPA filter during vacuuming, replace carpets with wood floorings, identify triggers to allergic symptoms, recommend wearing a medic alert bracelet. Encourage Michelle to wear a mask to lessen exposure and to carry the rescue inhaler for immediate needs.
Referrals/Consults: No referral to asthma specialist or pulmonologist at this time. Will consider under these conditions: asthma is difficult-to-control, medication side effects are intolerable, or when a patient has frequent exacerbations (Fanta, 2017).
Follow-up Plan: Return in 2 weeks to assess for symptom improvement and to determine whether to step up or step-down treatment. Mccracken et al., (2017) mentioned that asthma follow up visit should be done as follows: follow up every 2-6 weeks while obtaining control, every 1-6 months to monitor control and every 3 months when step-down therapy is possible. Bring in medications, peak flow meter and peak flow journal with you to follow up at follow up we will also reevaluate of medications for determination of control or uncontrolled symptoms, we will go over proper medication technique by demonstration by staff member and Michelle will repeat demonstration of proper medication technique and understanding. Review adherence to medication and any side effects of mediations. Will review any new environmental triggers.
PO #5: Advocates for positive health outcomes through compassionate, evidence-based, collaborative advanced nursing practice (Extraordinary Nursing)
The study of occupational asthma required me to use my experience, education, communicative skills, and critical thinking to create a comprehensive plan for the patient. I used EBP knowledge to arrive at a diagnosis and develop a treatment strategy. I also considered the patient’s specific needs and characteristics in order to ensure that my advice is appropriate for her socioeconomic and cultural background. My examination and suggestions were aimed at providing the patient with the best possible care and contributing to her long-term wellbeing. As a result, the created treatment plan allowed me to reach the program outcome of Extraordinary Nursing and further improved the multitude of abilities that APNs must possess.
NONPF Core Competency 9: Independent Practice
During the assignment’s completion, I acted as a licensed independent practitioner and applied my knowledge in such disciplines as physiology, pathophysiology, and pharmacology. First of all, I analyzed the patient’s complaints and determined the methods to diagnose her problem. I chose screening tools and performed assessments necessary to understand the state of the patient’s health. Next, I created a plan that included appropriate medications and lifestyle changes. When selecting measures for self-care and treatment, I acknowledged various legal and ethical issues that could arise for the patient and myself. Furthermore, I engaged in patient education and created a trusting relationship with the patient to deliver information and ensure that my client adheres to the suggestions. All activities performed as a part of this assignment contributed to my ability to practice independently.
Concepts and Reflection
Accountability is one of the pillars in independent nursing practice. Nurses need to take responsibility for their choices and decisions and demonstrate their competence in practice. Thus, accountability for one’s actions and the safety of patients is vital to health care. Nurses have to ensure that they are able to perform all duties mentioned in their state’s official standards. Otherwise, they will be unable to take responsibility for their performance.
Clinical decision making is the activity in which nurses partake every day. It is based on previous findings and patient’s needs, and nurses must understand the implications of their choices as well as the arguments for their conclusions. Moreover, clinical decision making requires one to integrate the previous research findings and trustworthy evidence in order to avoid negative consequences. It is expected of nurses to rely on the principles of critical and ethical thinking.
The patient’s case tested my abilities as a practitioner and improved my confidence in treating patients. It required my full commitment to nursing practice, exercising my theoretical knowledge, clinical experience, and patient-nurse communicative skills. I was able to judge my strengths and weaknesses as a future independent practitioner and to review my responsibilities in practice. The ability to apply different types of scientific information was helpful to my understanding of nursing competencies and strive for continuous improvement. I utilized existing guidelines for asthma diagnosis, considered the patient’s past health to correct the treatment plan, and exercised my leadership skills to set goals for the patient to achieve. The integration of different actions in this project enhanced my professional skill set and prepared me for the future.
Conclusion
The examination of the selected exemplars suggests that all competencies and objectives set by the program were achieved as a result of completing the course. Each assignment did not focus on one competency, requiring a multifaceted approach instead. I presented a description of the skills that were the central part of each project. As a result, one can see that all five Program Outcomes, nine MSN Essentials, and nine NONPF Competencies were covered during the learning process. The different aspects of the assignments allowed me to focus on different areas of the nursing profession. Some of them were more theory-driven, helping me to perfect my understanding of research project development and completion. Others involved practical exercises that tested my ability to apply scholarly knowledge in a real setting. Overall, the exemplars reflect the broad scope of activities in which I participated.
The completion of these assignments as well as the final reflection paper influenced my personal understanding of the nursing practice. I saw how complex and intricate nursing decision-making can be, and which of the aspects of the current health care system require improvement. Moreover, I was able to address my insecurities and weaknesses, especially my fear of being unqualified to assume additional responsibilities as a nurse. Through practice and research, I overcame this anxiety and prepared myself for future duties as an APN. This self-reflection revealed the scope of knowledge that I gathered and the number of activities that I already performed in a practice setting. These facts contributed to my confidence as a professional and assured me in my potential for self-improvement and contribution to the health of others and the field of health care.
References
Bernhardt, J. (2017). Early mobilisation and rehabilitation in the intensive care unit–Ready for implementation? Annals of Translational Medicine, 5(3), 57-59.
Chen, H. T. (2014). Practical program evaluation. Thousand Oaks, CA: Sage.
Clark, D. E., Lowman, J. D., Griffin, R. L., Matthews, H. M., & Reiff, D. A. (2013). Effectiveness of an early mobilization protocol in a trauma and burns the intensive care unit: A retrospective cohort study. Physical Therapy, 93(2), 186-196.
Engel, H. J., Needham, D. M., Morris, P. E., & Gropper, M. A. (2013). ICU early mobilization: From recommendation to implementation at three medical centers. Critical Care Medicine, 41(9), S69-S80.
Leditschke, I. A., Green, M., Irvine, J., Bissett, B., & Mitchell, I. A. (2012). What are the barriers to mobilizing intensive care patients? Cardiopulmonary Physical Therapy Journal, 23(1), 26-29.
Lord, R. K., Mayhew, C. R., Korupolu, R., Mantheiy, E. C., Friedman, M. A., Palmer, J. B., & Needham, D. M. (2013). ICU early physical rehabilitation programs: Financial modeling of cost savings. Critical Care Medicine, 41(3), 717-724.
Patel, B. K., Pohlman, A. S., Hall, J. B., & Kress, J. P. (2014). Impact of early mobilization on glycemic control and ICU-acquired weakness in critically ill patients who are mechanically ventilated. CHEST Journal, 146(3), 583-589.
Reade, M. C., & Finfer, S. (2014). Sedation and delirium in the intensive care unit. New England Journal of Medicine, 370(5), 444-454.
Schaller, S. J., Anstey, M., Blobner, M., Edrich, T., Grabitz, S. D., Gradwohl-Matis, I.,… Lee, J. (2016). Early, goal-directed mobilisation in the surgical the intensive care unit: A randomised controlled trial. The Lancet, 388(10052), 1377-1388.
Sricharoenchai, T., Parker, A. M., Zanni, J. M., Nelliot, A., Dinglas, V. D., & Needham, D. M. (2014). Safety of physical therapy interventions in critically ill patients: A single-center prospective evaluation of 1110 intensive care unit admissions. Journal of Critical Care, 29(3), 395-400.
Allison, V. L., Nativio, D. G., Mitchell, A. M., Ren, D., & Yuhasz, J. (2014). Identifying symptoms of depression and anxiety in students in the school setting. The Journal of School Nursing, 30(3), 165-172.
Cunningham, J. M., & Suldo, S. M. (2014). Accuracy of teachers in identifying elementary school students who report at-risk levels of anxiety and depression. School Mental Health, 6(4), 237-250.
Prochaska, J. D., Le, V. D., Baillargeon, J., & Temple, J. R. (2016). Utilization of professional mental health services related to population-level screening for anxiety, depression, and post-traumatic stress disorder among public high school students. Community Mental Health Journal, 52(6), 691-700.
Aldrich, M. C., Munro, M. M., Mumma, M., Grogan, E. L., Massion, P. P., Blackwell, T. S., & Blot, W. J. (2015). Chronic obstructive pulmonary disease and subsequent overall and lung cancer mortality in low-income adults. PLoS ONE, 10(3), 1-14. Web.
Doney, B., Hnizdo, E., Syamlal, G., Kullman, G., Burchfiel, C., Martin, C. J., & Mujuru, P. (2014). Prevalence of chronic obstructive pulmonary disease among us working adults aged 40 to 70 years. J Occup Environ Med, 56(10), 1088–1093. Web.
Holt, J. B., Huston, S. L., Heidari, K., Schwartz, R., Gollmar C. W., Tran, A., Croft, J. B. (2015). Indicators for chronic disease surveillance – United States, 2013. Morbidity and Mortality Weekly Report (MMWR), 64(1), 1 – 250. Web.
Reid P. T., & Innes, J. A. (2014). Obstructive pulmonary disease. In R. N. Colledge et al. (Eds.), Davidson’s principles and practice of medicine (22nd ed.) (pp. 662 -678). Edinburg, UK: Elsevier Limited.
Srivastava, K., Thakur, D., Sharma, S., & Punekar, Y. S. (2015). Systematic review of humanistic and economic burden of symptomatic chronic obstructive pulmonary disease. PharmacoEconomics, 33(1), 467–488. Web.
AANP Job Center. (2018). Recent jobs. Web.
Barnes, H. (2015). Exploring the factors that influence nurse practitioner role transition. The Journal for Nurse Practitioners, 11(2), 178-183.
DeNisco, S., & Barker, A. M. (Eds.). (2015). Advanced practice nursing: Essential knowledge for the profession (3rd ed.). Burlington, MA: Jones & Bartlett Learning.
Florida Board of Nursing. (2018). Advanced registered nurse practitioner (ARNP). Web.
Lima, S., Newall, F., Kinney, S., Jordan, H. L., & Hamilton, B. (2014). How competent are they? Graduate nurse self-assessment of competence at the start of their careers. Collegian, 21(4), 353-358.
Sastre‐Fullana, P., Pedro‐Gómez, D., Bennasar‐Veny, M., Serrano‐Gallardo, P., & Morales‐Asencio, J. M. (2014). Competency frameworks for advanced practice nursing: A literature review. International Nursing Review, 61(4), 534-542.
Cystic Fibrosis Foundation (2018). Web.
Katkin, J. (2017). Cystic fibrosis: Clinical manifestations and diagnosis. UpToDate. Web.
Lawton, M. R., & Schub, T. B. (2015). Cystic Fibrosis: Newborn Screening. CINAHL Nursing Guide. Web.
McCance, K. L., Huether, S. E., Brashers, V. L., & Rote, N. S. (2014). Pathophysiology: The biologic basis for disease in adults and children (7th ed.). St. Louis, MO: Mosby.
Van Biervliet, S., De Clercq, C., Declercq, D., Van Braeckel, E., Van Daele, S., De Baets, F., & De Looze, D. (2016). Gastro-intestinal manifestations in cystic fibrosis patients. Acta Gastro-Enterological Belgica, 79(4), 481-486.
Birgisson, N. E., Zhao, Q., Secura, G. M., Madden, T., & Peipert, J. F. (2015). Preventing unintended pregnancy: The contraceptive CHOICE project in review. Journal of Women’s Health, 24(5), 349-353.
Curtis, K. M., & Peipert, J. F. (2017). Long-acting reversible contraception. The New England Journal of Medicine, 376(5), 461-468.
Gavin, L., Moskosky, S., Carter, M., Curtis, K., Glass, E., Godfrey, E., … Zapata, L. (2015). Providing quality family planning services: Recommendations of CDC and the U.S. office of population affairs. Centers for Disease Control and Prevention: Recommendations and Reports, 63(4), 1-54. Web.
Boore, J., Cook, N., & Shepherd, A. (2016). Essentials of anatomy and physiology for nursing practice. Thousand Oaks, CA: SAGE.
Kon, C., & Rai, M. (2016). The microbiology of respiratory system infections. New York, NY: Academic Press.
Sharafkhaneh, A., Yohannes, A. M., Hanania, N. A., & Kunik, M. E. (2017). Depression and anxiety in patients with chronic respiratory diseases. New York, NY: Springer.
Ward, J. P. T., Ward, J., & Leach, R. M. (2015). The respiratory system at a glance (4th ed.). New York, NY: John Wiley & Sons.
Acetaminophen. (2018). Web.
Acuna, M. J. V., Labinson, P., & McDermott, J. (2017). Left lower arm hemichorea: An unusual presentation of new-onset type 2 diabetes. Clinical Diabetes, 35(3), 183-184.
Albert, P. R. (2015). Why is depression more prevalent in women? Journal of Psychiatry & Neuroscience: JPN, 40(4), 219-221.
American Diabetes Association. (2018). Standards of medical care in diabetes—2018. Diabetes Care, 41(suppl. 1), S13-S125. Web.
Armstrong, D. G., Boulton, A. J., & Bus, S. A. (2017). Diabetic foot ulcers and their recurrence. New England Journal of Medicine, 376(24), 2367-2375.
Aroda, V. R., Edelstein, S. L., Goldberg, R. B., Knowler, W. C., Marcovina, S. M., Orchard, T. J.,… Crandall, J. P. (2016). Long-term metformin use and vitamin B12 deficiency in the diabetes prevention program outcomes study. The Journal of Clinical Endocrinology & Metabolism, 101(4), 1754-1761.
Arthritis Foundation. (2018). Osteoarthritis treatment. Web.
Atorvastatin prices, coupons and patient assistance programs. (2018). Web.
Chatterjee, S., Khunti, K., & Davies, M. J. (2017). Type 2 diabetes. The Lancet, 389(10085), 2239-2251.
Fayfman, M., Pasquel, F. J., & Umpierrez, G. E. (2017). Management of hyperglycemic crises: Diabetic ketoacidosis and hyperglycemic hyperosmolar state. Medical Clinics, 101(3), 587-606.
Furukawa, S., Fujita, T., Shimabukuro, M., Iwaki, M., Yamada, Y., Nakajima, Y.,… Shimomura, I. (2017). Increased oxidative stress in obesity and its impact on metabolic syndrome. The Journal of Clinical Investigation, 114(12), 1752-1761.
Glucagon prices, coupons and patient assistance programs. (2018). Web.
Glucose meter cost. (2018). Web.
Kheradpezhouh, E., Ma, L., Morphett, A., Barritt, G. J., & Rychkov, G. Y. (2014). TRPM2 channels mediate acetaminophen-induced liver damage. Proceedings of the National Academy of Sciences, 111(8), 3176-3181.
McCreight, L. J., Bailey, C. J., & Pearson, E. R. (2016). Metformin and the gastrointestinal tract. Diabetologia, 59(3), 426-435.
Metformin prices, coupons and patient assistance programs. (2018). Web.
Navar-Boggan, A. M., Peterson, E. D., D’Agostino Sr, R. B., Neely, B., Sniderman, A. D., & Pencina, M. J. (2015). Hyperlipidemia in early adulthood increases long-term risk of coronary heart disease. Circulation, 131(5), 451-458.
Niafar, M., Hai, F., Porhomayon, J., & Nader, N. D. (2015). The role of metformin on vitamin B12 deficiency: A meta-analysis review. Internal and Emergency Medicine, 10(1), 93-102.
O’Donnell, M. L., Alkemade, N., Creamer, M., McFarlane, A. C., Silove, D., Bryant, R. A.,… Forbes, D. (2016). A longitudinal study of adjustment disorder after trauma exposure. American Journal of Psychiatry, 173(12), 1231-1238.
One a day women’s menopause formula multivitamin. (2018). Web.
Powers, M. A., Bardsley, J., Cypress, M., Duker, P., Funnell, M. M., Fischl, A. H.,… Vivian, E. (2017). Diabetes self-management education and support in type 2 diabetes: A joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. The Diabetes Educator, 43(1), 40-53.
Rafieian-Kopaei, M., Setorki, M., Doudi, M., Baradaran, A., & Nasri, H. (2014). Atherosclerosis: Process, indicators, risk factors and new hopes. International Journal of Preventive Medicine, 5(8), 927-946.
Ramkumar, S., Raghunath, A., & Raghunath, S. (2016). Statin therapy: Review of safety and potential side effects. Acta Cardiologica Sinica, 32(6), 631-639.
Semenkovich, K., Brown, M. E., Svrakic, D. M., & Lustman, P. J. (2015). Depression in type 2 diabetes mellitus: Prevalence, impact, and treatment. Drugs, 75(6), 577-587.
Thompson, A. T. (2018). Red flags for potential diabetes-related foot disease: When you should refer to a podiatrist. South African Journal of Diabetes, 11(3), 23-25.
United States Preventive Service Task Force (USPSTF). (2016). Breast cancer: Screening. Web.
Davidson, J. E., Aslakson, R. A., Long, A. C., Puntillo, K. A., Kross, E. K., Hart, J.,… Curtis, J. R. (2017). Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Critical Care Medicine, 45(1), 103-128. Web.
Griffey, R. T., Pines, J. M., Farley, H. L., Phelan, M. P., Beach, C., Schuur, J. D., & Venkatesh, A. K. (2015). Chief complaint-based performance measures: A new focus for acute care quality measurement. Annals of Emergency Medicine, 65(4), 387-395. Web.
Hübschen, J. M., Bork, S. M., Brown, K. E., Mankertz, A., Santibanez, S., Mamou, M. B.,… Muller, C. P. (2017). Challenges of measles and rubella laboratory diagnostic in the era of elimination. Clinical Microbiology and Infection, 23(8), 511-515. Web.
Wendorf, K. A., Kay, M., Ortega-Sanchez, I. R., Munn, M., & Duchin, J. (2015). Cost of measles containment in an ambulatory pediatric clinic. The Pediatric Infectious Disease Journal, 34(6), 589-593. Web.
Asthma and Allergy Foundation of American. (2015). Flu (Influenza). Web.
Buttaro, T., Trybulski, J., Polgar-Bailey, P., & Sandburg-Cook, J. (2017). Primary care: A collaborative practice (5th ed.). Web.
Espinoza, L. E., Espinoza, L. E., Wilson, M. L., & Denton, T. E. (2018). Asthma predictors influence on self-management asthma education status. American Journal of Health Behavior, 42(5), 74-84. Web.
Fanta, C. H. (2017). Diagnosis of asthma in adolescents and adults. In H. Hollingsworth (Ed.), UpToDate. Web.
Global Initiative for Asthma (GINA). (2018). Global strategy for asthma management and prevention. Web.
Haarman, M. G., Hunsel, F., & Vries, T. W. (2017). Adverse drug reactions of montelukast in children and adults. Pharmacology Research and Perspectives, 5(5), n/a-N.PAG. Web.
Johnson, J. D., & Theuder, W. M. (2014). A stepwise approach to the interpretation of pulmonary function tests. American Family Physician, 89(5), 359-366. Web.
McCracken, J. L., Veeranki, S. P., Ameredes, B. T. & Calhoun, W. J. (2017). Diagnosis and Management of asthma in adults: A review. JAMA: Journal of the American Medical Association, 318(3), 279. Web.
Ortega, V. E., & Pennington, E. J. (2017). Drug treatment of asthma. Merck Manuals Profession Version. Web.
Srivastava, M., Bhadouriya, S. S., Saxena, R., Singh, V., Srivastava, A., & Bisht, M. (2016). Comparative clinical evaluation of effect of topical verses systemic anti -allergic drug in allergic rhinitis: A prospective study. Online Journal of Otolaryngology, 6(1), 35-46.
Zhong, J., Lai, D., Zheng, Y., & Li, G. (2018). Ma-Huang-Fu-Zi-Xi-Xin decoction for Allergic rhinitis: A systematic review. Evidence-Based Complementary & Alternative Medicine (ECAM), 1-6. Web.
Chen, A. M., Yehle, K. S., Albert, N. M., Ferraro, K. F., Mason, H. L., Murawski, M. M., & Plake, K. S. (2014). Relationships between health literacy and heart failure knowledge, self-efficacy, and self-care adherence. Research in Social and Administrative Pharmacy, 10(2), 378-386.
de Leeuw, E. (2017). Engagement of sectors other than health in integrated health governance, policy, and action. Annual Review of Public Health, 38, 329-349.
De Nicola, L., & Zoccali, C. (2015). Chronic kidney disease prevalence in the general population: Heterogeneity and concerns. Nephrology Dialysis Transplantation, 31(3), 331-335.
Hagan, T. L., Schmidt, K., Ackison, G. R., Murphy, M., & Jones, J. R. (2017). Not the last word: Dissemination strategies for patient-centred research in nursing. Journal of Research in Nursing, 22(5), 388-402.
Kong, L. N., Qin, B., Zhou, Y. Q., Mou, S. Y., & Gao, H. M. (2014). The effectiveness of problem-based learning on development of nursing students’ critical thinking: A systematic review and meta-analysis. International Journal Of Nursing Studies, 51(3), 458-469.
Melnyk, B. M., Gallagher‐Ford, L., Long, L. E., & Fineout‐Overholt, E. (2014). The establishment of evidence‐based practice competencies for practicing registered nurses and advanced practice nurses in real‐world clinical settings: Proficiencies to improve healthcare quality, reliability, patient outcomes, and costs. Worldviews on Evidence‐Based Nursing, 11(1), 5-15.
National Organization of Nurse Practitioner Faculties [NONPF] (2017). Nurse practitioner core competencies content. Web.
Steptoe, A., Deaton, A., & Stone, A. A. (2015). Subjective wellbeing, health, and ageing. The Lancet, 385(9968), 640-648.
Appendix A: Concept Map