Nursing profession is among the leading human health sciences with significant theory- practice gaps. While the learners are well equipped with both knowledge and skills during different levels of training, which is in clinical and practical, there still remains a huge mismatch in their actual practice in the health institutions. This has contributed to the theory practice gap, which is the difference between what is taught during training and the expectations in the clinical set-up during practice. Theoretical-practice gaps cause a high risk to patients, especially those that are critically ill due to mismanagement (Arends & Callies, 2022). Therefore, this paper analyzes the theoretical-practice gaps in the nursing profession.
In the case study presented, the critical nurse who supposedly has more experience in working with critically ill patients continues to take care of an elderly patient after an operation. Well, postoperative patients, especially those under mechanical ventilation require maximum care while in the intensive care unit. This may involve closely monitoring oxygen saturations and other patient’s vitals. In this case, the seventy five year old postoperative patient also has an underlying condition, obstructive pulmonary disease, which increases the oxygen requirements. While breathing difficulty is one of the main challenges with such patients, regular sanctioning reduces the amount of secretions, thus reducing the chances of respiratory distress.
The main theoretical-practice gap identified from the case is the use of distilled water while sectioning the patient. The nurse instilled distilled water into the endotracheal tube during sectioning. While the use of normal saline before sanctioning is a common clinical practice for intubated patients or those with tracheostomy tubes, evidence shows that there are more disadvantages associated with it. During clinical training, this is an area that is commonly taught in many institutions. However, the use of normal saline only reduces patients’ oxygen saturations after sanctioning (Arends & Callies, 2022). Therefore, whether the secretions are thick or not, distilled water should not be instilled to the endotracheal tube, especially at the time of sanctioning as it can lead to dyspnea, hence respiratory distress.
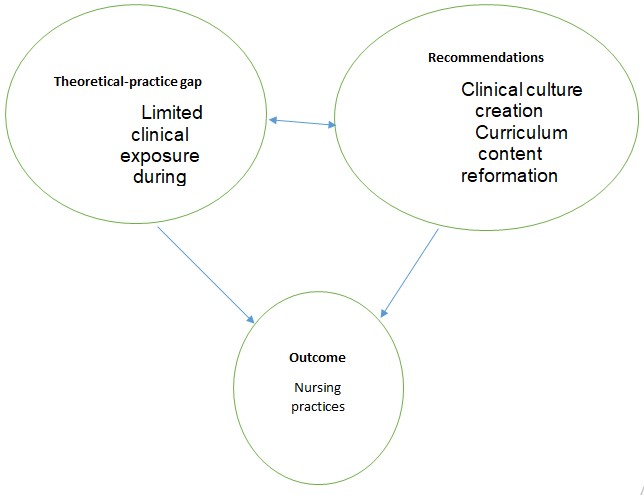
To close this theoretical-practice gap, several approaches are reliable. First, the curriculum content reformation, which include changing certain aspects taught in class and replacing with evidence based findings is of great significance. The conventional practices in nursing are now changing due to more research and advances in technology. Another approach to bridge the identified theoretical practice gap is by creating a clinical culture. The learners should be allowed to regularly practice in clinical set-ups often (Haghighat et al, 2020). Although learning the theory part in classrooms is paramount during training, an equal effort should be directed to clinical practice. This allows learners to gain skills and a few other things that are not taught in class. Additionally, a clinical culture helps the learners to put the knowledge learnt into practice.
Finally, Haghighat et al, 2020 suggests that nursing students should be trained in health centers owned by their training institutions. In other words the clinical practice should be based on the known institutions. In conclusion, theoretical-practice gap is a universal challenge in the nursing profession and appropriate measures should be put in place to bridge these gaps. The measures suggested above, coupled with other evidence based recommendations can help solve this issue.
References
Arends, R., & Callies, D. (2022). Dissemination enhancement in Doctor of Nursing Practice students. Journal of Professional Nursing, 40, 34–37.
Haghighat, S., Borhani, F., & Ranjbar, H. (2020). Is there a relationship between moral competencies and the formation of professional identity among nursing students? BMC Nursing, 19(1).