Public Health Theory: Supporting Implementation and Health Promotion
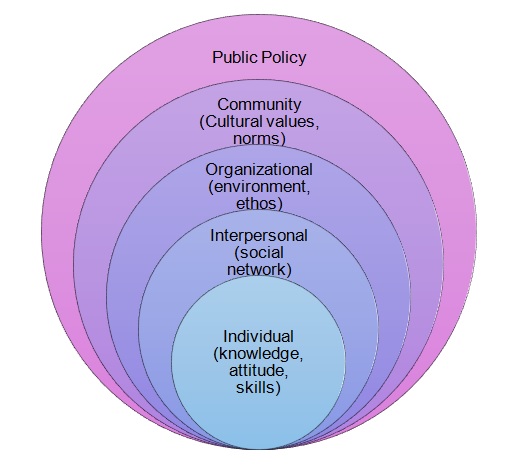
Since the program aimed at managing the issue of obesity implies altering patients’ behaviors and eating habits, a model that encourages change is required for managing the situation. Therefore, change-oriented public health theories will have to be considered. Because of the necessity to focus on both external factors shaping patient’ behavior and the active promotion of family and community support, the Social Ecological Model (SEM) will have to be used. SEM will help embrace the effects of public policies, cultural values and norms, social interactions, and changes occurring at the individual level, such as the acquisition of specific information and skills (see Appendix A).
SEM is essential for managing the problem due to the opportunity for exploring the potential of modern technology, at the same time maintaining the focus on interpersonal communication and individual changes. However, what makes SEM particularly important to apply to the specified concern is its direct connection to the principles of Reciprocal Determinism (RD). By definition, RD implies that a person can play the roles of both a recipient and promoter of change (Golden, McLeroy, Green, Earp, & Lieberman, 2015). Therefore, the SEM framework will enable the target population to take the active part in the recovery process. By involving vulnerable groups into the process of managing their health issues, one will alter the paradigm of patient-nurse relationships by making people with weight issues no longer feel as passive recipients of change. Instead, the framework invites patients to participate actively in the management of their health by deconstructing the communication process and using modern social media as the tools for enhancing patient-nurse interactions.
Although the SEM theory has a number of strengths that make it a sensible choice for implementing the program, it also has several problems that may require further corrections. For example, the fact that it implies dealing with a vast amount of rather subjective data can be seen as a disadvantage because of a possible reduction in the levels of results’ credibility. However, the specified problem can be addressed by introducing the sampling method that will allow diversifying a selected sample to the greatest extent possible. Thus, balanced analysis of the issue can be performed.
The SEM theory will shed light on the nature of the social pressure that patients with obesity experience, as well as on the factors that contribute to the persistence of myths about obesity, in general. The obtained information will inform the intervention approaches for reducing the harm caused by the specified myths and the further promotion of desirable behaviors and attitudes within the community. As a result, comfortable environment in which obese people can start managing their weight and follow prescribed steps will be created.
Evidence-Based Prevention and Health Promotion Activities: Reducing Health Risks
The use of modern media for disseminating crucial information and coaching the target population to lose weight, as well as providing the community with instructions regarding patient support is the key evidence-based prevention strategy. When exploring the problem of obesity, one must consider not only the factors that contribute to weight gain but also the problems that obesity entails. At this point, it needs to be mentioned that a patient may fail to obtain control over obesity depending on the cause thereof. In case hormonal issues such as the malfunctioning of the thyroid gland (particularly, hypothyroidism) are at the root of the problem, the process of addressing obesity must remain under the consistent supervision of a healthcare practitioner (Janssen et al., 2015). In the specified scenario, the issue of social pressure is especially important to address since the society often refuses to see patients with uncontrollable weight gain as such and, instead, considers them lazy and unmotivated (Farhangi, Emam-Alizadeh, Hamedi, & Jahangiry, 2017). Consequently, the problem of social pressure may eventually result in societal contempt for patients and their further ostracism unless managed accordingly.
One must admit that the implementation of the program is fraught with numerous challenges, the dubious impact of social media being the key one. On the one hand, it is important to promote involvement and shed light on the subject of change in attitudes via social networks. On the other hand, studies show that the more time the vulnerable population spends in the online environment, the greater threat of acquiring extra weight they face (Llauradó et al., 2015). Thus, a balanced approach toward the use of modern media must be considered essential. It will be necessary to use social networks as the gateway to providing the target population with extensive information about the management of obesity.
In addition, to prevent the progression of obesity within the target community, one will need to use social media as the means of inviting fancily members and the community, in general, to support people with weight issues. Therefore, the program will also imply working with community members to change the current perception of obese people within the society and affect the dynamics in the relationships between the specified population and the community. Thus, the latter can be shaped not only in terms of the target demographics’ behaviors but also regarding community members’ attitudes toward obese people. As a result, people suffering from obesity will no longer experience the pressure of social contempt; instead, they will feel the support and assistance of their families and friends. The specified setting is expected to contribute to a steep drop in the levels of obesity since the target population will no longer feel the pressure of social prejudice and thus, will not be bound by the overwhelming feeling of guilt.
In addition, one must also consider the use of social media as the place for opening a dialogue with the vulnerable population about their idea of healthy dieting and other concepts related to weight loss. The suggested step is bound to lead to the discovery of a wide range of myths and misconceptions regarding dieting shared by a large number of obese people. For instance, the nature of obesity being solely gluttony is a common misconception that makes patients seem lazy and unmotivated. However, gluttony and sloth are not the only cause of the disorder. Apart from unhealthy eating habits, obesity can occur in patients suffering from hypothyroidism and the Cushing’s syndrome (Collares et al., 2017). Furthermore, several mental health conditions such as depression may contribute to the development of unhealthy eating habits and the following progression thereof, thus leading to obesity (Llauradó et al., 2015). However, the false assumption that people become obese by simply overeating leads to the development of contempt and the following discrimination of people with weight issues. By using social media as the platform for building awareness and educating community members, one will be able to reduce the amount of harm that these myths produce.
Finally, the reduction of health risks will require providing patients with dietary instructions and giving their families and community members pieces of advice regarding the provision of support. Apart from general guidelines such as the importance of positive reinforcement, the proposed instructions will also have to include suggestions regarding communication with the vulnerable population. For example, listing the methods of addressing specific issues delicately will have to be provided. Furthermore, social media platforms can be used to provide online counseling to the families of obese people and community members that need additional information. By establishing a direct dialogue with a nurse or a healthcare expert, one will be able to avoid stereotypical thinking and clichéd arguments that are most likely to lead to a conflict with an obese patient.
Evaluation Program: Determining the Efficacy of Health Promotion Activities
To test the success of deploying the proposed framework, one will have to determine the level of change that will have occurred by the end of the program to the community in question. Seeing that the goals involve primarily altering people’s attitudes toward the phenomenon of obesity, including reducing patients’ fear of ostracism and community members’ disdain for obese people, the assessment process may become complicated. In order to conduct the assessment properly, one will need to set the priorities of the program in line and develop a series of steps for evaluating the progress.
To locate the general effect of the program, one will need to define the percentage of weight loss that will have occurred among the target population by the set deadline. At this point, one must mention that, being attitude-oriented rather than aimed directly at making obese people lose weight, the program in question is likely to require some time to take a major effect on the vulnerable population. Instead, the changes in people’s attitudes toward obesity are seen as the priority.
Determining the shift in the community’s attitude toward the problem, however, must be deemed as the priority and the key objective of the program. Specifically, it will be necessary to ensure that community members and the families of obese people are aware of the significance of their support. A quantitative assessment of the changes in people’s willingness to show their support for people with obesity and their appreciation for patients’ efforts will be required. Furthermore, a qualitative analysis of these alterations in the community members’ perspective will also be necessary in order to understand the current tendencies and ensure that the environment in which patients with obesity live should not become toxic again.
Moreover, the evaluation of the levels of awareness among community members, as well as patients themselves, will be needed. The specified step can be accomplished by inviting the target audiences to participate in a quiz that will provide nurses with detailed results. The link to the questionnaire will be sent to participants after the program is completed. Thus, nurses will receive detailed feedback that will provide an in-depth look into the changes within the community. In addition, this information will inform the further choice of strategies for preventing instances of obesity in the future and providing vulnerable groups with the information that they seek. Since the program is twofold and implies changing the attitudes of both obese patients and people that are prejudiced toward people with weight issues, two types of questionnaires will need to be designed. Thus, one will be able to determine the level of change within both of the specified populations. While the vulnerable group, which includes people with obesity, is the priority, it is also crucial to define the shift that is expected to occur across the community.
However, the data that will be received after the program is completed may be rather intricate and even contrived. The specified phenomenon may occur due to problems in personal perception of the subject matter, as well as a significant degree of subjectivity in participants’ responses. In case a more complex assessment tool is required, one may need to resort to health education intervention trials (Collares et al., 2017). By definition, the suggested tool allows “measuring the inputs, processes, outputs, outcomes and impacts over a longer time horizon” (Kaur, Prinja, & Kumar, 2015, p. 110). Thus, it can be utilized to embrace a wider range of factors when determining the outcomes of the program implementation.
The suggested framework will also serve as the means of evaluating individually the impact of each tool for information dispersion among community members (Kaur et al., 2015). As a result, not only will the superior strategies and devices be identified but also hindrances in the promotion of the program will be located. The significance of a qualitative assessment must not be underestimated in the specified case since it will point to the internal logic of changes in people’s perception of obesity. As a result, the attitudes toward the disorder and obese patients will become easier to control, and the problem of social pressure that patients with obesity experience will become less intense.
When considering interventions for patients with obesity, nurses tend to focus on weight management, which is a natural yet not quite sufficient step to take to handle the concern. Because of the stigma and social pressure experienced by patients with obesity, the active support of family and community members is required. Herein lies the necessity of a massive change in people’s perception of the disorder and the role that they play in its management. While patients with weight management concerns will need to be provided with dietary instructions, their family members and the local community will also have to receive detailed instructions. Nurses must provide families and community members with essential information about assisting obese people, which can be done via social networks as one of the most popular types of modern media.
Therefore, the use of traditional assessment tools for locating the efficiency of a behavioral therapy are crucial in the case under analysis. The program is aimed primarily at altering the behaviors of the vulnerable population and community members, in general, and reducing the intensity of prejudices, in particular. Therefore, it is imperative to introduce both qualitative and quantitative tools for measuring the outcomes. The qualitative analysis will shed light on the direction in which the shift in the audiences’ perception of the problem is geared, whereas the quantitative assessment will help determine the efficiency of the utilized tools. As a result, a comprehensive analysis will be performed, and detailed instructions for improving patient outcomes will be received.
References
Collares, F. M., Korevaar, T. I., Hofman, A., Steegers, E. A., Peeters, R. P., Jaddoe, V. W., & Gaillard, R. (2017). Maternal thyroid function, prepregnancy obesity and gestational weight gain — The Generation R Study: A prospective cohort study. Clinical Endocrinology, 87(6), 799-806. Web.
Farhangi, M. A., Emam-Alizadeh, M., Hamedi, F., & Jahangiry, L. (2017). Weight self-stigma and its association with quality of life and psychological distress among overweight and obese women. Eating and Weight Disorders – Studies on Anorexia, Bulimia and Obesity, 22(3), 451-456. Web.
Golden, S. D., McLeroy, K. R., Green, L. W., Earp, J. A. L., & Lieberman, L. D. (2015). Upending the social ecological model to guide health promotion efforts toward policy and environmental change. Health Education & Behavior, 42(Suppl. 1), 8S-14S. Web.
Janssen, I. M., Homan, J., Schijns, W., Betzel, B., Aarts, E. O., Berends, F. J., & de Boer, H. (2015). Subclinical hypothyroidism and its relation to obesity in patients before and after Roux-en-Y gastric bypass. Surgery for Obesity and Related Diseases, 11(6), 1257-1263. Web.
Kaur, M., Prinja, S., & Kumar, R. (2015). Evaluating the performance of health promotion interventions. The Indian Journal of Medical Research, 142(2), 109-112. Web.
Llauradó, E., Aceves-Martins, M., Tarro, L., Papell-Garcia, I., Puiggròs, F., Arola, L.,… Giralt, M. (2015). A youth-led social marketing intervention to encourage healthy lifestyles, the EYTO (European Youth Tackling Obesity) project: A cluster randomised controlled trial in Catalonia, Spain. BMC Public Health, 15(1), 607-615. Web.
National Institute of Health. (n.d.). Social and behavioral theories. Web.
Appendix A