Introduction
The paper has provided two designs for experiments as an alternative for the diagnosis and treatment of Borderline Personality Disorder (BPD) The paper has first presented the existing treatment, diagnosis and treatment of BPD and then provided two experiment designs. The first experiment is based on the Hamilton Depression Scale (HAMD) and the other on the Dissociative Experiences Scale.
Existing Treatment on BPD
Martens (2005) has presented extensive research on Borderline Personality Disorder (BPD). According to the author, Borderline personality disorder (BPD) is characterized by a pervasive pattern of instability in affect regulation, impulse control, interpersonal relationships, and self-image, as well as frantic attempts to prevent abandonment, self-mutilating or suicidal behavior, chronic feelings of boredom or emptiness, and brief paranoid ideas or severe dissociative symptoms related to stress (American Psychiatric Association, 2000).
BPD patients often have multiple severe and chronic behavioral problems, including suicidal and other self-injurious behaviors, which make them frequent users of mental health resources. Causal factors are only partly known, but genetic factors and adverse events during childhood, such as physical and sexual abuse, contribute to the development of the. Patients who meet criteria for BPD are prevalent in clinical practice, comprising about 10% of psychiatric outpatients. They usually are difficult to treat, and some forms of treatment may even lead to their problems becoming more severe; therefore, clinicians may feel frustrated, incompetent, or hopeless about the patient.
Therapy is often complicated by co-morbid Axis I and/or Axis II disorders. BPD is usually accompanied, for example, by one or several of the following symptom disorders: eating disorders, depression, posttraumatic stress disorders, premenstrual tension, dissociative disorders, or anxiety disorders–not to mention one or more additional personality disorders. The accompanying personality disorders will have an impact on amenability to psychotherapy.
The treatment presented by Martens (2005) has used previous research, developed, refined, and tested Dialectical Behavior Therapy (DBT), a principle-based psychotherapy for chronically parasuicidal women with borderline personality disorder. DBT utilizes both established change interventions from cognitive-behavioral therapy and acceptance strategies from humanistic therapy and Eastern and Western meditative practices (Fruzetti). DBT also shares elements with psychodynamic, client-centered, gestalt, paradoxical, and strategic approaches. Both acceptance and change strategies are dialectically balanced or synthesized into a multicomponent treatment program.
DBT provides structured telephone contacts with individuals diagnosed with borderline personality disorder that emphasize the role of learning principles. The author attempted to find out four characteristic problem areas that are often found among multiproblem borderline patients and they are confusion about self, impulsivity, emotional instability and interpersonal problems.
The author examined, in a nonrandomized sample of suicidal DSM-IV BPD patients (n=27; 14-19 years old), self-reports of the helpfulness and overall effectiveness of four skills (mindfulness, distress tolerance, emotion-regulation, and interpersonal effectiveness skills) using pre- and post-treatment evaluations and found significant reductions in BPD symptoms in all four problem areas (confusion about self, impulsivity, emotional instability, interpersonal problems). The most highly rated skills included distress tolerance and mindfulness skills.
The The author in a prospective randomized controlled study of the chronically suicidal women revealed that DBT (n=24) compared with TAU (n=23) showed a wide variation in the results in parasuicidal behavior (repeat rate between 26% and. 60%). DBT patients were significantly more likely to drop out of treatment (83% to. 42%) and had fewer inpatient hospital days than the TAU subjects. Treatment duration was 12 months. The DBT program included individual psychotherapy, 150 minutes of group skills training, didactic and homework review, and consultation teams.
First Design – Hamilton Depression Scale (HAMD)
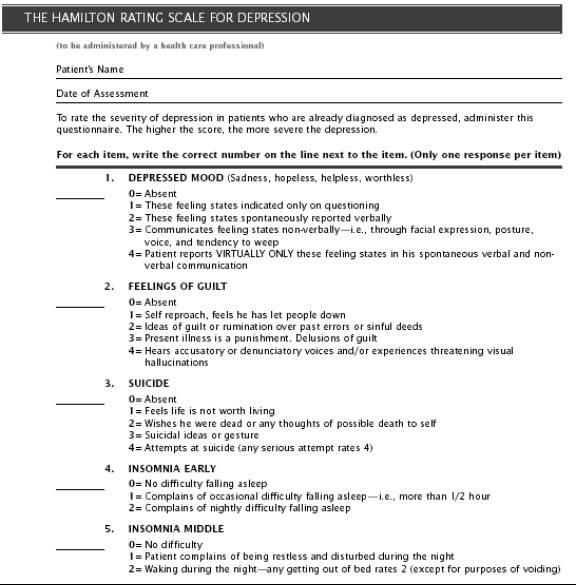
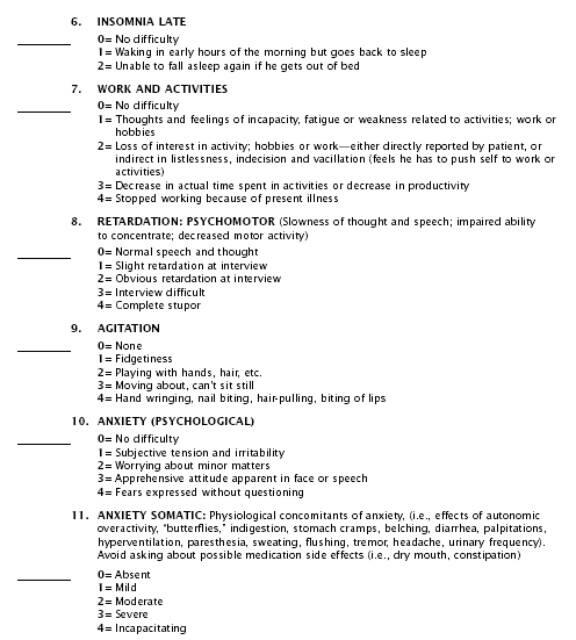
Hamilton (1960) first proposed the Hamilton Depression Scale (HAMD) that is a 17 to 21-question survey instrument that is used by the doctor to rate the severity of depression. Please refer to Appendix 1. Hamilton Depression Scale. The instrument is not self-administered but needs to be only used by the doctor while examining the patient. Individual patients are asked to relax while the doctors asks a number of questions that relate to examining the patient so that the doctor can form an assessment of the severity of the case. The value of scale, and its limitations, can best be considered against its background, so it is useful to consider the limitations of the various rating scales extant.
They can be classified into four groups, the first of which has been devised for use on normal subjects. Patients suffering from mental disorders score very highly on some of the variables and these high scores serve as a measure of their illness. Such scales can be very useful, but have two defects: many symptoms are not found in normal persons; and less obviously, but more important, there is a qualitative difference between symptoms of mental illness and normal variations of behavior. The difference between the two is not a philosophical problem but a biological one. There is always a loss of function in illness, with impaired efficiency.
The test is used to measure a number of parameters it originally had 17 variables and these have been increased by different researchers over the years. The test has four possible ratings that the doctor can use to identify the symptoms. The variables measured are: given in the following table.
The test needs to be administered to patients who have been preliminarily identified as having BPD.
Hamilton recommends that it is particularly useful to have two raters independently scoring a patient at the same interview, since this gives data for calculating the interphysician reliability. The score for the patient is obtained by summing the scores of the two physicians. This is, of course, the best way of learning how to use the scale, Where only one rater uses the scale, the scores should be doubled so as to make them comparable. With sufficient experience, a skilled rater can learn to give half-points.
Hamilton has suggested using the scoring Factor methodology.
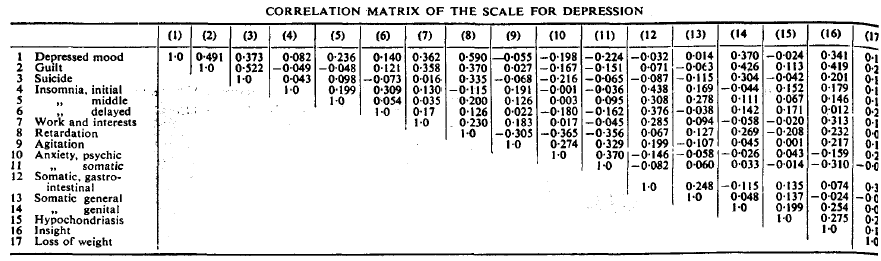
The following table provides the score for factor saturation and latent roots
Hamilton speaks of the strengths of this test since the control would be in the hands of doctors who would be able to make a proper testing and diagnosis. The author has claimed that the test has advantages over self-administered tests, which are noted for inconsistencies, errors and bias as respondents for self administered tests tend to show hesitancy during the testing.
Hamilton again speaks of certain limitation, the main being that everything is left to the doctor who administers the test. A lot would depend on the skill level of the doctor and some inherent preconceived notions or bias that the doctor may have. But again Hamilton has suggested that two doctors administer the test and that the resulting score should be added and halved.
Second Design – Dissociative Experiences Scale (DES)
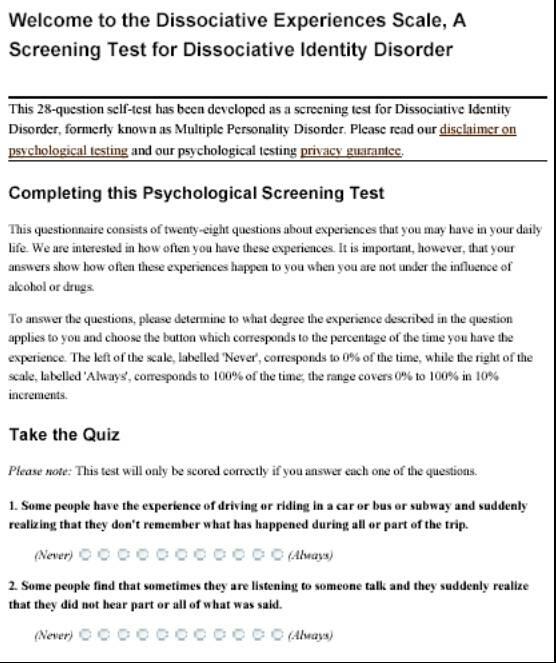
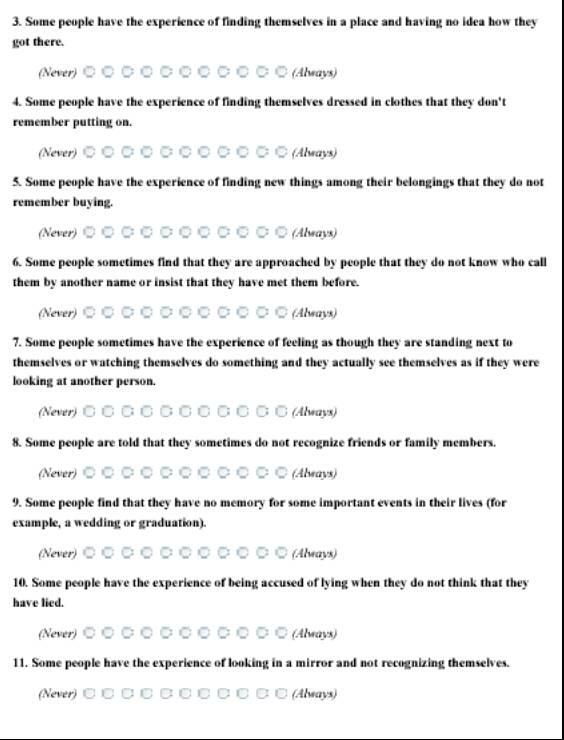
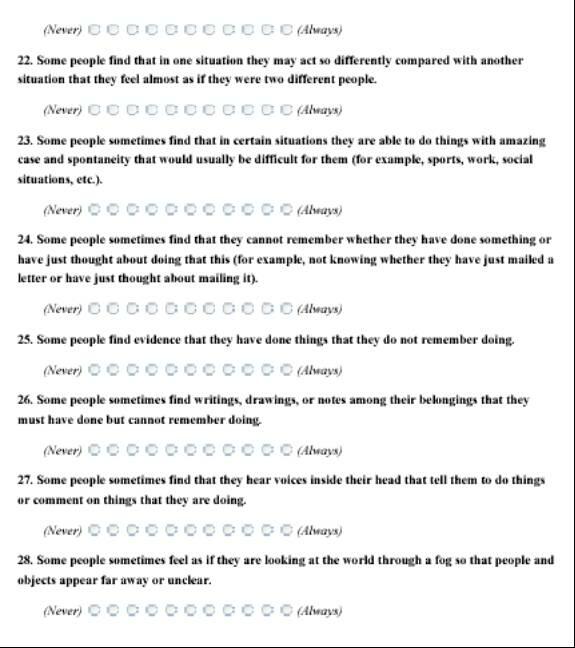
Maulhauser (12 December 2007) has written that the DES scale, developed by Eve Bernstein Carlson, Frank W. Putnam, is designed to help identify patients with dissociative psychopathology and as a research tool to quantify dissociative experiences, This is a self administered test and has a set of 28 questions with different variables. This is a self administered test and is to be used as a starting point and should not be used as a tool for diagnosis.
The score will help patients to develop a better understanding of themselves and their mental state. The Dissociative Experiences Scale is designed to identify people with dissociative psychopathology. It provides a means of quantifying dissociative experiences. The scale uses a number of broad range of dissociative variable and these include disturbances in memory, identity, and cognition, and feelings of derealization, depersonalization, absorption, and imaginative involvement. Please refer to ‘Appendix 2. Dissociative Experiences Scale’ for details about the test.
Maulhauser reports that the DES uses a visual analogue scale that requires examinees to mark their responses along a numerically anchored 100-millimeter line. Item responses range from 0%, “This never happens to you,” to 100%, “This always happens to you.” The DES II uses a more convenient 11-point Likert scale. Total scores are obtained by averaging the 28 item scores. Maulhauser suggests that that the DES yields reliable scores in many assessment contexts and has a validity and reliability between 85 to 93 percent.
The author also suggests that the primary validation studies with the DES feature Spearman rank-order correlations of the instrument with age and socioeconomic status. Item-total correlations also use this statistic.
In the experiment, non-random patients would be subjected to the test and the responses measured as a percentile value. The test can be used as the starting point to support later studies and the test reflects what the patients feel about themselves.
As mentioned by Maulhauser, the test would put the control in the hands of the patients and they may exhibit a tendency to select answers that seem correct and not what they actually feel. This may lead to errors and bias. In any case, later therapy sessions and interviews with doctors would reveal the extent to which the patient attempted to manipulate the results.
Conclusion
The study has presented two designs that would be used in place of a published report to study the issues associated with Borderline Personality Disorder (BPD). The paper has first presented the existing treatment, diagnosis and treatment of BPD and then provided two experiment designs. The first experiment is based on the Hamilton Depression Scale (HAMD) and the other on the Dissociative Experiences Scale. The designed instrument along with the variables, scoring methodology and other details have been presented.
References
Hamilton Max (1960), A Rating Scale for Depression. Journal of Neurology, Neurosurgery and Psychiatry, Volume 23, pp: 56-62
Maulhauser Greg, 2007. Dissociative Experience Scale. Web.
Martens Willem H.J (2005), Therapy on the Borderline: Effectiveness of Dialectical Behavior Therapy for Patients with Borderline Personality Disorder, Journal of Annals of the American Psychotherapy Association, Volume: 8, Issue: 4, pp: 5 – 10.
Appendix