Abstract
Self-isolation is an essential policy and practice to stop the pandemic spread, and many countries introduced a series of mandatory lockdowns. However, there is a cost to this practice: isolated people tend to have mental issues connected with loneliness, fear, and the inability to contact those they love. The current research aims to find ways to help people in isolation, primarily in hospitals, who are separated from their friends and family. Literature for the research was searched via PubMed database and free search in Google Scholar. An article was considered relevant if published at least in the 2020 year in the English language and explores the themes of social isolation during COVID-19 and its consequences. Articles that highlight the hospital-based isolation and its outcomes are preferred over those highlighting self-isolation, and those providing recommendations about the patient support are preferred over those that do not. There was found and shown that hospital isolation is connected with mental health issues, loneliness, anxiety, feeling of restriction, and a lack of freedom. The feeling of grief and bereavement is often present in patients and their relatives due to the fear of death connected with the COVID-19. The usage of social media for communication, the help of a mental health specialist, and ensuring enough free space and privacy for all patients may lower those negative consequences. In addition, transparent communication between hospital staff, patient, and relatives are crucial for the information provision and maintenance of good relations: it reduces anxiety and feeling of loneliness. To implement those recommendations, hospitals should train staff to work with isolated patients, allocate free space for them, and cooperate with local public health facilities.
Introduction
Isolation is necessary during the COVID-19 pandemic, as it stops its distribution; however, new problems emerge due to a lack of social contacts, restricted freedom, and separation from friends and family. When patients are isolated in hospitals, away from their friends, family, and daily routine, the staff is responsible for their well-being and should appropriately detect and address those issues. They may include mental issues, bad emotions, a feeling of being restricted, and anxiety. Those issues are to be studied in the current review, and recommendations about how they may be solved are formulated.
Search Strategy
Evidence from other studies should be used to support the thesis: in the case of the current review, to show how patients can be supported during the COVID-19 isolation in hospitals. To meet this aim, nine sources are enough, and they should be connected with the isolation due to COVID-19 and social support. The process of selection in the form of the PRISMA diagram is shown in the Figure 1. All articles should be published between 2020 and 2022, as the pandemic started in 2020, and all articles published earlier are not relevant to it; other criteria may be seen in the Table 1.
Themes of COVID-related isolation, mental health, and hospital policies are crucial. While several of those articles may be dedicated to self-isolation as they may contain important information about the patient support, most of them should be connected with the hospital isolation (Hsiao et al., 2021; Sahoo et al., 2020; Saltzman, Hansel, and Bordnick, 2020). The influence of isolation on mental health is another topic of interest for the current research (Kumar and Nayar, 2020; Pancani et al., 2021). Some of the included articles explore related themes, such as supporting bereaving people, general recommendations to hospitals, and COVID-19 policies (Chopra et al., 2020; Chung et al., 2021; Selman et al., 2020; Wang et al., 2021). Many articles research the biological and physiological effects of the COVID-19, and their areas of interest are molecular biology, virology, and biochemistry. Those articles are excluded as they do not research the psychological and social effects of the disease.
Table 1: A search strategy
PRISMA Flowchart
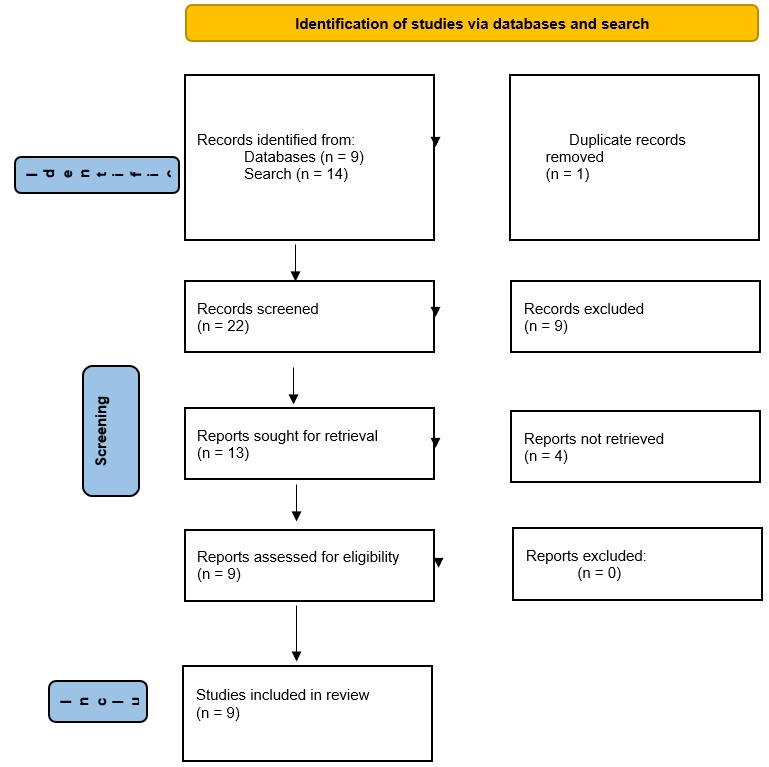
Table of Evidence
While being a necessary measure to prevent the COVID-19 distribution, self-isolation creates new troubles, which should be addressed and solved. The necessity of isolation is demonstrated by the Chinese experience, where a harsh lockdown is implemented directly after the disease is identified (Wang et al., 2021). As a result of such centralized isolation, the disease was quickly defeated in China, and the number of COVID-19 cases in the country remains low. However, forced isolation leads to a drastic decrease in life quality, a rise in mental health problems, increased loneliness and anxiety, and general bad feelings and emotions (Pancani et al., 2021). The find, test, trace, isolate, support (FTTIS) strategy is proposed to maximize the benefits of isolation while minimizing its adverse outcomes (Chung et al., 2021). Hospitals should be prepared to allocate free space and resources, train teams to support patients, and provide all data in open access, easing the communication with patients and their relatives and decreasing their anxiety (Chopra et al., 2020). All those issues, approaches to solving them, and recommendations for implementing those approaches are to be discussed.
Troubles Associated with the Isolation
The main problem is mental issues, resulting from prolonged isolation from society, people, the common life routine, and loved ones. Children are especially vulnerable due to their developing psyche and often inability to understand why they need to be isolated (Sahoo et al., 2020). All ages, however, are susceptible to that: a long loneliness period negatively correlates with mental and physical health (Saltzman, Hansel, and Bordnick, 2020). People in isolation tend to be afraid and blame themselves for creating trouble; they have the risk of social phobia development (Hsiao et al., 2021). They often lose their jobs, and their well-being thus, decreases; due to the collapse in their daily routine, they often have suicidal tendencies, regardless of whether they are self-isolated or in hospitals (Kumar and Nayar, 2020). In that way, various mental issues are the most important issue during the isolation, and they should be addressed.
The inadequate place of isolation is another issue: all patients should have enough space, sufficient brightness, and be sure that their privacy will not be violated. There is evidence that the more adequate space available for patients, the better their mental health is (Pancani et al., 2021). Hospital free space and resources should be allocated, thus, in a way to guarantee that all patients will have access to the services they are needed (Chopra et al., 2020). Developing a good infrastructure in hospitals is crucial for stopping the spread of the pandemic and ensuring the well-being of patients (Chung et al., 2021). Therefore, a lack of free space worsens the patients’ conditions, and it is another widespread problem that should be addressed.
Addressing Troubles: Recommendations
Most mental issues can be solved with a mental health specialist’s timely and efficient help. The lack of a qualified mental health specialist is a big challenge, which may be overcome by training the hospital staff to be empathetic and supportive (Kumar and Nayar, 2020). Social networks enable receiving psychological help online, which is much quicker than direct visiting, and more comfortable for both specialist and patient (Chung et al., 2021). Grief management is a set of practices aimed at decreasing the bad feelings in patients and their bereaving relatives (Selman et al., 2020). They include the provision of communications via the Internet, telephone, or letters, and psychological, emotional, and spiritual support. Self-care is another essential element of patient support: the hospital staff should teach patients to care for themselves appropriately, which will improve their well-being (Hsiao et al., 2021; Saltzman, Hansel, and Bordnick, 2020). It is recommended that the hospital staff ensures that all patients have access to the mental health facilities and, in addition, that nurses can provide at least basic mental health by themselves.
Social isolation may be eased with the usage of social networks, which are very popular in modern days. The social contact number positively correlates with the patient’s well-being, especially during the long isolations, more than one month (Pancani et al., 2021). Wide technology access in the times of the COVID-19 pandemics is a unique opportunity to become more resilient to the isolation outcomes (Saltzman, Hansel, and Bordnick, 2020). It is beneficial for children, particularly vulnerable to the isolation’s adverse outcomes (Sahoo et al., 2020). The recommendation is that all patients should have a connection with the outer world via Internet services, and if they cannot provide it for themselves, hospital staff should help them.
Information transparency and the developed hospital infrastructure are promising approaches to address troubles with anxiety and fear connected with the COVID-19 isolation. It means open access to all information about the coronavirus, disease, isolation terms, and necessity, what is permitted and forbidden during it, and why (Chopra et al., 2020; Chung et al., 2021; Hsiao et al., 2021; Selman et al., 2020). In addition, hospitals need to be sure that they have enough free space for current and future patients and that their privacy is ensured (Chopra et al., 2020; Pancani et al., 2021). Such an approach reduces anxiety and makes patients more confident, as they will have enough information about their condition (Chung et al., 2021). Open information access reduces the feeling of grief connected with the disease in patients and their relatives, especially in the case of acute disease (Selman et al., 2020). By providing the information transparency and allocating their resources, hospitals would substantially improve the well-being of their patients.
Critical Appraisal
Experience of patients with COVID-19 in hospital isolation in Taiwan (Hsiao et al., 2021)
This is a primary study connecting with the COVID-19 patients in hospital-based isolation: in this way, it is the relevant article for the current review. It aimed to explore two themes: the psychological effect of the hospital isolation on patients and their behavior during the isolation. Based on those findings, approaches to improve their psychical conditions are proposed. In-depth interviews were used to obtain the data, and nine patients from a northern Taiwan hospital were interviewed via Google Meet. Content analysis, then, was applied to the interviews to elucidate the interviewees’ problems, troubles, and what is important to them. Results show that patients have increased anxiety, tend to blame themselves, and feel a lack of freedom. A good supply of information and the ability to use social networks and phones to contact friends and relatives help them recover.
Thus, the article explores how hospital patients behave in the conditions of total isolation. Their feelings, emotions, and thoughts are recorded, which is valuable information about the isolated COVID-19 patients. Based on the content analysis, while the limitation is that the data are entirely relevant only for the Taiwanese conditions, general results may be extrapolated to other hospitals and patients. For example, hospitals may increase the well-being of isolated patients by simply improving their access to information about the virus and isolation and ensuring that they have contact with relatives.
Forced Social Isolation and Mental Health: A Study on 1,006 Italians Under COVID-19 Lockdown (Pancani et al., 2021)
This article is a primary study: it explores the one thousand Italians who are in isolation due to the COVID-19 lockdown to assess their conditions, understand the factors that increase or decrease their well-being, and how they may be addressed. Participants were chosen from the largest number by their willingness to participate in the study, eligibility (for example, they need to be in Italy), and the consent given. The survey was used for this research: each participant was asked to provide short answers to measure their level of depression, anxiety, the frequency of contact with people, the closeness to people they contact with, and how appropriate the places they reside. The importance of this research is that it shows the patterns which influence people’s well-being during isolation. While this study is dedicated not only to those residing in hospitals, it is relevant for the current paper, as those patterns apply to patients in isolation, too. For example, the research highlights the importance of free space and privacy for the patients and the sufficient information supply.
Conclusion
Hospital isolation is a vital emergency measure necessary to stop the proliferation of the COVID-19, but it is connected with various troubles, and all of them should be highlighted and addressed. First, the prolonged isolation leads to the feeling of danger and loneliness and then mental issues. Second, poor hospital infrastructure, insufficient free space, and the lack of information worsen the former trouble and the patient’s well-being in general. All those problems may be solved by timely psychological aid, well-planned hospital infrastructure, information transparency, and ensuring the patient’s contact with the outer world via the Internet or telephone.
Reference List
Chopra, V., Toner, E., Waldhorn, R. and Washer, L. (2020). ‘How Should U.S. Hospitals Prepare for Coronavirus Disease 2019 (COVID-19)?’ Annals of Internal Medicine. doi:10.7326/m20-0907.
Chung, S.-C., Marlow, S., Tobias, N., Alogna, A., Alogna, I., You, S.-L., Khunti, K., McKee, M., Michie, S. and Pillay, D. (2021). ‘Lessons from countries implementing find, test, trace, isolation and support policies in the rapid response of the COVID-19 pandemic: a systematic review.’ BMJ Open, 11(7), p.e047832. doi:10.1136/bmjopen-2020-047832.
Hsiao, C.-T., Sun, J.-J., Chiang, Y.-H., Chen, H.-L. and Liu, T.-Y. (2021). ‘Experience of patients with COVID-19 in hospital isolation in Taiwan.’ Nursing & Health Sciences, [online] 23(4). doi:10.1111/nhs.12878.
Kumar, A. and Nayar, K.R. (2020). ‘COVID 19 and its mental health consequences.’ Journal of Mental Health, [online] 30(1), pp.1–2. doi:10.1080/09638237.2020.1757052.
Pancani, L., Marinucci, M., Aureli, N. and Riva, P. (2021). ‘Forced Social Isolation and Mental Health: A Study on 1,006 Italians Under COVID-19 Lockdown.’ Frontiers in Psychology, [online] 12. doi:10.3389/fpsyg.2021.663799.
Sahoo, S., Mehra, A., Suri, V., Malhotra, P., Yaddanapudi, N., Puri, G.D. and Grover, S. (2020). ‘Handling children in COVID wards: A narrative experience and suggestions for providing psychological support.’ Asian Journal of Psychiatry, [online] 53, p.102207. doi:10.1016/j.ajp.2020.102207.
Saltzman, L.Y., Hansel, T.C. and Bordnick, P.S. (2020). ‘Loneliness, isolation, and social support factors in post-COVID-19 mental health.’ Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), pp.S55–S57. doi:10.1037/tra0000703.
Selman, L.E., Chao, D., Sowden, R., Marshall, S., Chamberlain, C. and Koffman, J. (2020). ‘Bereavement Support on the Frontline of COVID-19: Recommendations for Hospital Clinicians.’ Journal of Pain and Symptom Management, 60(2), pp.e81–e86. doi:10.1016/j.jpainsymman.2020.04.024.
Wang, X., Wang, J., Shen, J., Ji, J.S., Pan, L., Liu, H., Zhao, K., Li, L., Ying, B., Fan, L., Zhang, L., Wang, L. and Shi, X. (2021). ‘Facilities for Centralized Isolation and Quarantine for the Observation and Treatment of Patients with COVID-19: Experience from Wuhan, China.’ Engineering, 7(7). doi:10.1016/j.eng.2021.03.010.