Introduction
The background of the management problem
Health care management has been the preserve of qualified and trained managers since time immemorial. The advent of specialisation in health care has opened doors for the incorporation of professional health workers in management. Although little achievement has happened in this direction, debate is gathering momentum on the role professionals ought to play in the running of health care particularly in the United Kingdom.
The United Kingdom is among the most developed economy in the world in terms of its gross domestic product. Health care is mainly provided by the government funded by the National Health Service (NHS) that is supplemented by efforts from the private sector. The National Health Service runs all the public hospitals and serves slightly more than 90% of the population. Since its inception by an act of parliament in 1946, the NHS has continued providing primary care and inpatient treatment care. With a workforce estimated at more than 1.3 million, the NHS spends a large portion of its funds in remuneration of managers who are not professional health workers. This came into effect in late 1980’s when the government introduced policy changes that underscore the need of general managers to boost efficiency and accountability in the hospitals. The policy also recommended the active involvement of clinicians in the overall running of health, although at lesser extent. Despite many years of policy changes on management and service delivery, the NHS has continued to experience financial pressures due to changing dynamics of health care such as insurance, aging population and improved technology (National Health Service, n.d., para. 1).
Introduction to the Management Problem
Management entails aspects of getting activities done efficiently and effectively by engaging services of other people in an organization. Health care management involves integration of leadership abilities, management prowess, and aspects of administration in health care facilities. Health care management is imperative in the determination of the overall health status of a country population. Furthermore, health has been closely linked with economic development owing to the destabilisation of workers productivity that may result to ill health. Management entails many intertwined roles that enhance the achievement of positive benefits. According to Mintzberg (1973), the roles of a manager have surpassed those advocated by the classical literature. In addition to the planning, coordination and financial management, the managers are supposed to play interpersonal and decisional roles as well as act as information agents of their organisations (Mintzberg, 1973).
Health care management refers to the overall running of activities related to prevention and treatment of illness and diseases as well as the maintenance of physical and mental well being (National Health Service, n.d., para.2). The health care services are offered through the concerted efforts of nurses, doctors and other specialised and unskilled workforce. Management in all areas including health care entail encompass the planning, staffing and organising supplemented by leadership and control (Whittington 1994, p.12). Taking into considerations the level of investments made in health care, there is need to have very competent individuals mandated to manage the resources. Effective application of managerial skills will result in the development of solid health institutions with the ability to provide quality services to the citizens. Management also endeavours to follow laid down policies that are vital in guiding the institutions in the achievement of specific objectives and goals. It is therefore an integral aspect of any organisation since it links up the various actors and factors of production. This is evident in hospitals where the first line managers shoulder much of the responsibilities of linking up the patients, staff and senior managers (Duffield, 1992, p.42). The possession of managerial skills comes in handy in the exercise of daily routines that require a wide variety of competencies.
Management in the healthcare organisations has taken different twists in the last few decades owing to various policy changes aimed at addressing the problems plaguing the health sector. The understanding of the functioning of the healthcare system is imperative in the achievement of efficacy and effectiveness in the overall running of the institutions. The linkage of technicalities from the first line to the top brass of management has greatly improved thereby resulting in timely action on pertinent issues. Moreover, involvement of professionals from different cadres of health workforce helps bring synergy that is crucial in coordination and communication. The application of laid down guidelines respects the various regulations governing the professional performance (Duffield, 1992, p.42).
The National Health Service has continued to experience budget deficits despite investing in the hiring of trained managers (Witz, 1994, p. 10). The over-dependence on managers has been criticised thereby making the hospitals to start embracing the clinicians as a core component of their management. Recently, the labour government led by Gordon Brown has increasingly advocated for the scaling down on managerial jobs thereby giving the doctors more leeway in the management of the institutions.
The overdependence on this cadre of workers to deliver change in the health care institutions has received criticism from previous studies. The embracement of clinicians in the management is not new to United Kingdom since the last decade has seen its slow implementation. Leatt (1994, p. 171) asserted that an ever increasing number of physicians were expected to involve themselves in managerial work, in addition to their professional activities. However, discontent has occurred with several analysts arguing that conflicting roles will ensue. Their argument pegs on whether there will be effective delivery of teaching, clinical care or even research in line with the newly acquired managerial duties. The excellent performance of the clinicians and physicians in junior levels of management has endeared the physicians to policy makers who are continuously pushing for the downscaling of managers in favour of the clinicians. Despite putting in place several policy measures in terms of hospital management, severe problems in the management and service delivery persist.
Research work has continuously delved on the variations witnessed in managerial work while paying scant attention on how the evidence can be utilised to impart on the managerial practices. The mere description of the features that depict managerial work and theories that fail to link the relations between managerial works with the research findings serves to justify the need to undertake a study on this topic. This worsens due to the lack of adequate information that depicts how, the reasons managers are able to reaffirm the norms, and to a smaller extent the meanings that enhances the interaction of the managerial practices (Hales, 1999, p.372-373). This study is therefore imperative in the determination of the degree the clinicians are involved in management while also checking their impact in service delivery.
Statement of the Management Problem
The United Kingdom cannot continue relying largely on trained managers in the overall running of health care system who have failed to achieve the desired expectations in terms of accountability and governance. The exorbitant fees paid to the managers as remuneration has continued influencing negatively on the budgetary allocation to NHS thus the need to embrace the clinicians as integral component of the management. Minimal research has occurred on the factors and implications of the switch to managerial duties by the clinicians. Of particular importance, are the policy implications needed in place in order to achieve maximum productivity of the professionals and health care organisations while minimising the role conflicts among the various stakeholders.
The role and Competencies of Managers
Managers have become integral part of any organisation and business because of their ability to link up the factors of production and the various actors. Hales noted that managers have a propensity of indulging much on the daily activities that involve supervision of the workforce and ascertaining everything is in order at the workplace (2001, p.52). The most common features of this work include involvement in fragmented activities, usually interrupted, and the propensity to address the urgent rather than the planned activities. The irresistible obligation to provide solutions to problems affecting the work processes. More importantly, is the increasingly indulgence in all types of communication (Hales, 1999, p. 338). Communication plays a big role especially when dealing with the internal and external environment. In this regard, the managers have to display impeccable communication skills especially when dealing with situations concerning the welfare of the workforce or reputation of the organisation.
In order to understand the specific roles of managers, it is imperative to list the purely managerial duties and separate them from the normal duties. Avoidance of the assumption that everyone knows what managerial work entails is paramount while substantive linkages between who and what they are need explanations in terms of positive or negative impacts on effective management (Hales, 1999, p.336). This is imperative since it helps remove the ambiguities and controversies that surround the role played by the management.
There has been much debate on the role of managers because of several factors. In their course of action, the managers need observe guidelines and take into consideration the objectives of the organisation before embarking on a certain course of action. According to Mintzberg (1973), managerial work is greatly informed by several schools of thought. The classical school is reliant with the five basic functions expected of all managers. Apart from planning, coordinating and organising, the managers are also expected to command and control the functioning of the institution and the workforce (Hales, 2001, p.50-53). Today, managers have to offer motivation to the work force while at the same time exerting their influence in the overall staffing of the institutions. In fact, innovation is the single most activity that distinguishes a successful manger from the rest. Management requires a lot of courage, effective communication skills, determination and a combination of the right skills for success to be achieved in the negotiations or in the achievement of the long-term goals of the organisation (Mintzberg, 1998, p.142-144)
Mintzberg (1973) noted that managers indulge in several roles while executing their responsibilities. Interpersonal roles play a major role in ensuring the togetherness of the workforce (Mintzberg 1973). The manager acts as a figurehead and a leader upon whom others seek direction or help. Communication roles help the manager to interact with various stakeholders and effectively deal with the workforce. More importantly, the manager must have the ability to monitor and disseminate information while at the same time act as a spokesman of the organisation in different forums. The informational roles are important in health care setting since the working environment requires accuracy when making decisions particularly on the course of action to take when dealing with a patient. The exposure of the organisations to the harsh work environment requires the managers to make strategic decisions regarding the operations. In this case, the health care manager must be in the forefront in the initiation and development of change management. Monitoring and evaluation capabilities assist in analysis of the situation before corrective measures are applied especially when there is a deviation from the initial plan. Problem solving is another unavoidable role that the manager must struggle to execute diligently. Problem solving may involve the internal conflicts witnessed within or those pitting the organisation with others. Resources form the foundation of any organisation and as such, the manager must be ready to allocate the resources appropriately while keeping in mind the time, programme and formalities involved in the process (Hales, 2001, p.50-53).
Effective management requires the managers to have a combination of the skills. Proper utilisation of communication and decision making skills have continuously propelled their careers while helping the organisation build its image. Moreover, information gathering has proved instrumental particularly when the institutions are planning to initiate change management. For the managers to perform the above roles efficiently, they must have the following competencies. The managers must be progressive and results focussed by directing the team towards the right path of prosperity. According to Hales (2001, p. 50-58), managers must be competent in planning the financial and human resources and be willing to develop a cohesive and focussed team that will push forward the desired change. Possession of powerful decision making and communication skills also affects the change management. Health care managers must listen to their juniors and patients in order to effectively address their concerns Hales (2001, p. 50-58). Managers must embrace and act on the positive feedbacks and criticisms from the stakeholders since this will greatly inform the final decisions on paramount issues in the organization.
Professional as Managers in Health Care Settings
For many years, managerial positions were the preserve of professionally trained managers. However, following the dismal performance of the health care units, several government regimes embarked on a restructuring plan that resulted in the development and implementation of policy papers in the last two decades of 20th century. The integration of managerial and clinical practice received mixed reactions from various stakeholders. This ushered the integration referred to as the ‘two window’ in reference to the two roles assigned to the professional. The metaphor represented a great interchange that embraced transparency and openness in the running of health care. The introduction of this concept served to bridge the gap that existed in the earlier years.
Bolton noted that since early 1990, the government has embraced the role played by the nurse in the delivery of quality patient care and organisation of NHS (2005, p.6). Although the first line managers existed before this directive, they actually received a major boost since they could progress to the middle level management (Duffield 1994, p. 49). International evidence provides interesting insights. Canada is experiencing the same problem of health professionals taking up managerial jobs (Duffield 1994, p.50). However, the change is due to a constellation of internal and external factors in the health care system. The ever rising costs of health care buoyed by advancements in technology and insurance premiums has worried the government making it to institute policies to regulate the medical practice. Furthermore, increased pressure particularly from the medical fraternity and the decline in demand for medical professionals has resulted in the diversification into other areas.
Likewise, nurses are lured into managerial positions as part of normative device that is aimed at regulating the work pool by reducing competition through diversification of roles (Bolton, 2005, p.7). Canada thus has experienced the surge in the number of physicians holding top managerial positions with health care providers and learning institutions. The Canadian hospitals have increasingly tapped the potential by offering them high-level positions as administrators, board members and trustees. This has propelled into decision-making organs where they delve on strategic planning and financial management (Leatt, 1994, p.171-173). Australia has also embarked in change management where the nurses are assigned several roles to maximise their productivity. According to Duffield (1994, p.49), the nurses, who act as first line managers, are assigned triple roles aimed at promoting and maintaining clinical excellence in the institutions. More importantly, the nurses are burdened by the workload combined with the high standards of accountability required of them. The situation is complicated by the changes in patients, organisational and nursing dynamics (Duffield, 1994, p. 50).
The opening up of managerial positions has resulted in conflict in the workplace by advocating a performance culture. The nurses are pushed to deliver care at the lowest cost possible thereby bringing into fore the probability of poor quality care for patients (Bolton, 2005, p.6). Furthermore, the switch aims at realigning the medical profession from their normal duties where the administrators supervised them. The sense of autonomy and empowerment that comes with the positions is construed to be a part of a wider scheme of normative control aimed at silencing the professionals, eventually endearing them to managerial positions. The two-window system is detrimental in career advancements since the professionals lose their focus, thereby concentrating more on managerial roles. The nurses become overly frustrated by the system on realising they are overburdened with responsibilities. This worsens due to the tight budgetary controls and ambitious measures and targets aimed at improving their performance. This system has posed ethical dilemmas to the professionals since they feel compromised by accepting to offer poor quality care while the institution reap considerable profits (Bolton, 2005, p.7).
The physicians also face conflict in their execution of their roles. The physicians not only oversee activities in the health care organisations, but also protect the patients from any harm or harassment when accessing medical services. Ethical dilemma results in case of an eventuality where the patient and the employer are involved. Furthermore, the physicians act as part of a convoluted network of professionals who uphold some standards and values as part of their broad mandate. The network also called role set comprises the patients together with the other members of the professional fraternity. A role conflict may ensue particularly when there is a disagreement or failure to satisfy expectations of one or all of the members. Such instances are vey critical to the professional since it may lead to a negative eventuality. Role conflict is believed to take the following forms; instances when the professional association is convinced that the physician manager has deserted the profession by spending lengthy duration of his/her time in managerial duties; and involvement in teaching or research ventures may be against the expectations of the employer. Role conflict occurs when organisational decisions touching on programs targeting patients have negative implications in their life and health (Leatt, 1994, p.173-174). Role conflict is a dilemma that faces the healthcare professional thereby forcing them to strike the right balance between their professional conduct and the managerial duties.
Physician managers have to become accustomed to the notion that they must account for others actions in addition to theirs. The physicians take up many roles depending on hospitals or departments. Most of them take up managerial roles where overseeing the activities of their junior staff is part of their mandate. Staff roles that involve formulation of policies and collateral role that ensures collaboration between two persons are also favourites for the physicians. They are also absorbed as monitors and representatives whereby they represent the interests of a particular group. Other roles may include secondment for a short duration and coordination of certain group of people (Leatt, 1994, p.172-173). Involvement in one or more of the above roles may have strain on the performance of the professionals although it opens other career advancement avenues.
The issue of clinicians taking up employment will only become a policy issue when the government exerts undue pressure on the health care system aimed at minimisation of costs. The medical fraternity realised that their existence is challenged hence should involve themselves in policy formulation at all levels of governance. At this point, the physicians feel compelled to intervene as part of wider efforts of fostering participation in the governance. Leatt asserted that the physicians need to acquaint themselves with the policy and largely the political processes that give birth to the policies (1994, p.174-175). This is imperative in the understanding the implications of funding to the clinical practice and health care system. The need to focus on client oriented programs and decisions informed by evidence-based practice are crucial in the achievement of the intended policy changes. The understanding of strategic building and quality improvement particularly in the healthcare systems are among areas that need close attention by the physicians. Initiation and development of performance improvement plans in the organisation is imperative in the achievement of the quality improvement (Leatt, 1994, p.174-175).
Following the changes in the management in the recent past, what remains to be seen is the tenability of the paradigm shift. Considering the practice is gaining root in many healthcare organisations, it will not be long before notable changes occur especially regarding the quality of patient care and the improvement in the financial outlook of the organisations.
Research aims and objectives
- To identify the factors that influences the clinicians’ engagement in the health care management.
- To identify the various roles embraced by the clinicians after joining the health care institutions as managers, and the barriers and challenges they encounter.
- To explain the factors that lead the physicians to switch to managerial duties and the role played by professional bureaucracy in perpetuating the switch.
- To describe the impacts to healthcare in terms of policy brought about by clinicians embracing management.
Specific research questions
The main aim of this study is to analyse the extent to which clinicians engage in health care management. To explore the above aims, a number of research questions were developed.
- What is the meaning of management and how does it differ in the context of health care?
- How does professional bureaucracy in health care impact on physicians and other health care workers taking up managerial duties?
- What are the main predisposing factors that make clinicians to take up managerial duties?
- What are the major roles taken by the physician managers in the health care organisations?
- What policy measures put in place or are needed to safeguard the interests of all stakeholders affected by the switch?
Significance of the study
The study will focus on deducing the factors that influence the clinicians to engage in the health care management. The study in particular will be interested in addressing the knowledge and research gap between the reasons behind the engagement of clinicians in managerial duties particularly in the United Kingdom. The study will also look into the various roles embraced by the clinicians after joining the health care institutions as managers. More importantly, the study will try to explain the factors that lead the physicians to switch to managerial duties and in particular look into depth, the role played by professional bureaucracy in perpetuating the switch. Outlining and discussion of the resultant implications due to this switch will occur in order to get the real impact on the professionals and the health care organisations. The factors that influence the formulation of policies aimed at managing the engagement of clinicians in management will receive considerable attention. The policies in place or needed will also be discussed in depth.
Who is this study of interest?
As concerted efforts get underway to integrate health professionals in management aspects and as issues related to roles embraced by clinicians on assuming health management duties, achievement of quality care to patients will get immense attention. As more questions surface about what motivates clinicians into taking up management positions in health care providing organizations, at the receiving end will be the patients who will be enjoying better service delivery.
Organisation of the study
The organisation of the study will be as follows;
- Chapter one: this chapter will mainly discuss the introduction and the research methodology. The introduction will include the context, background and the statement of the problem in relation to the study topic. Research questions and the significance of the study will be part of this chapter. The organisation of the study and the time frame will be described.
- Chapter 2: chapter two will discuss the management literature review with emphasis on health care organisations.
- Chapter 3: the management context will form part of this chapter
- Chapter 4: epistemology and methods will be described in depth in this chapter.
- Chapter 5: chapter five will shed light on the findings from the literature review of previous studies conducted on NHS in United Kingdom.
- Chapter 6: the chapter will mainly delve on the discussion. The discussion of the results in relation to the management context will be achieved here.
- Chapter 7: the chapter will describe the conclusions and recommendations made based on the discussion of the findings. The chapter will also suggest areas of future works
Literature Review
Introduction
This chapter will present a literature of the functioning of the clinicians in the health systems across the globe with specific interest in barriers they face in executing their responsibilities. In tandem with their functions, the chapter will present an in-depth review of the professional bureaucracy with regard to the changes and implication of policies in the health systems. Taking into consideration the involvement of non-clinicians in managerial capacities, the chapter will shed light on the potential inter-professional and role conflict experienced by the health workers. More importantly, presentation of the theoretical frameworks applied in carrying this study will occur in relation with the management context of the National Health Service in the United Kingdom.
Health care management
Since 1980, nursing, medical, combined with the allied health workers have continually responded to the ever increasing and changing complexity in clinical practice and to a larger extent, the organisational designs through restructuring into a wide range of domains. The three ranges of domains include management practice, clinical practice, and research and education. Of particular importance has been the formalisation and institutionalisation of managerial roles thereby eliciting intense debate. Over the last few decades, there have been tremendous changes in the management of health care organisations occasioned by various policy and economic changes in the world (Walshe & Rundall, 2001, p. 429). It has become common for healthcare professionals to utilise the available scientific evidence in deciding the policy or management changes to undertake in the organisations. According to Sackett and Rosenberg (1995, p. 32), the concept underlying evidence based healthcare has become an integral component to every clinician, manager, and policy makers in the management of healthcare services all over the world. The involvement of clinicians in healthcare management is due to the urgent need to encompass evidence based healthcare and clinical practice in the overall development of strategic and organisational development plans.
According to Davis and Nutley (1999, p. 2), the clinician management concept has provided the best remedy to the ever increasing problems and challenges affecting the delivery of effective healthcare services. That notwithstanding, the changeover to clinician management has offered many challenges and drawbacks and these threatens to compromise the cordial relations between the professional and management roles of the clinicians. Furthermore, an increasing propensity of conflicts between the clinicians and non-clinicians has occurred thereby curtailing organisational performance of many healthcare institutions. It is worth noting that this paradigm shift has resulted in better management of resources and enhanced provision of quality care in the long term. In tandem with the trends in management, organisations have taken different approaches when it comes to healthcare management with varying levels of success and failures. In majority of the civilised societies, health sector has become very dynamic thereby suggesting the need for continuous and long term learning for the managers and providers of healthcare services. Walshe and Rundall (2001, p. 430) stressed that monumental task in management is needed in ensuring efficiency and effectiveness in the delivery of quality patient care and organisational development. More importantly, translation of theory into practice has ensured that the leadership receive important skills that will lead to better healthcare management.
In line with realignment of managerial roles in healthcare, several European countries embarked on reformist agenda (Neogy & Kirkpatrick, 2009, p.1). Duffield (1992, p.48) asserts that the key components of management include managing relationships, management tools and organisational processes in healthcare. Across European health systems, management of relationships entailing interactions with the customers and stakeholders, collaboration with other organisations and strategic management has received due attention in the last few years. Moreover, Neogy & Kirkpatrick (2009, p. 71) asserted that healthcare managers have continually utilised important tools such as healthcare finance, economics, information systems, marketing and total quality management in order to achieve superb results in their work in the health systems (Duffield 1992, p. 497).
Varying degree of involvement for clinicians in strategic management has been experienced in European countries (Neogy & Kirkpatrick, 2009, p.1). Strategic management in healthcare organisations is imperative in ensuring the organisation is well aligned to meet the expectations and demands of the external environment. In line with this, strategic management requires the development of appropriate relationships particularly with the customers, competitors and other organisations and relevant government regulators.
Strategic management process helps in the integration of theory into practice, thereby offering avenues for the accomplishment of the set goals and objectives. Floyd and Wooldridge concept provides the greatest linkage in the contribution done by middle management in influencing strategic decisions (Floyd & Wooldridge, 1992, 1997, 2000). In essence, it partly provides a basis unto which the external environment influences the management with regard to expectations and demands of the outside world (Dent et al, 2003, p. 357). Realignment of the organisation internal environment, capabilities, competencies and largely its resources in line with the concept largely determines the achievements of the organisation. A balance between the external and internal environment is inevitable as stressed by Walshe and Rundall (2001, p. 430). In relation to the theory, strategic management in health systems require the determination of the aspirations of the organisation, its leadership and more importantly its employees. To achieve successful formulation and implementation of organisational strategies, it is overly imperative to strike the correct balance between the factors of management
In addition to the organisational internal environment, middle management has become the major area where clinician managers have influenced development in healthcare institutions. Although minimal research has occurred in the field of middle management, the contribution to strategy development has been recognised and appreciated by stakeholders in the sector. With regard to health systems, a middle manager has come to refer to the person who reports to the chief executive office of the entity or organisation for that matter (Floyd & Wooldridge 1992, p. 45). Involvement of middle level managers in the eventual strategy development provides the much needed stimulus to strategic thinking in business entities and not-for profit organisations. Middle managers have continually faced the brunt of downsizing undertaken in many organisations due to embracement of cost containment and free market policy in 1980 and 1990 (Scarborough & Burrell 1996, p. 12). Criticism on the part of middle managers as impediments to change has occurred. Nevertheless, their managerial roles have continually changed with time with much delegation happening (Dopson &Neumann, 1998).
Much literature has concentrated on the role of managers while ignoring the contributors and the drivers to the fulfilment of these roles. Despite being a key pillar in the implementation of policy in healthcare organisation, little research has delved on their role and the main hindrances in achieving these roles. Managers’ involvement in strategy development has provided the much-needed clinical expertise in the organisational development. Organisational performance is usually pegged on the contribution and the influences of what takes place in the middle of the healthcare organisation. Consideration of the contributors and drivers in change in relation to the effectiveness of the strategies in the hospitals and health systems has overly received minimal attention from researchers, although managers act as agents of change and strategic actors. To understand the roles of middle management, Floyd and Wooldridge (1997) developed a typology in strategy development. Despite its setting in a turbulent business climate with ever-changing expectations especially with regard to the responsibilities of middle managers in running the organisation, the typology has provided guidance to middle clinician managers in executing their responsibilities. The scenario consists of two distinct phases. The first phase started in early twentieth century up to the start of the 1980’s and came to be referred to as the golden age since the middle managers were vibrant and their numbers soared. The elaboration of the hierarchy was achieved in Europe and the United States. Global competition ensued from the 1980’s thereby ushering the second phase (Frohman & Johnson, 1993, p. 87).
Frohman and Johnson (1993, p. 90) asserts that a more complex and new competition reality took place buoyed by the forces of deregulation and pressures from internal pressure. Delayering of middle managers has since become a norm due to the belief by the top executives’ that the responsibilities undertaken by them are merely implementation processes. Moreover, cost reduction and the desire to achieve improved organisational performance expected from the delayering has not been witnessed in many of the cases. Several organisations including the National Health Service and service providers in the American health system embarked on downsizing of their workforce through implementation of policy changes meant to lower running costs (Ferlie et al 1996, p. 98). Although they have gained leeway in ensuring cost effectiveness, the health systems have continually suffered from poor strategy development that in essence has led to poor quality in patient care services.
Middle managers, who are mainly clinicians, serve as intermediaries of change in the healthcare organisations (Balogun, 2003, p. 69). Clinicians’ contribution during the change process provides the expertise and impetus required for success in the health care institutions. Managers tend to fulfil several intertwined roles during the change implementation process- “undertaking personal change, helping others through change, implementing necessary changes in their departments and keeping the business going” (Balogun, 2003, p. 70). The middle managers, nurses and doctors, roles have been studied from a wide array of perspectives, with staff, organisational and relation to co-workers receiving immense attention (Duffield, 1992). Moreover, patients and their immediate relatives are indirectly required to rate the functioning of the managers while assessing the overall quality of their work (Frohman & Johnson, 1993, p. 87). In addition, the managerial roles have been studied in relation to the job satisfaction, work environment, stress and the overall influence on strategic changes and realignment of power structures in the organisation. Nonetheless, the roles of clinicians remain largely unclear owing to the fact that the topic is largely understudied.
The role played by managers in interpreting the change intent is large thereby guiding their actions and influencing the overall implementation outcomes. Middle managers serve as a crucial link between the top executives and first line management health organisations thereby ensuring provision information upwards while consuming strategic decisions (Ferlie et al 1996, p. 98). Middle managers are hence the pillars and agents pivotal in the implementation of strategic decisions particularly when touching on core areas of health systems such as patient care (Floyd & Wooldridge 1997, p. 466). However, failure and inefficiency in the part of managers make them act as blockage of change especially when they act to curtail the smooth flow of information (Dopson & Neumann, 1998, p. 67).In studying the roles of clinician managers, different theoretical frameworks received application depending on health cares system. Leaderships approaches such as total quality management (TQM), balanced score card and the commonly utilised management by objectives (MBO) has received wide application. While each approach has received application, minimal studies have occurred in comparing their efficacy and effectiveness in different managerial setting (Surakka, 2008).
Middle managers act as strategic asset for the restructuring program in the organisation through offering diligent and loyalty to the organisation (1992, p. 12). Contradicting findings on the role of managers as assets in strategic development has been provided through empirical research. Although there are optimistic and pessimistic views on the middle managers service as strategic asset, the direction they take depends largely on motivational initiatives and the workload pressures in the organisation. More than two thirds of the organisations in Britain had indeed restructured while more than 50 % of managers interviewed decried increasing workload and more responsibilities in the workplace ((Martin, 1992). Successful restructuring must take into account the roles carried out by the middle managers.
Understanding of organisational culture has become a key requirement for middle managers serving in health care organisations. Involvement of the middle managers in strategic development is crucial if a clear understanding of the impact of the organisational culture is to be achieved. While previous studies had denoted that strategically involving the middle managers in for profits has yielded positive benefits in terms of shaping organisational culture, scanty evidence on its impact on not for profit organisations has been observed (Martin, 1992, 245). In contrast, studies carried out in hospitals across Europe and America has indicated there are several benefits of integrating strategic skills in middle management.
Strategy management roles are integral for middle managers in order for them to actively lead the organisations in achieving their set goals. Considering the divergent theoretical frameworks applied in studying managerial roles by clinicians, it becomes clear that clinician management is dynamic and prone to policy changes in the healthcare structure. The role in developing and sustaining organisational culture is imperative for creation of a solid foundation where improvements on quality and cost effectiveness can be achieved. The paradigm shift to clinician management has occasioned the need for clinicians to acquire basic financial skills that are useful in the management of funds in the health system. Duffield asserted that managers needed to have working knowledge of some basic tools at their disposal in order to develop and maintain an effective and overly efficient organisation (1992, p. 50).
Considering the extent of budgetary allocation for healthcare services in western societies, competence in healthcare finance has become an integral component useful in guiding management particularly when engaging in expenditure and collaboration deals with other organisations. Likewise, financial statements in the United States are important in the determination of the feasibility and attractiveness of healthcare alliances, mergers and the success expected from certain strategic decisions (Broyles & Falcone, 2005, p. 34). Continued relations with insurance companies, managed care organisations and other service providers are usually pegged on the performance and attractiveness of financial statements. the knowledge and the application of the systems combined with the working knowledge of the clinical databases has enabled the US healthcare system better placed to embark on positive strategies that keeps in mind the values of the organisations and patients rights.
Knowledge of the administrative and financial systems combined with the strategic decision support systems is instrumental in aiding the top brass management in coming up with competitive and long term strategies especially in the health insurance and private health sectors. Studies on administrative roles of nurses and doctors based on leadership approaches has denoted the importance of financial literacy particularly in the face of financial deals between worth millions of dollars within the sector. In contrast, inadequacy in funding to health sectors in parts of Europe, Asia and Africa has curtailed the achievement of this goal.
Communication is pivotal in the achievement of quality management in the healthcare institutions. Vastola and Tosoloni (2005, p.223) noted that the importance of quality management has forced the stakeholders including the clinician managers to integrate quality in the strategy development by ensuring resource leveraging. It is worth noting that the clinical managers have the mandate to link quality management into organisational learning and quality improvement process in order to enhance its sustainability. In fact, Mintzberg theory of managerial roles has depicted communication and liaison roles as imperative for any managerial position (Mintzberg, 1973, 1974).
More importantly, the role played by integrated systems particularly in the last decade will influence the delivery of healthcare services in the coming few years (Blair a & Fottler, 2002, p. 54). Of particular importance is the dynamic nature observed in the stakeholders thereby requiring the development of solid systems that will aid in their management. It is worth noting that the customers form the bulk of the stakeholders thereby making it vital to laying down of strategies that will ultimately lead to the effective management. Furthermore, increasing competition among the providers ultimately result in the better service delivery for patients (Duncan et al, 1998, p.1-3) while development of strategic alliances with several other hospitals will enhance the overall delivery of patient care (Neogy & Kirkpatrick, 2009, p.1).
Quality and professional empowerment represent crucial tools that enhance the development and actualisation of human resources (Vastola & Tosolini, 2005, p. 233). Contribution of better and improved technical expertise especially when the development and eventual implementation of the training is combined with quality improvement should be prioritised. Active involvement of physicians in the top management showed significant positive relationships particularly when working hand in hand with other stakeholders such as board and managers (Weiner, Shortell & Alexander, 1997, p. 506).
Impediments in clinician management
Intense debate has continued to rock the clinician manager roles. In the recent past, debate has revolved on the merits of the quality and the applicability of evidence based practice in turning around the practice domain from the simplistic to a more complex and professional one. Failure to utilize evidence based practice in the strategic and organizational management has prevented many professionals from embracing management roles in European health systems. Furthermore, Walshe and Rundall (2001, p. 65) has noted that there are efforts to recommend a standardised body of concepts, skills and knowledge before one qualifies as a clinician manager.
Although much has happened in terms of reforming the perception of clinician managers, they continue to execute their responsibilities in organizational structures that have limited career advancement to offer. Anderson & McDaniel (1993, p. 56) asserted that structural barriers such as insufficient power and authority has been identified as the major impediments in the effective execution of boundary spanning roles in the United Kingdom and USA. Many a time would a clinician find himself at the top senior level of administration, but fail to clinch the top executive roles due to a constellation of limiting factors. Scherer (1999, p. 87) noted discrepancies in the easiness of attaining executive roles with physicians more likely to act as equal members of the top management level than nurses and other health professionals. Nurse Directors were faced with several impediments that prevented them from attaining the positions of chief executive officers, according to a large scale survey conducted in England.
Previous studies have asserted that the benefits accrued from clinician managers are enormous. The healthcare professionals have remained reluctant to embrace and value managerial roles as a noble and legitimate activity that has the ability to offer satisfaction just like the clinical practice (Ham, 2003, p. 4). The embracement of the managerial jobs usually comes with their own practical and sometimes conceptual barriers. Professional identity is the most prevalent conceptual barrier in the execution of the hybrid practice roles (Braithwaite & White 2003, p. 78). In line with this confusion, mixed empirical findings have reported that the hybrid manager losing professional identity or credibility by the act of deserting the professional practice. Moreover, branding of clinicians as people who lack business acumen by the fellow colleagues from other field is common who act as general managers. Organizational structuring witnessed in the last two decades has eroded the cordial relationships between the management and professional to a point of sheer antagonism thereby leaving the hybrid managers in a dilemma on which side to lean to (Davies, Hodges & Rundall, 2003).
In addition, the practical issues such as the need for educational preparation overly dissuade majority of the individuals who are motivated and ready to venture into the hybrid management roles. This has forced the educators to start integrating the equivalent of management practice into the curricula of the specific health professions thus improving the capabilities of the trainees. A wide range of educational opportunities and programmes are available to bolster the effectiveness of the management practice in the clinician managers. Majority of the successful organisations are keen to harness the best talent among their human resources. In the case of hospitals, majority of the highly talented and skilful are mainly professional working in the functional areas of the provision of services. The propensity of the dual hierarchy finding application in healthcare has meant alienation of the groups from institutional management. It is therefore worth noting that the success of hospital operations is reliant on the proper incorporation of professional expertise and the overall management structure (Surgeon 2003, p. 35).
The intersectional integration of professionalism and complexity forms a new source of better insights that are imperative in improving the outlook of the healthcare industry either from both the business and the clinical practice point of view. The limitations offered by the organisational change are responsible for difficulties in the implementation of policies. Organisational change should be directed towards ensuring the achievement of professional bureaucracy. Taking into account that professionals are independent in their functioning, replacing their work is an insurmountable task. Implementation of change in the healthcare requires the replacement of the existing staff with people that are very sympathetic particularly to the change process. More importantly, the leadership come in handy during the organisation for change during the crisis situations while other strategies come second after these requirements (Anderson & McDaniel 2000, p. 82; Surgeon 2003, p. 35).
Conflict in the clinician-managerial roles
Health professionals and managers have embraced changes of policy in healthcare systems all over the world. The turbulence in the functioning of the healthcare system has burdened cadres such as nurses and physicians with extra responsibility of management and accountability in the healthcare setting (Everson-Bates 1992, p. 17). Furthermore, changes in the demographic compositions of the patients and clinicians have occasioned the difficulties in role interpretations while modifying patterns of response (Duffield 1992, p. 49). This has brought into fore the need for a systematic managerial infrastructure intended to offer support with the first line managers in nursing and medicine. In line with this, the fist line managers must be equipped with the required skills, knowledge to ensure that patient care is enhanced, and staff motivated. The first line managers work in tandem with the middle level and the senior managers. Since the higher managerial positions are filled through well-orchestrated promotion framework, any changes in the competencies and attitudes in any level of management may have far-reaching implications on the system thereby influencing its direction and eventual effectiveness (Duffield & Franks 2001, p. 88).
Despite the fact that managers have the mandate to oversee, the operations of business entities, nurse managers are ill prepared to run the business operations as compared to their normal clinical activities. The managers’ and the executives’ perceptions on the required competencies and roles remained dismally poor. Managers and the executives were in total agreement on the issue of required competencies, although the nurses’ managers did not clearly understand the responsibilities of the executives (Kleinman, 2003, p. 454). While the executives placed more emphasis on the acquisition of a second degree in improving performance for the managers, it was not really appreciated by the nurses.
Recent structural and organisational changes have increasingly shifted the nurses from their common work positions thereby placing more burdens on them (Kleinman, 2003, p.4 34). While majority work as first line managers, others have occupied senior and executive positions such as human resource managers, policy analysts. The few who are occupying the executive positions find themselves mandated to address the professional needs in areas of public relations, ethnic affairs and information and technology. Mintzberg (1994, p. 37) asserted that the first line managers role involves the blending of care whereby managerial responsibilities have to be mixed with patient care.
Although much has been reported on the evolving role surrounding their work, scanty evidence exist on the exact roles of the first line managers (Sanders et al 1996, p.23). The lack of consensus on the exact roles has largely been blamed on the significant differences evident in the individual healthcare systems. The overly reliance on the setting and the organisational structure that the nurse is exposed before deciding on the scope of their roles has complicated the analysis thereby making the available data to remain unreliable (Wilmot 1998, p. 45). However, in their execution of these responsibilities the first line managers usually encounter enormous challenges occasioned by the aggressiveness and volatility in the marketplace.
Despite enormous studies dealing with staff empowerment, scant evidence exists on the part of nurses’ managers. Stark differences were observed in the nurse managers perceptions of power depending on their level (Goddard & Laschinger, 1997 p. 132). Middle level managers reported higher tendencies of having greater access to power as compared to the lower first line managers. Despite middle level managers reporting higher access to empowerments opportunities, they failed to achieve empowerment owing to management constraints just like the first line managers. Inaccessibility to factors that are important to support the empowerment process makes managers less effective in their job performance. Moreover, there exist a link between the structural empowerment and effectiveness in leadership role (Upenieks 2003, p. 54). Middle level and senior managers who had a positive response towards provision of access of information, support and resources are in a better position to respond that their work was highly valued by their employers. The perceptions of nurse managers towards empowerment were overly related to efficiency in terms of competencies achieved in the various leadership positions (Laschinger & Shamian, 1994, p. 23).
Further research also noted that managers’ ability to jumpstart activities in the organisation was inherently related to the perceptions of the staff nurse on their empowerment (Kanter, 1993, p. 35). Powerful managers have the propensity of empowering their employees by way of their association. However, limitations in terms of accessibility of funding and the lack of equal footing at policymaking level continue to be the major hindrances towards achieving adequate capacity to respond to or initiation of change in nurse executives. It therefore becomes important for the management to provide clinician managers with the supportive organisational conditions needed to achieve managerial performance particularly in nursing practice. Moreover, non clinician managers and administrators have always had the propensity of taking long to understand the unique skills and expertise brought to the table by the clinicians. Clash and lack of understanding of each other has precluded and curtailed working relationship between non-physicians and physicians (Schneller, 1991, p.23). In light of this misunderstanding, healthcare organisations faced with dwindling margins must ensure they involve the administration and board of directors in order to come up with strong structures.
Professional bureaucracy
The success of any organisation and business is pegged on its performance and the quality of services offered to its customers or clients. In line with this, mixed success and failures has been witnessed in Europe owing to the reform path they have taken. In addition, clinical autonomy has been regarded as a core concept that influences the overall outcome of health system (Harrison & Doswell, 2002, p. 208). However, professional autonomy is faced with tremendous challenges in the majority of the western countries. That the clinicians are overly managed by other people means that the propensity of receiving unfair treatment is likely to occur (Eltson, 1991). The clinicians are therefore eager to have the power to determine their own destiny in terms of the clinical practices and ability to assess their own performance without having to report or account to non-clinician managers (Harrison & Doswell,2002, p. 208).
Majority of the European health systems has continuously utilised two phases of management. Likewise, the NHS and the German health system have endeavoured to improve their systems by introducing policy changes aimed at improving the efficiency and cost effectiveness of the systems emerged (Neogy & Kirkpatrick, 2009, p. 14). The two lines of management, characteristic of the NHS, have a top management structures that is political and hierarchical in its approach. According to Harrison & Doswell (2002, p. 216), the coexistence usually generates to acrimony and tension fuelled by their differences in objectives and goals. Whilst the managers’ survival is entirely pegged on the effectiveness in meeting the projected targets, the professionals are overly involved in peer review mechanisms aimed at consolidating and furthering their profession (Fitzgerald & Ferlie 2006 p. 65).
The embracement of the clinician management took effect after the traditional bureaucratic approach experienced various challenges that almost led to the total collapse of health systems in other countries. Studies have shown that clinicians who undertake management training exhibit high competency and bring unique leadership in the health systems. Furthermore, the clinicians have the intimate knowledge of the functioning of the health systems hence their views are generally acceptable by all the concerned stakeholders. More importantly, other studies have denoted that clinicians are better placed to lead health systems into efficiency through their adoption and embracement of high risk strategies and technology that is in line with advancements in medical field (Harrison & Doswell, 2002, p. 216),
In line with the reforms aimed at involving the clinicians in healthcare management several forms of bureaucracies have been entrenched in different health systems in parts of the world (Neogy & Kirkpatrick, 2009, p. 14). Although the hybrid structures enjoy massive application, disparities in their performance have occurred particularly with regard to relations with the administration. Hoff noted that there are professionally compatible who inherently adopts custodial relations in contrast with the organisational compatible who are overly interested in the managerial responsibilities. Davies et al noted that whilst convergence between the clinician and non-clinicians in the junior management levels has been witnessed, little can be said about the directorate positions.
In Denmark, the prerogative of leading the unitary form of bureaucracy is usually vested on the leading consultant in the hospital while junior members of the profession are overly interested in clinical and professional matters at the expense of organisational performance. In contrast, the Italian health system has adopted a clear directorate structure through legislation although very few doctors accepted to take up managerial roles (Lega, 2008, p. 56). Despite this setback, doctors and health workers receive wider consultations particularly during the development of hospitals and welfare improvement unlike in Netherlands.
While majority of the institutions retain the traditional approach and contractual arrangements, others have entirely joined the management ranks (Plochg, 2006, p. 37). While the latter has similarities with the decentralised system in Germany, clinicians have become influential in Germany health system thereby undermining the medical profession through their wider involvement in budgetary and administrative issues (Nowak 2006, p. 1522). Introduction of policy measures governing the management and clinician engagement has received luke-warm reception from the doctors who are at odds in participating in managerial duties due to lack of adequate managerial training.
In view of the forms of bureaucracies, dissatisfaction was highly reported between the doctors and the managers although the level of dissatisfaction was lowest as you go up the hierarchy. Clinician managers reported positive relationships with colleagues in the same level of administration although the other staffs were less positive. The frosty relations between the doctors and staff on one hand and the directors and other managers on the other are fuelled by the incessant supervisory roles vested on the non-clinicians (Neogy & Kirkpatrick, 2009, p. 14)..
Conceptual frameworks
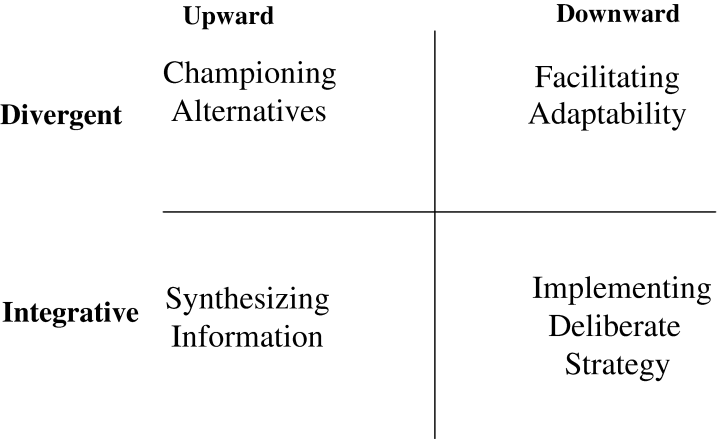
The studies on management roles of clinicians relied on several theoretical frameworks informed by the variables under assessment. In view of this, the theory of managerial roles and the Floyd and Wooldridge theory of strategic management were applied in several studies (Currie & Procter 2005; Carney, 2004). Floyd and Wooldridge typology of strategy development in middle management has broadened its application into the influence wielded by stakeholders in the management particularly at the middle level. Taking into account that majority of middle level managers are clinicians, Floyd and Wooldridge (1992, 1994 &1997) embraces the strategic roles of the middle managers in addition to thinking. In their theoretical framework, two dimensions are presented. The first dimension looks into the direction of influence the middle managers exerts on the strategy development in the organisation. Secondly, the second dimensions are concerned with the extent the influence of the managers alters or realigns the concept of strategy in the organisation. In view of the two dimensions, four types of managerial roles are formed.
First, the managers synthesize information thereby interpreting it before channelling it upwards for consideration by the executive management. In doing so, the executive management may accept to utilise the information as an important basis to make decisions on the utilisation of resources in the long term. Under championing alternatives, development of potential alternatives to the normal strategies in a bid to offer better solutions to the organisation occurs. Thirdly, involvement of middle managers in bringing transformation, by exerting changes under their dockets, in a process referred to as facilitating adaptability.
Fourthly, under implementing deliberate strategy, is instrumental in the overall organisational performance. The alignment of the organisation action to ensure it becomes in tandem with the strategic aims and goals championed by the top brass management. Middle managers come in handy during policy implementation thereby ensuring that the corporate strategies are well replicated in workable action plans. In line with this, uniformity must be carried out in order to ensure that that consistency in performance is exhibited at the operating levels. The clinician managers’ role in maintaining consistency in delivery of services is paramount to avoid breakdown in the coordination of the vital elements involved in strategic management.
Taking into consideration the various roles of the middle managers, this study will apply the theoretical frameworks in trying to discuss the levels of involvement of clinicians in management particularly in strategy development. Owing to its wide application in studies assessing the managerial roles of clinicians in healthcare systems, Mintzberg theory of managerial working roles was preferred for this study. After the selection of the relevant studies using systematic and realism reviews. It was found essential to analyse the information as carried out in earlier studies (Baxter, 1993 & Skytt et al, 2006).
Mintzberg (1973, p.54) espouses that a role is ‘’any organised set of behaviours belonging to an identifiable office or position’’. Since its innovation, the theory has been reliant on 10 roles that are common to the managers. In a nutshell, the roles were put into 3 categories for ease of understanding; interpersonal roles that depict the authority and status of the manager, decisional roles that assert the authority of the manager particularly in utilisation of information; and informational roles that relate access to information in relation to the interpersonal roles.
There lacks enough literature that clearly defines the managerial roles for clinicians across the levels of management particularly with regard to the middle managers, where majority of the clinicians influencing strategic change fall. With regard to this confusion, literature has depicted heightened tension on the degree non-clinicians should cede responsibilities traditionally vested on them (Currie, 1999; Storey, 1992). While management literature regards middle managers as pivotal in implementing strategy, other studies have depicted them as barriers to change (Wheatley, 1992 & Storey 1992). The success of the organisation is inherently dependent on the level of involvement of middle managers in making decisions.
Mintzberg (1973) purposely groups managerial responsibilities and roles as:
Table 1: Mintzberg: The Managerial Roles (Adapted from Mintzberg, H., 1973, The Nature of managerial work. New York: Harper and Row).
Management context
Introduction
Healthcare has become dynamic in nature owing to its influence from political and policy changes in various governments around the world. Taking into account the onset and development, a contextual basis of the management will be discussed at length. An in-depth analysis of the British National Health Service will be presented in this chapter. Taking into account the objectives of this study, it becomes imperative to discuss the bureaucracy, functionality of the managers and the barriers or conflict they face on a daily basis when executing their managerial responsibilities. In tandem with the changes experienced in the health systems around the world in the last three decades, this chapter will describe the policy changes and implications to the strategic and operational management of the National Health Service.
Contextual basis of the clinician-managerial roles
In the healthcare field, the role of the clinician manager is mainly advocated for by means of bridging the wide gap evident between professional hierarchies on the one hand and managerial hierarchies on the other. In view of this underlying difference, the boundary-spanning roles are usually undertaken with the sole aim of checking the views and interests of the various stakeholders and ensuring they are aligned to overall goals and objectives propagated by the organisation.
Clinician managers ought to act as the advocate and defender of their colleagues in the profession while also ensuring that they translate the goals and objectives of the organization to the junior and fellow clinicians with a view of instilling the discipline that is vital to ensure organisation success. Striking the balance between the two demanding and contradictory roles has always become a tricky part of the career of clinicians in Europe. Research shows that those clinician managers who overly achieve the balance are at a greater chance of succeeding in their position and vice versa (Neogy & Kirkpatrick, 2009, p.1).
Previous studies in a majority of the developed countries in Europe on the formal roles of clinicians in management have produced findings with wide disparities. Varying degree of involvement and differing roles have also emerged (Neogy & Kirkpatrick, 2009, p.1). Denmark is by far the most progressive country, with doctors here having increased autonomy and accountability in the healthcare management in addition to a systematic management training programme usually designed to cover healthcare workers. Danish authorities have prioritized instilling leadership and communication skills in the clinicians from the time they undertake training as a preparatory measure for them to join management in the institutions.
On the other hand, studies done in the UK depict a bad picture where conflict and antagonism especially between the clinicians and the non clinical managers has escalated in the recent pas, thereby causing stakeholders to embark on a reformist agenda. In line with this, tremendous progress in terms of an integration of the management r, coupled with their definition of boundaries of roles has occurred with more far reaching reforms expected in the NHS. The French and the German healthcare systems have not effectively integrated the concept of training in their institutions of higher learning. However, taking into account the goodwill exhibited by the stakeholders, their systems has made tremendous steps toward integration of clinicians in management roles within a short period (Eeckloo, Delesie & Vleugels, 2007, p. 68).
On the degree of involvement of healthcare teams in management, disparities have existed owing partly due to the difference in the management concepts. In contrast with the UK, French healthcare system embraced the clinician management concept later but has effectively embedded it in its well managed healthcare system (Eeckloo, Delesie & Vleugels, 2007, p. 67). In Germany, the situation has received mixed reactions, with several large institutions embracing the concept while others retaining the traditional approach. However, Germany tends to involve its healthcare teams in strategic management with several positions reserved for doctors in the strategic and executive boards (Dent et al, 2003, p. 356; Fattore, 1999, p. 56).).
On the other hand, Netherlands seems to share similarities with the German counterparts in terms of embracing the dual concept of managerialism. Whilst most large hospitals in Netherlands have doctors at the top management level, lesser numbers of health systems retain the earlier approach where managers are hired on a contractual basis with high autonomy over the doctors (Fattore, 1999, p. 56). The adoption of the clinician management is encouraging in European health systems and is expected to improve the strategic management and organizational performance.
Management context of the British National Health Service
The British National Health Service (NHS) came into effect in 1948 through an act of parliament and was mandated by the government to provide healthcare services to all the British citizens in England, Scotland, Northern Ireland and Wales. The services are available to the more than 60 million people in the United Kingdom regardless of their ability to foot the charges for the services. The overall mission of the NHS is to safeguard while promoting the mental and physical health at the optimum levels for all UK citizens through holistic approach that entails prevention of ill health, timely and accurate diagnosis and treatment and long term rehabilitative of the disabled and the chronically ill. Taking into account that the NHS is 100 % funded by public funds, its management is supervised by the department of health through 8 regional management boards and is entirely required to be accountable to parliament. Moreover, the NHS is the primary organ that is mandated by the government to set, implement and evaluate policies relating to all public health issues in the UK (NHS England, 2009, para. 1-4).
Nearly 1.7 million people are employed directly or indirectly while the annual budget is estimated at about 100 billion with the bulk of it going into paying the salaries and procuring medical supplies. With more than 120, 000 qualified doctors and more than 410, 000 nurses, NHS has developed several strategies aimed at inducting them in management of t wide range of services. An estimated 700, 000 are believed to visit the NHS facilities to access medical services weekly (NHS England, 2009, para. 3). The colossal amounts channelled to the National Health Service have elicited debate on the need for health policy reforms aimed at introducing end-user payment services.
The NHS is under the supervision of the Department of Health, whose stewardship is bestowed on the secretary of state in charge of health affairs. The Department of health has overall responsibility in the control and management of the 10 strategic health authorities (SHAs). In addition, the SHAs are mandated to oversee the activities of the NHS trusts operating within their jurisdiction. The performance of the NHS has not been systematically reviewed but figures denoting the health of the population denote a decrease in the mortalities while a significant increase in the life expectancy has been witnessed (NHS England 2009, para. 5).
The paradigm shift to the patient centred approach has brought tremendous improvements on the quality of care services. On management platform, far reaching reforms introduced in the last 20 years has improved efficiency. However, efficiency on financial and administrative matters has not achieved much improvement owing to the complexity and the enormity of tasks required of the NHS. In line with this, the NHS is usually faced with deficits owing to the failure of the various organs to adhere to the laid down guidelines on resource allocations. Of particular importance, is the introduction of clinician managers in the management structure of the health systems (NHS England, 2009, para. 5). Clinician managers are crucial to successful implementation of the organisation goal because of their propensity to have wide knowledge of the health activities.
In late 2002, the government created 28 strategic health authorities (SHAs) with the main aim of managing the NHS at the local level thereby acting as a linkage with the Department of Health (Royal College of General Practitioners 2004, p. 1). Majority of the roles carried out by the SHAs entail supporting in the integration of national priorities in delivery plans formulated by the local health units while assisting in improving overall performance and providing necessary guidance especially in resolving conflicts in the health systems (Royal College of General Practitioners 2004, p. 1). The authorities and trusts are mandated to run all health systems in the UK. Under the authorities falls more than 300 primary care trusts (PCT) that are mainly mandated to plan and improve the functioning of the community health services and the delivery of primary care services to the citizens.
Acute trusts ensure that the hospitals run smoothly and healthcare provided is of high-quality while planning and implementing development programs in the core areas. Majority of the clinicians by the acute trusts thereby may end up taking up jobs as managers in the hospitals. While the ambulance trusts provide emergency services with care and mental trusts offering social care and mental health respectively. In addition, the foundation trusts are health entities that are managed by a management unit that comprises a wider range of professionals. The local managers who are assisted by clinicians and members of the public mainly execute the running of its holistic activities.
The decentralized units help the community and the public to choose the best approach to the provision of healthcare in their areas countries (Neogy & Kirkpatrick,2009, p. 34). The incorporation of the different cadres of personalities from different fields has provided the foundation trusts with the necessary expertise in improving its performance. Since their inception in 2004, the foundation trusts have enjoyed considerable autonomy and accountability in terms of financial management and functioning thereby enhancing the delivery of tailor-made services while bringing forward the decentralisation programme (NHS England, 2009, para. 6).
Since the inception of NHS, various changes have come into force with the most prominent occurring in 1983 after recommendations from the Griffiths report. The introduction of general management staff as the highest organ in the hospitals with autonomy on financial matters came into effect. Although the reforms never achieved much, future changes improved on this premise after realizing the importance of clinicians to sit in the management boards. In 1990, a directorate structure was established thereby allowing clinicians to participate in decision making and policy formulation at the hospital levels and local trusts and authorities countries (Neogy & Kirkpatrick, 2009, p. 14).
Further changes introduced by the labour government encouraged the hospitals to convert to foundation trusts with the sole aim of putting emphasis on the role of management in improving the overall delivery of quality care. More importantly, the fact that managers have been held accountable for the clinical performance has reinforced the work of the clinicians in the NHS. The policy recommendations in early 2000 required the adoption of clinical directorate whereby the directors and the middle managers exercise executive powers in terms of managing the human resources and financial responsibility. Although the percentage of clinical managers is low compared to that in Italy, the stakeholders cannot ignore their involvement. In line with these changes, professional bodies noticed the importance of acquiring management skills thus enhancing their capabilities in running the hospitals.
Majority of clinical managers have undertaken training through making them more competent in executing their responsibilities. In accordance with the NHS plan of 2000, the size of the workforce was expected to increase substantially while encouraging the speedy implementation of national guidelines at the local management level. Involvement of clinicians in the management had to be applied to enhance the overall achievement of the 10 year plan that intended to bring far reaching reforms in management and functioning of the health systems in the UK (NHS England, 2009, para 10). Furthermore, changes introduced in 2005 and in 2009 have seen the reduction of bureaucracy in the health systems thereby releasing millions of pounds in savings to the frontline services in the UK hospitals.
NHS boasts of a sizeable proportion of clinicians serving as executives, middle level and first line managers in the clinical and health systems. Apart from acting as the organizational heads, the senior executives are mandated to undertake responsibilities in managerial and financial matters (Sausman, 2001, p. 20). In addition, setting and maintenance of clinical standards has become one of their core responsibilities considering the demand for quality care for patients. Although majority of the responsibilities aimed at improving public accountability are generally new, the managers and the executives have achieved tremendous achievements in NHS management. Their background in clinical practice has conferred greater advantage in propelling the clinical units into achieving their set objectives and goals. The clinicians and non clinicians has formed an indispensable combinations has become crucial for the success of the NHS.
However, the involvement of clinicians in the hospital management has elicited controversies and tension with the non-clinicians. While the clinicians such as nurse managers and first line managers have gained autonomy in their carrying out their responsibilities, conflict between profession and managerial work continue to persist. In this regard, the doctors and nurses have had to contend with increased workload coupled with conflicting interests in the workplace. It is therefore worth noting that the provision of the necessary trainings and bonding seminars must be enhanced to promote harmony in the managerial field.
Policy changes in the health systems
Massive reforms and policy changes have taken place in the European health system in the last three decades. The need to foster the doctors-managers relationships and improve cost effectiveness of the health systems has occasioned the initiation of these reforms. Furthermore countries such as Denmark experienced political dissatisfaction particularly with the running of health institutions by the counties thereby preferring the centralised system. On the other hand, the surge in the recurrent expenditure such as doctors fees paved the way for action for Netherlands. Reforms in Denmark started with the formation of the troika model that comprised the general manager and one member from the nursing and medical profession in the management structure. In contrast, the Italian health system embraced the clinical directorate model in 1992, which was officially adopted in 1999, as a measure to enhance the running of the health units. Denmark and Italy embarked on these reforms to eliminate the inefficiencies resulting from the previous approaches.
Although the integration of clinicians in the management came late, tremendous improvements in terms of efficiency has been observed in the two countries (Neogy & Kirkpatrick, 2009, p. 14). On the other hand, Netherlands introduced far-reaching reforms aimed to reduce fees paid to doctors by forming a representative committee to replace the unilateral organ led by doctors alone. This in essence brought down the influence of doctors while increasing the participation of all health workers in the budgeting and administration. In this case, the Netherlands shifted towards the Denmark and Italy model by realising the need for consultative leadership. Despite the fact that its hospital underwent turbulent times, France conclusively introduced the decentralisation policy that gave the regional and internal structures in the hospitals the power to decide their management. The involvement of clinicians’ in administrative and budgeting led to improved efficiency. In contrast, Germany had never introduced any reforms on the clinician-management concept hence allowing their health units to embrace business models (Blank & Burau, 2007, p.45). The lack of any policy direction is a paradigm shift from the approaches applied in other European countries and appreciated particularly during the period most of the countries were in financial turmoil.
In order to achieve more benefits from the clinician-managers, it is imperative for the concerned to implement policy changes based on evidence-based practice. Moreover, the integration of the reforms should be planned systematically and must respect the professional ethics while improving the organisational culture. Fostering interdisciplinary training and education for the clinicians and the managers is therefore paramount particularly when carried out early in their professional career. The interdisciplinary trainings would eliminate the discord that clinicians have on non-clinicians managers (Nash et al 2003, p.652). More importantly, the policy makers should apply promotion and embracement of policy frameworks that encourage a combination of clinical experts with professional managers in order to achieve improved performance.
Methodology
Introduction
This chapter entails identification and selection of a research design to be used in conducting the study. Qualitative research designs are considered. In addition, a description of the procedure utilized in data collection and analysis is overly discussed. Literature review is applied in the data collection due to its simplicity and the enormity of information expected from the study as the key data collection methods in the study.
Study design
Research design defines a framework that enables a researcher to collect data appropriate to conduct a study regarding the issue under investigation. Research design enables the research findings to be more logical and appropriate. The research design selected for a particular study should contribute towards improving the degree of accuracy in the study. In addition, the design adopted should reflect the entire research. This entails the process of collecting data from the field, analysis and elaboration of research questions. According to Yin (2009), research design acts as an architectural blueprint for a particular research project.
Research design methods
Systematic reviews, realist and thematic analysis are utilised since they offered moderated information that took into consideration several sources in their reviews. Searching for the relevant empirical evidence takes centre stage at this point with the sole aim of supporting the theoretical framework, either in a contradictory or modifying manner.
Thematic analysis is pivotal particularly when comparing previous studies that utilized quantitative and qualitative data. Thematic analysis is a research approach that mainly involves analysis of information by creating and overly applying codes in data management. Taking into account the relatively large amount of data from the previous studies, realist reviews are vital in the analysis and compilation of enormous literature before arriving in a common position (Lacey & Donna, 2001)..
Realist review is useful because of its applicability in complex settings. Its holds its basis on the latest invention of an emerging realist approaches that are pivotal in evaluation of influence of the doctors’ managers relationships in healthcare management. The fact that the method provides and in-depth explanation and analysis makes it a useful tool that achieves holistic aims such as deducing the relationships between several agents. The nature of the relationships may be deduced by ascertaining who works for whom taking into account the reasons and the manner the tasks is executed.
Literature reviews is a research design that tries to review the major and critical points espoused in knowledge presented in certain studies while examining them in relation to the methodological and theoretical frameworks utilised. In view of the above, this study applied literature review as the research design to enhance the relation of the various ideas and approaches presented in the previous studies.
Literature reviews
The research objectives were met through the usage of literature review. Literature reviews was useful because of its applicability in complex settings. The fact that the method provides and in-depth explanation and analysis makes it a useful tool that achieves holistic aims such as deducing the relationships between several agents. The nature of the relationships may be deduced by ascertaining who works for whom taking into account the reasons and the manner the tasks is executed. In this case, the National Health Service was evaluated based on factors that determine and influence the degree to which the clinicians are involved in the healthcare management. The study design employs a longitudinal approach whereby the investigation of the degree of involvement of the clinicians in management was conducted, collection and analysis of the available information to come up with a report that reflects the management scenario (Yin 2009, p.43). Considering the fact that the main aim of the study was to evaluate managerial experiences of the clinicians, literature review provided the most appropriate methodology to utilise in the study on National Health Service.
To start with the researcher is expected to develop and clearly explain the theoretical frameworks in addition to the assumptions made. Assumptions on how the relationships between the clinicians and the other managers interact, and the impact of their contribution on policy were ascertained. Searching for the relevant empirical evidence takes centre stage at this point with the sole aim of supporting the theoretical framework, either in a contradictory or modifying manner. The compiled results should have the ability to incorporate the theoretical understanding with more advanced and well-researched evidence that takes into consideration its relevance to the study. In this end, the incorporation is pivotal in shedding light on the relationship between clinicians and efficiency in healthcare management while explaining the mechanisms and the environment the workers are able to executive their responsibilities. Focus is hence turned to the contextual relationships in combination with the relevant outcomes in the organisation.
The approach is also vital since it is premised on explanation building where a researcher takes an in-depth analysis or evaluation of a particular study topic. Literature review gives a holistic view of an event or situation taking into account its merits and demerits. The suitability to utilize a theoretical framework in the synthesis and discussion of information is a major advantage offered by the study approach (Saarikoski, 2003). The research design has shortcomings in that the study findings cannot be utilized to reflect the management experiences in other health systems since the entities operate in different conditions.
Data collection and analysis
Yin (2009) defines data collection as the process through which the researcher prepares and collects data from the field in an effort to ensure that sufficient data is available to conduct the study. Data collection is a key consideration since it ensures that the research design utilized is effective. This arises from the fact that there is a direct relationship between the data collected and the quality of research. The researcher should consider a number of issues in the process of collecting data. These include the source of data, amount of data required, form of data, its reliability and accuracy. There are two main categories of data sources available for the researcher. These include primary and secondary sources. People are the core sources of data with regard to primary sources. On the other hand, secondary sources include documented works such as administrative records and from management information systems. The form of data has an effect on the study’s feasibility that is in turn determined by data availability. The various forms of data available include documented evidences such as reports, case studies and reviews.
The amount of data required for the study must overly be estimated prior to conducting the study (Yin, 2009). This is achieved by making a decision on the number and types of sources to use. In the process of collecting data, it is vital for the researcher to conduct site selection. This refers to the field from which the data is collected. With regard to this study, the researcher used the field as the main source of data. The site selected plays a significant role in determining the method of data collection to be used. The researcher has the discretion to use the most effective method of data collection that he or she deems to be the most effective. Saarikoski (2003) asserts that incorporating several sourcees ensures that the process of data collection is comprehensive. The resultant effect is that the quality of the research is improved. In an effort to improve the reliability of data collected, primary methods of data collection were used.
Data collection was achieved through literature review of previous studies undertaken on the degree of involvement of clinicians in the healthcare management of the National Health Service units including the hospitals, authorities and trusts. Studies delving on the professional bureaucracy, roles and competencies of clinician managers and the policy implications occasioned by the infiltration of clinicians in the NHS management. The search of papers was carried out the CINAHL, Medline and PsycInfo databases were utilised. The research materials published between the years 1980 and 2009 were considered for the study. A comprehensive list of journals were collected from a variety of sources that publish medical and nursing journals in combination to allied health professionals materials that encompasses the relevant studies on managerial roles of the clinicians.
Literature review was utilised since it offered moderated information that took into consideration several sources in their reviews. Studies selected for the systematic reviews include those that had investigated the managerial roles of the clinicians and their relationships with the other professional managers. Referencing terms such as “doctors/managers”, “Managerial roles”, “role conflict”, “clinical manager/policy” and “professional bureaucracy” were applied to aid during the literature search. Furthermore, the reference lists of the previous works undertaken by renowned researchers were checked to identify relevant study materials. The complete search of the databases produced 251 references before reducing to a partly 176 after limiting the search to clinician managerial roles. In addition, a further restriction of the search to managerial roles in relation to conflict, bureaucracy and policy implications produced 25 references. Owing to limitations of accessibility, only 20 studies were utilised in the final analysis. The 20 studies included 17 original investigations of managerial roles of the clinicians and 3 reviews. Among the 17 studies, 15 were case studies while the rest were reports.
Papers and works selected for the study had to meet a certain set of criteria. All the works published in English not earlier than 1980 since that is the time major reforms targeting the management structuring started in the NHS. The introduction and implementation of Griffith report saw the involvements of general managers before a reversal of policy started taking momentum in the following several years reaching its peak in the last few years. Policy changes in the last two decades have emphasized the involvement of the clinicians in all spheres of healthcare management. In addition, the studies must have a systematic methodological approach and discuss the relationship between clinician involvement in management with bureaucracy, policy changes and their functioning in the establishment. Furthermore, coverage of at least one of the major cadres of health professional was instrumental in the selection since their influence is widely felt at the management and operational levels.
Results and Findings
Introduction
Literature review is an important research design tool especially in studies requiring an in-depth picture of a management in healthcare. This chapter will present the results and findings from the data collected from the review of previous studies. Analysis of the data to summarise the major managerial roles bestowed upon the clinician managers will be conducted with particular interest on the nurses and doctors since they form the largest proportion of the workforce. In view of the studies selected the potential areas of conflict in the work place with regard to the relationships within the profession and t professional relationship and with other managers. Considering the health sector is a multifunctional unit, it therefore brings to fore the need to come up with relevant policy changes intended to safeguard the interests of the concerned groups while removing ambiguity in their functioning.
We found 251 studies involving doctors as managers in the overall running of the National Health Service. Out of these, 231 studies were excluded because of failing to address the issues of policy implications and role conflict in the clinician-manager relationship. Only 20 papers (12.55%) met the required criteria of denoting a clear relationship between managerial roles and professional bureaucracy in relation to barriers and policy changes in the NHS, published between 1980 and now, and participants are from a cadre of health professionals with a sizeable representation in the hospital.. Of these 15 were case studies, 2 were reports while another 3 were reviews of previous literature. A partly four studies utilised quantitative research methods while the others applied qualitative approach. Majority of the studies did not utilise comparative analysis in their methodology.
Different models and theoretical frameworks found application in the papers carried out in different circumstances and dissimilar setting depending on the stage of development in the NHS. Mintzberg, grounded theory and Floyd & Wooldrige approaches received application in the various studies. Overall, information collected involved the degree of involvement of clinicians in management of the NHS and in particular their roles, level of involvement, professional bureaucracy and the policy changes in the management of healthcare in the UK. However, minimal research studies delving on the efficiency brought by clinician-managers were identified during the search.
What are the major roles taken by the physician managers in the health care organisations?
Healthcare managers’ job entails intensive management of relationships and the response to various external changes (Duncan et al 1988, p.1-3). Owing to the fact that the areas in relationship are inherently intertwined, the manager may lack the power to direct them while other external forces lack the required power to influence the decision making within the organisation. Stakeholders in the heath sector need leadership that can effectively direct and manage the complex and ever changing relations. Physicians, patients, medical practices coupled with government agencies formed the most important stakeholders in the hospitals.The majority of the papers denoted that since the early 1990’s, an ever-increasing trend of doctors and nurses involvement in healthcare management has occurred in the NHS (Burgoyne & Lorbiecki, 1993; Fitzgerald & Sturt (1992) and Shewan & Read (1999). There was greater willingness for incorporation into the management particularly from the nurses. Findings in the reports and case studies agreed on the desire and involvement but the level varied across the various studies depending on their year of publication.
Low involvement of nurses was reported compared to doctors although small numbers of health workers were integrated in the management structures (Currie & Procter, 2001; Currie, 2006). Varying degrees of discontent among the professional managers was recorded in several reports and case studies. In addition, clinicians who reported greater willingness to join the management felt dissatisfied by the management structure where a non-specialist in the field was charged with the mandate of leading with all the clinicians fully accountable to them. The level of involvement varied across the management structure. While majority of the reports indicated that a high number of nurses were involved in the management at junior levels (Shewan & Read, 1999; Sausman, 2001; Currie, 2006). It was common to find majority of the nurses serving in positions of first line and middle managers while partly a few received consideration for the executive positions. The nurses perceived this scenario as a kind of segregation and discrimination by the doctors and other stakeholders. In line with this, doctors were found to comprise a majority of the clinicians involved in top management positions in the trusts and hospitals. However, a few reports denoted that a sizeable proportion of the clinicians expressed discontent with their involvement in healthcare management (Currie, 2006; Jones & Dewing, 1997& Llewellyn, 2001).
Strategic involvement of middle managers in proposing and development of organisational culture is instrumental in shaping the overall organisational culture. Previous studies indicated culture as among the major influences in the strategic management of healthcare. Professional clinicians were embracing strategic management roles on top of their clinical practice (Llewellyn, 2001). In contrast, some studies have reported varying involvement of clinicians in strategic management with policy and size of the institution remaining the main determinants of the participation (Jones & Dewing, 1997). Professional managers are hence faced with a challenge because the involvement of middle managers in the overall development of the strategy must occur if the organization needs and expectations are to be met.
Varying outcomes exist on the role of strategic involvement and cultural influences to healthcare organisation. High quality and focussed care was offered to patients especially when they were overly engaged in strategic development (Carney 2002, p. 56). In line with this, Thorne (2000, p. 45) noted that culture was imperative in the effective delivery of superb patient care by nurses working in public hospitals wards. A demonstration on the link of high quality care to the changing culture in the organisation was carried out. In fact strategic has been regarded as the pillar, which leads the organisations and hospitals to thrive.
Involvement of clinicians and non-clinicians in the strategic development is believed to result in improved productivity occasioned by diversity in skills. The presence of professional clinicians as middle managers, influences organisational culture largely than non-clinicians achieved, due to the fact that the socialisation process is part of daily schedule of the clinician. Middle managers who were professional clinicians possessed a much stronger cultural value largely based on a professional and ethical approach especially in the effective delivery of excellent and quality care to the patients (Carney 2006, p. 30).
Clinicians are overly involved in communication roles such as representative and staff duties particularly in the executive boards. The physician managers have become accustomed to representing the views of other professionals thereby safeguarding the growth and integrity of the medical profession (Leatt, 1994, p. 174). More importantly, the physician managers come in handy when offering collateral roles whereby they conduct dispute resolution when two specialities are in conflict. Since majority of the individuals engage in monitoring of projects that are overly strategic to the organisations, it becomes imperative for them to portray superb communication skills. Physician managers have regularly come forward in ensuring professional standards are respected and conform to the organisational standards. Moreover, the physician managers (Willmot, 1998) also achieve ensuring cordial relationships among the various professionals and external environment.
Majority of the papers reviewed lacked enough quantitative data to enhance their rating. The fact that most of them were descriptive enabled the researchers to collect large portion of information on the roles of the doctors and nurses. A review conducted by Shewan and Read (1999, p. 78), denoted that role developments was inherently influenced by certain forces in the environment. Majority of the studies indicated that policy forces and professionalism were cited as the major influencers in taking up some responsibilities. NHS middle managers acted strategic roles that mainly required them to synthesize strategic ideas for consideration by the executive and the top brass. Although only less than one third of the studies reported the scenario, the participants who denoted it as a part of the barriers to successful implementation of plans to improve healthcare in the hospitals and trusts (Currie & Procter 2005, p. 45) emphasized its impact on morale. In other reports, the middle managers indulged in entrepreneur roles where they are overly in charge of synthesising of organisation strategic plans with the sole aim of improving efficiency while ensuring cost effectiveness in the whole system (Currie 2006, p. 45; Willmot, 1998; Kieran & Rundall, 2001).
On the part of executive positions in the hospital and trust boards, doctors occupied most of the positions reserved for the healthcare workers. Neogy & Kirkpatrick (2009) noted that although majority of the members originated from non-clinical backgrounds, inclusion of clinicians was pivotal in pushing the clinical agenda that was more interested in improving patient care. Management roles at this level were limited as espoused in more than half of the studies. Some studies reported that the managers held considerable influence n the decisions made by the board (Currie & Potter, 2005). While the other members of the board emanated from core areas of an organisation, the doctor manager was responsible for formulating policies and offered guidance on mattes relating to public health in the board (Jones &Dewing, 1997; Currie, 2006). A few studies noted that the clinical directors have autonomy to execute budgetary allocations while maintaining responsibility of the human resources (Neogy & Kirkpatrick, 2009; Jones & Dewing, 1997). Sausman (2001, p. 21), noted that the executives in the NHS had overly achieved autonomy particularly when executing financial and managerial responsibilities. On the contrary, Forbes, Hallier and Kelly (2004, p. 168), noted conflicting results on achievement of the expectations of the managerial roles and financial obligations. The lack of the ability and skills to execute the responsibilities were observed in more than half of the sample population in the latter study. While managerial roles are limited at this level, mixed feedbacks were reported across the studies with majority of them indicating inefficiencies in the execution of the specific responsibilities (Edwards, 2005).
In contrast, the roles of the middle management was enormous owing to the fact that they were supposed to ensure efficiency at their department while developing strategic tools that would work in the achievement of the same (Sausman, 2001; Warwicke, 1998; Williams, McGee & Bates, 2001). The middle managers therefore served as the guide of the organisation towards its achievement of its strategic goals and targets. Furthermore, the middle managers oversaw the functioning of the first line managers and ensured distribution of workforce in their workplace was in tandem with the national priorities of NHS. In contrast to the large numbers of general management, the middle clinical managers provided much guidance particularly with regard to technical expertise (Edwards, 2005).
According to Currie (2006, p.5), the middle managers particularly the nurses were found to offer much input in the decision making. A shift from the previously held obligations of implementing policies from the top level was hence witnessed in about half of the studies. All the reports indicated middle managers were overly involved in supervising other fellow clinicians thereby resulting in conflict between management and professionalism. In particular, the radiographers were found to develop some hybrid roles that commensurate the changing environment in the NHS and in the other cadres of health professionals (Forbes, 2000; Williams, McGee & Bates, 2001).).
In other studies, the clinicians were found to play several roles that involved acting as a gatekeeper to accessibility of specialised care (Warwicke, 1998, p. 331; Burgoyne & Lorbiecki 1993, p. 252). Nurse Managers performed a wide range of activities besides their normal chores of supervising the bed making and washing. A study carried by Surakka (2008, p. 526), concurred with several others in identifying accountability and managerial duties as major components of the job description. In comparison, the first-line managers were regarded as the most useful personnel in the management structure. The majority of the studies indicated that their major role was to bring together a harmonious workforce through creation of a proper working environment (Williams et al, 2001; Kieran & Rundall, 2001).
In order to become effective in offering leadership and direction, training courses and on-job training came in handy (Ham, 2010, p. 6). Skill mixing was greatly enhanced by induction and integration of competence training approaches in boosting the skills of nurses in readiness for managerial duties. A study carried out by Currie and Procter (2005, p. 65) identified skill mixing that takes into account the individual needs and preferences were overly introduced. While skill mixing and on-the-job training found wide application in several studies, the researchers asserted that proper planning and implementation of the training program is imperative in achieving the end results. Substantial differences in the conduct of the managers were recorded between pre and post training (Edwards, 2003).
Financial management in terms of health economics has become another key area that clinician managers must exhibit outright competence. Management in healthcare systems must also be overly conversant with health information systems especially at this age of technological advancements (Forbes et al, 2004, p. 170; Burgoyne & Lorbieckie, 1993; Currie & Procter, 2001). Knowledge of the administrative and financial systems combined with the strategic decision support systems is instrumental in aiding the top brass management in coming up with competitive and long term strategies especially in the health insurance and private health sectors. Evaluation of financial performance with the aim of ascertaining the profitability and the manner of resource utilisation particularly in the face of resource limitations has achieved prominence in healthcare finance (Broyles & Falcone,, 2005, p. 34; Burgoyne & Lorbieckie, 1993; Currie & Procter, 2001).
How does professional bureaucracy in health care impact on physicians and other health care workers taking up managerial duties?
In tandem with previous studies that indicated simmering conflict between several aspects of the management front, this review was able to deduce some interesting findings. While the majority of the studies asserted increased conflict between the profession and management, several authors denoted persistence in conflict between the professional and clinician managers in the NHS. For instance, Forbes et al (2004, p. 170) reported the existence of poor working relationship between the clinician manager on one hand and the professional managers and the investors on the other. More importantly, mutual disrespect and discontent on the performance of the managers was reported by the doctors mainly due to the doctor-management interface and the overly rejection of some of their conditions on autonomy and trust (Marshall, 2003; Davies, 2003; Freedman, 2002; Atun, 2003).).
Clinicians continually engage in conflict and acrimonious relationships with other managers unless proper controls are entrenched in the management systems (Burgoyne & Lorbieckie, 1993; Currie & Procter, 2001). Reluctance to share and direct the middle level and first level clinician managers in the management of the staff has raised tension and discontent between the two professions. That notwithstanding, tension has gripped the doctors and the managers with regard to their functionality. Differing perspectives and approaches to core aspects such as accountability, finance, guidelines and coming up with targets has also resulted in acrimonious relationships (Edwards, 2003; Atun, 2003).
Role conflict across the managerial levels was reported in several studies. Shewan and Read (1999, p. 78) noted a heightened conflict between professionalism and managerial roles in the first line, middle level and executive level. While a sizeable proportion gave up on clinical practice, others had to learn to juggle between the two demanding responsibilities (Freedman 2002, p. 135). A study conducted by Fitzgerald and Sturt identified accountability, motivation, supervision and development of strategies as the major roles a clinician should put emphasis on while serving in the clinical directorate model (1992, p. 139). Lack of understanding of managerial roles resulted in tensions and conflicts amongst the professionals and the general managers (Forbes et al 2004, p. 168; Smith & Preston 1996, p. 32). A study involving radiographer managers denoted a surge in cases of role conflict and tension occasioned by the switch to hybrid roles in management (Forbes & James 2000). The perceptions of the desired goals and roles for first line managers have resulted in conflict with their superiors who believe they are usurping the mandate of the senior level management (Willcocks, 1994; Kieran & Rundall, 2001).
First line nurse managers are overly affected by the nature of the supportiveness in the organisational climate. The issue of decentralisation plays a major role since it directly and indirectly affects the organisational commitment through job satisfaction coupled with organisational commitment. Furthermore, retention of nurse managers is also fuelled by many factors such as effective communication (Warwicke, 1998, p. 331; Burgoyne & Lorbiecki 1993, p. 252; Willmot, 1998). The availability of superior and clearly expressed expectations and the possibilities of participating in the organisation planning and strategic decision making played a key role in determining the retention rates particularly in Australia and America (William and McMurray 2003, p. 76). More importantly, effective administrative systems, compensation, life work balance and lack of negative stress experiences enhanced the retention of nurses’ managers (Neogy & Kirkpatrick, 2009; Jones & Dewing, 1997; Sausman, 2001).
Factors such as interactions among the researchers and policy makers are imperative in the decision making by healthcare managers and related policy makers (Neogy & Kirkpatrick, 2009). The emergence of new frontiers such as managed care has signalled the urgent need for redefinition of the roles of the physicians. It is therefore worth noting that physicians’ executives have the greatest potential of becoming champions of integrity in clinical practice while ensuring the patients gets the best services from the facility.
What policy measures put in place or are needed to safeguard the interests of all stakeholders affected by the switch?
Policy changes targeting the professional bureaucracy has been emphasized in almost all the studies (Thorne, 2002, p. 14). The fact that policy has a paramount role to play in influencing doctors and managers relationships has made its application to occur at a slow pace in the NHS. Studies depicting the struggles between the professionals and the clinicians in management of NHS have become persistent since clinical directorate level of management came into force. From the studies, a paradigm shift towards better managerial roles and professionalism has occurred thereby ensuring that the clinical directors are overly involved in strategic development (Burgoyne & Lorbieckie, 1993, p. 247). While some clinicians embraced managerial roles as alternative to practising, others keep struggling with both responsibilities. Poor relationships between the managers and clinicians have continually increased thereby resulting in synthesis of ways of dealing with the clinician-management gap (Forbes et al 2004, p. 168; Marshall, 2003). Taking into account the influence from the clinician and managers on service delivery, policy changes on professional bureaucracy is urgently needed.
Discussion
Introduction
The lack of utilisation of comparative analysis and the application of various methodologies in the studies helped bring a holistic picture of the situation in the NHS management. More importantly, analysis of the 20 studies yielded useful information on the managerial roles of clinicians in the NHS while also taking into account the conflict and the policy changes influencing the clinician-manager relationships. Owing to limitations in research materials on the same topic, this study will provide crucial information to the policy markers and the managers. The utilisation of literature review in the eventual provided concrete information that served to validate or invalidate conclusions derived from other studies.
What are the major roles taken by the physician managers in the health care organisations?
The introduction of healthcare reforms in UK led to an upsurge in the number of clinicians joining the managerial ranks. That the previous studies depicted the involvement of clinicians in management makes the study provide additive material to the available pool of information. The level of participation of nurses in management has been occasioned by the low social status accorded to them by the other cadres of health personnel. Although the doctors provide guidance and instruction to the nurses, the nurses are of the opinion that the doctors have overstepped their mandate by trying to control the nursing practice and profession. The findings contradict Floyd and Wooldridge (1996) assertion of inclusion approach in management and overly respect for interested parties in a bid to create a harmonious relationship in the healthcare setting.
On the other hand, doctors have shown reluctance in accepting managerial responsibilities due to the obligations and the demands of acting as the manager in the hospital environment. Juggling between the managerial duties with clinical practice has proved challenging to doctors. In comparison, Harrison and Ahmed (1994) asserted that the decline in medical autonomy in the last three decades has been brought about by the capitalistic nature of the economy coupled by the global meltdowns witnessed during this period. In support of the clinician involvement in management, Floyd and Wooldridge (1996) stressed the need to embrace an inclusive approach when making strategic decisions while outlining the potential negative consequences in cases of exclusion and its overall impact on the work outcomes and understanding of the strategies. In view of the complementary nature of the various cadres, Hodges and Rundall (2003) emphasized the benefits and positive impacts with regard to the synergic nature of combining the middle managers, clinicians and professional managers in running of healthcare systems.
The improvement of the knowledge base of the patient and the availability of adequate information on patient care for the consumers has put a lot of strain on the doctors who earlier had the preserve of treating patients without being questioned. According to Davies, Hodges and Rundall (2003, p. 638), the tendency of managers being taken to task over professional negligence and misdemeanour of their health systems by the regulators have continually served to dissuade the medics from taking the jobs due to the fear for prosecution. A constellation of forces working in the destabilisation of hospital managerial environment exist with regard to clinicians been put off by the prospects of receiving instructions from non-clinicians especially on matters they deem appropriately and better placed to deal with compared to the managers. Floyd & Wooldridge (1996, 1997) asserted that the exclusive approach has the potential to bring collision between middle level and the first line managers with the administration system with regard to differences in approaches in the management of the workforce and the functioning in the health systems. Increasing discontent will be reported if the repercussions of applying clinical directories in the management of healthcare systems are not appropriately checked.
Stigmatisation and discrimination of nurses also prevented them from attaining senior managerial positions when compared to their doctors’ counterparts (Carney, 2004). In comparison, McMurray and Williams asserted that lack of adequate supervisory encouragement and fairness coupled with poor organisational climate has hindered the progression of nurses’ managers in their career path (2006, p. 30). However, increased participation in decision making, as espoused in inclusive approach of management, would encourage nurses to take up the top executive positions (Carney, 2004, p. 345).
The impact of semi-autonomy of middle managers in strategic decisions lowers the morale hence curtailing the successful implementation of plans to improve healthcare in the hospitals and trusts. On the part of executive positions in the hospital and trust boards, doctors occupied most of the positions reserved for the healthcare workers. Inclusion of clinicians was pivotal in pushing the clinical agenda that was more interested in improving patient care. Management roles at this level were limited owing to the bureaucratic regime that was more interested in achieving sustainability in the system. Although the managers held considerable influence in the decisions made by the board, their participation fell short of the integrative approach espoused by Floyd & Wooldridge (1996, 1997). While the other members of the board emanated from core areas of an organisation, the doctor manager was responsible for formulating policies and offered guidance on mattes relating to public health in the board. The inability of clinicians to have sizeable representation in the pyramidal structures, translates to exclusion in vital decision making. More importantly, the nurse managers are captives of the medical power who have failed to accept that nurses can be in charge of their own destiny (Strathem, 1994). Perception that senior executives were discontented with the increased autonomy of professional clinicians thereby resulting in power struggle that shifts strategy development to the managerial component of the top brass (Floyd & Wooldridge, 1996, 1997), strategic consensus and financial accountability (Carney, 2004), all of which may result in influencing the functioning of the healthcare system negatively.
That the clinical directors have autonomy to execute budgetary allocations while maintaining responsibility of the human resources is a step forward. The partial autonomy received by the executives in the NHS when executing financial and managerial responsibilities could was largely a realignment of the power distribution (Shortell & Kalunzy, 1994). In contrast, the roles of the middle management was enormous owing to the fact that they were supposed to ensure efficiency at their department while developing strategic tools that would work in the achievement of the same. The middle managers therefore served as the guide of the organisation towards its achievement of its strategic goals and targets. The functioning of the first line managers and distribution of workforce in their workplace was in tandem with the national priorities of NHS. The middle management had received some form of autonomy by receiving powers to develop policies, albeit at a limited level, which is in itself a shift from the implementing role. The role of middle managers espoused in this review denotes a semi autonomous role which is contrary to the more autonomous espoused by Floyd and Wooldridge (1996, 1997).
Middle managers assert their authority in supervising other fellow clinicians thereby resulting in conflict between management and professionalism. In particular, development of hybrid roles that commensurate with the changing environment and acting as gatekeeper to accessing specialised care. The paradigm shift to achieving more power in making strategic decisions may herald a major milestone for clinicians since it represents the weakening of the professional bureaucracy (Biddle, 1986). Nurses and doctors in the middle management behave in certain ways depending on the expectations of their seniors and the central governing authority. Conflicting expectations of the contribution of middle managers by the government and the doctors makes them remain as spectators in the change process (Mintzberg, 1973; Ham, 1997). The confusion brought by the power struggle between the two authorities has a potential of instigating role conflict to the middle managers.
Managers in the NHS have been well equipped to perform communication and monitoring roles in the management of key functions in the health systems. Skill mixing and on job training on communication has achieved tremendous improvement in the transfer of information in the hierarchy thereby ensuring responsibilities are efficiently executed. However, communication was curtailed where there was existence of many layers in the hierarchical ladder of management (Surakka, 2008; Forbes, 2000). Literature relating to application of hierarchical layers of management denotes that excessive layering will occur in any system utilising hierarchy. In addition, Mintzberg (1994) asserts that communication breakdown will always occur in the event where there is passage of information through many channels. In comparison, Mintzberg (1997) contends the need for swiftness in judgmental capacities with regard to passage of information to the lower levels of the organisation.
While the functioning of the middle managers share similarities between the private and the state run utilities, several changes on the overall layout are needed to fast track development by unlocking the potential of managers. To start with, middle managers in positions that has constant interaction with the external environment thereby making them strategic in coming up with initiatives that has the potential to propel the organisation to new heights (Floyd & Wooldridge, 1997, p. 472). In tandem with the aspect of interaction, managers should be kept abreast in accessing information hence enhancing their roles in provisions of alternative strategies in development especially at the upper and lower ends of the middle management. Delayering experienced by the participants is inherently associated with the positioning of the middle manager in the hierarchical approach while changes into the hierarchical approach may have negative or luke- warm consequences to the development of the strategic roles of middle management (Mintzberg, 1973).
Floyd and Wooldridge (1994) together with Frohman and Johnson (1993) have suggested the shift from the traditional hierarchical approach increases the potential in middle managers while improving their competitive advantage in the long term. A shift from acting as implementers is imminent and is widely accepted to take the NHS by a storm. Inadequacy in power and authority has resulted in the execution of boundary spanning roles in the NHS with the conflict between the clinicians and non-clinicians continually impeding the delivery of better services in the NHS. The inequality in access of the power in the NHS and in US healthcare system has limited the functioning of nurses while promoting the uptake of leadership positions by the doctors. Management roles for physician managers in the NHS are increasingly becoming a burden to the physicians thereby making them to relinquish their professional roles. Over the time, the doctors and the nurses have demonstrated their capabilities in delivering their communication, representative and financial roles in the NHS (Floyd & Wooldridge, 1997).
Several barriers to career advancements in the management hierarchy reported mainly affected all the other cadres of health professionals except the doctors. Doctors’ advancement to top executive positions was largely affected by the political interference. Inequalities in accessing promotions are contrary to assertions in Floyd and Wooldridge (1996, 1997). More importantly, the study findings contradict Mintzberg theory of managerial since the organisation lacks to appreciate the contribution of certain cadres thereby resulting in dormancy and underutilisation. Nurse Managers in the NHS have faced a myriad of constraints and barriers that have continually limited their career roles at the junior and middle management levels. Insistence on financial skills and professional stigma has played against the nurses in gaining promotion in the NHS hierarchy. In comparison, Faugier and Woolnough (2001) was quick to point out that similar predicaments coupled with age and gender remained the greatest obstacles nurses in Sweden and other Eastern European countries faced. In contrast, nurses in Sweden had received increased autonomy where they exercise financial obligations and personnel management unlike in the UK. In line with other studies, Skytt et al (2007) noted that nurses’ managers were overburdened with several responsibilities but overly lacked enough authority to carry out independent tasks. On that note, involvement of nurse managers in NHS contradicts Mintzberg theory of managerial roles while concurring with Taunton et al, (2004).
Conflict in the management
The clinicians and non-clinicians have continued experiencing acrimonious relationships particularly when executing their responsibilities. Poor working relationships brought about by duplication of roles and lack of clear demarcation of job description was overly responsible for unwarranted efficiencies in coordination between the two groups (Marshall 2003; Davies 2003; Burgoyne & Lorbieckie 1993, p. 250). Conflict in personnel management roles formed the largest cause of acrimonious relationship in NHS. In comparison, lack of empowering clinicians was responsible for the misfortunes encountering the Swedish health system (Skytt et al, 2008, p.1013).Empowerment of the first line nurse managers managed to offer a reprieve that ushered a rejuvenation of the Swedish healthcare. The integration of the boundary roles and finding a common ground between the clinicians and non-clinicians as espoused in the inclusive approach was instrumental in bridging the gap the management gap (Persson & Thylefors, 1999, p. 13); Nilckon 2003). The study findings concur with Mintzberg (1973) theory of managerial roles, and Floyd and Wooldridge (1996) assertions on the relationship dynamics in the health sector.
Role conflict
Organisational structure has become one of the major areas under which role conflict is inherently observed particularly when clinicians are faced with professional and managerial dilemmas. Although the middle and first line managers are the most affected, the implications of the role conflict has far reaching implications to the whole organisation. Just like in NHS, role conflict has hampered efficiency in managerial roles for clinicians in Germany and France. While the degree of inhibition varies, their impact has greatly hampered the strategic development of the health system while ensuring patient care services are dismal (Neogy & Kirkpatrick, 2009, p. 43). The embracement of more efficient flatter models of management would discard the traditional and bureaucratic models. In line with this, much involvement of nurse managers in strategy development from the lower to the upper level of management would help solve the role conflict dilemma since the views of the nurses would receive wide acknowledgement (Wooldridge & Floyd 1990). Adoption of flatter structures would inherently solve problems associated with conflict between the various levels of management in NHS. Changes in the structuring have overly resulted in the inception and reorientation of managerial responsibilities such as financial responsibility thereby causing conflict between the clinicians and the non-clinicians at the hospital level (Jenkins, 1995). Exclusion hampers the tendency of different managers to interact with sidelining of clinicians resulting in acrimonious relationships between the two cadres while ensuring communication is curtailed among the clinicians (Jenkins, 1995; Floyd & Wooldridge, 1997).
How does professional bureaucracy in health care impact on physicians and other health care workers taking up managerial duties?
Professional bureaucracy in the NHS has become dynamic owing to the persistent changes in government policies. Organisational restructuring and strategic frameworks has fuelled the changes in the management structures in NHS trusts and hospitals. The clinical directorate model is the culmination of reforms that brought clinicians in the management arena in the NHS. Only a minority of hospital trusts in the NHS are run by clinicians compared to slightly more than half in Italy, 15 % in Denmark and a few in the Netherlands (Neogy & Kirkpatrick, 2009). Preference of chief executive officers with a management or economic background to act above the clinician-dominated boards has received application in the European health systems. Directors in Italy and Germany enjoy substantial autonomy on budget and management of human resources unlike their counterparts in the UK NHS (Eeckloo, Delesie & Vleugels, 2007).
Middle management in the NHS is similar to several health systems where clinicians whose main function is to supervise the line managers and ensuring the delivery of quality services in the hospitals hold the positions, as espoused by Floyd and Wooldridge (1992, 1996, 1997). In contrast, Italy, Denmark and Netherlands had relatively few managers occupying general and administrative positions owing to reforms that formalised the involvement of clinicians in several functional roles in the hospitals and trusts (Dent et al, 2005; Scarbrough, & Burrell, 1996). In view of this, Mintzberg (1973) assertion is furthered by this study, albeit in the nurses and physician managers.
What policy measures put in place or are needed to safeguard the interests of all stakeholders affected by the switch?
Embracement of transformational and advanced roles for clinicians in tandem with the Blair government policy changes resulted in that catapulted clinicians into managerial positions thereby enhancing their involvement in the strategic management. The extent of application of the different management and leadership approaches in line with policy changes are instrumental in guiding the distribution of roles for managers (Kirkpatrick et al, 2009). Restratification of health systems to increase the involvement of clinicians’ involvement in has gained momentum in the work. Emergence of new divisions has resulted in the development of unique professions, which are overly aligned with the management and leaderships roles espoused by Mintzberg (1990) and Floyd and Wooldridge (1997).
The paradigm shift brought improved efficiency and organisational efficiency while reducing the budgetary allocation fro administration in the NHS. Nevertheless, the turn around was short-lived since escalation of medical costs and existence of major loopholes in the expenditures has occasioned the clamour further policy changes that will results in the reduction in managerial positions thus directing millions of pounds into patient centred programs (Walt & Gilson 1994). The policy changes in the professional bureaucracy have thrust clinicians into management, thus bestowing them with added roles in strategy development and organisational performance in the NHS.
Conclusion and Recommendations
Conclusion
This research looks into the level of involvement of clinicians in the management of National Health Service in the United Kingdom, particularly in the areas of doctors and nurses and their relationships with non-clinicians. Management is pivotal in enhancing efficiency in healthcare systems, through improving the strategy development and organisational performance. The level of involvement of clinicians especially doctors and nurses in middle and senior management have shown an upward trend in the last few decades, although the doctors are more likely to achieve managerial roles.
It is worth noting that clinician involvement is imperative due to their enormous potential in influencing the strategy development and the delivery of healthcare through incorporation of wise leadership, professionalism coupled with superb decision making skills. However, to rise up the management ladder is not an easy task as witnessed in the NHS. The clinicians must undertake managerial training, exhibit competency and build trust through showing their ability to perform the duties and responsibilities espoused by Mintzberg theory (1973). The clinician managers must demonstrate their capabilities in order to play a pertinent role in strategy development thus contributing in the adoption, planning and implementation of evidence based practice in nursing and medical care that is essential in improving care to clients. Clinicians should endeavour to cooperate with other managers particularly in matters concerning financial accountability and human resources management. Incorporating all views from the various managers forms a core premise in enhancing a focussed approach towards achieving the goals and objectives of NHS.
The NHS management should define the boundary roles of the clinicians and the non clinician managers to bring down instances of conflict. More importantly, role conflict lowers and limits the productivity of the professionals and hence addressing it is imperative in helping nurses and doctors to concentrate on managerial roles. The realisation that the managerial role is a different career path complementary to their profession will induce confidence in the clinical managers during operational and strategy development. On the other hand, nurse middle and senior level clinical managers should embrace delegation thus leaving the first line managers to deal with day to day care of patients. To effectively deliver on their managerial roles, allowing the nurses and doctors close interaction with other managers from other sectors not only improves the implementation of the strategic development while making a contribution to the to the development of successful programs in the NHS.
Continuous changes in policy and implementation of frameworks in the NHS has brought paradigm shift on the running of the NHS core activities that encompasses the contribution of different stakeholders. Rich input in terms of strategic development enhances the improved delivery of healthcare services, cost effectiveness and maximum output in tandem with the invested resources. Alteration in professional bureaucracy in the NHS has empowered and strategically placed the clinicians to deliver and fight for their professional rights and demands. Overall, the paradigm shift to more clinicians in management has yielded fruits thus policy changes proposition by subsequent governments should be critiqued to avoid watering the tremendous gains achieved in the recent past.
Recommendations
To further the research in this area, there is need for studies that will delve on the degree of involvement of clinicians at the first line, middle level and senior level management and the impact they have on the organisational development at their respective levels. Furthermore, the contribution of the clinician management towards the strategic development is required particularly on specific areas such as their impacts on improving organisational performance, patient care and financial accountability. A critical appraisal of the impact of the integration of clinicians in NHS management should be carried out with respect to the various policy changes.
Reference List
Anderson, R. & McDaniel, R. 2000. Managing Health Care Organizations: Where Professionalism Meets Complexity Science. Health Care Management Review, Vol. 25, No. 1, pp. 83-92.
Atun, R. 2003. Doctors and managers need to speak a common language. British Medical Journal, Vol. 326, pp. 655.
Balogun, J. 2003. From Blaming the Middle to Harnessing its Potential: Creating Change Intermediaries. British Journal of Management, Vol. 14, pp. 69–83.
Biddle, B. J. (1986). Recent developments in role theory. Annual Review of Sociology, Vol.12, pp. 67–92.
Bolton, S. 2005. Making up managers: the case of NHS nurses. Work employment and Society, Vol. 19, No. 1, pp.5-23.
Broyles, D. & Falcone, D. 2001. Management in healthcare systems. Oklahoma: university of Oklahoma health sciences centre.
Burgoyne, J. & Lorbiecki, A. 1993. Clinicians into management: the experience in context. Health Service Management Reserve, Vol. 6, No. 4, pp. 248-59.
Carney, M. 2004. Middle manager involvement in strategy development in not-for-profit organizations: the director of nursing perspective-how organisational structure impacts on the role. Journal of Nursing Management, Vol. 12, pp. 13–21.
Carney, M. 2006. Understanding organizational culture: the key to successful middle manager strategic involvement in health care delivery? Journal of Nursing Management, Vol. 14, pp. 23–33.
Currie, G. & Procter, S. 2005. The antecedents of middle managers strategic contribution: the case of a professional bureaucracy. Journal of Management Studies, Vol. 42, pp. 7.
Currie, G. 2008. Reluctant but resourceful middle managers: the case of nurses’ in the NHS. Journal of Nursing Management, Vol. 16, pp. 1012–1020.
Davies, H. & Harrison, S. 2003. Trends in doctor-manager relationships. British Medical Journal, Vol. 326, pp. 646-649.
Davies, H., & Nutley, M. 1999. The Rise and Rise of Evidence in Healthcare. Public Money and Management, Vol. 19, No. 1, pp. 9–16.
Dent, M., Kirkpatrick, I., Kragh, J. & Neogy, I. 2009. Medicine and management in a comparative perspective: the case of Denmark and England. Sociology of Health & Illness, Vol. 31 No. 5 2009 ISSN 0141–9889, pp. 642–658.
Dopson, S. & Neumann, J. 1998. ‘Uncertainty, Contrariness and the Double-Bind: Middle managers’ Reactions of Changing Contracts’, British Journal of Management, 9,pp. 53–70.
Duffield, C. 1992. Future responsibility and requirements for first-line nurse managers in New South Wales. Journal of Nursing Scholarship, Vol. 24, pp. 39–43.
Duffield, H. 2001. The role and preparation of first-line nurse managers in Australia: where are we going and how do we get there? Journal of Nursing Management, Vol. 9, Issue 2, pp. 87-91.
Duncan, W., Swayne, F. & Ginter, P.1998. Handbook of health care management. Washington, D.C: Wiley-Blackwell.
Edwards, N. 2003. Doctors and managers: A constructive dialogue has to replace mutual suspicion. British Medical Journal, Vol. 326, pp. 116-117.
Edwards, N. 2005. Doctors and managers: building a new relationship. Clinical Medicine, Vol. 5, No. 6, pp. 577-9.
Eeckloo, K., Delesie, L. & Vleugels, A. 2007. Where is the pilot? The changing shapes of governance in the European hospital sector. The Journal of the Royal Society for the Promotion of Health, Vol. 127, No. 2, pp. 78-86.
Everson-Bates, S. 1992. First-line nurse managers in the expanded role: an ethnographic analysis. Journal of Nursing Administration, Vol. 22, pp. 32–37.
Fattore, G., 1999, Cost containment and reforms in the Italian National Health Service, in Health care and cost containment in the European Union, E. Mossialos and J.Le Grand, Editors. Ash gate: Aldershot.
Faugier, J. & Woolnough, K. 2001. Nursing directors. Great barrier reach. Health Services Journal, Vol. 111, No. 5784, pp. 24,
Ferlie, E., Ashburner, L., Fitzgerald, L. & Pettigrew, A. M., 1996, The New Public Management in Action. Oxford: Oxford University Press.
Fitzgerald, L. & Ferlie, E. 2006. Managing Change and Role Enactment in the Professionalised Organisation. London: NCCSDO.
Fitzgerald, L. & Sturt, J. 1992. Clinicians into management: on the change agenda or not? Health Service Management Reserve. Vol. 5, No.2, pp. 137-46.
Floyd S.W. & Wooldridge B. (1990) Managing strategic consensus: the foundation of effective implementation. Academy of Management Executive, Vol. 6, No. 4, pp. 27–39.
Floyd S.W. & Wooldridge B. (1992) Middle management involvement in strategy and its association with strategic type: a research note. Strategic Management Journal, Vol. 13, pp. 153–167.
Floyd, S.W. & Wooldridge, B. (1996) Dinosaurs or dynamos? Recognizing middle Management’s strategic role. Academy of Management Executive, Vol. 8, No. 4, pp. 47–57.
Floyd, S. & Wooldridge, B. 1997. Middle Management’s Strategic Influence and Organizational Performance. Journal of Management Studies, Vol. 34, No.3, pp. 465–485.
Floyd, S. & Wooldridge, B. (2000). Building Strategy from the Middle: Reconceptualizing Strategy Process. Thousand Oaks, CA: Sage.
Forbes, T., Hallier, J. & Kelly, L. 2004. Doctors as managers: investors and reluctants in a dual role. Health Service Management Research, Vol. 17, No. 3, pp. 167-76.
Freedman, D. 2002. Clinical governance–bridging management and clinical approaches to quality in the UK. Clinical Chim Acta, Vol. 21, No. 3191, pp. 33-41.
Goddard, M. & Laschinger, H. 1997. Nurse Managers’ perceptions of power and opportunity. Canadian Journal of Nursing Administration, Vol. 34, pp. 40–66.
Hales, C. 1999. Why do managers do what they do? Reconciling evidence and theory in Accounts of managerial work. British Journal of Management, Vol. 10, pp.335- 350.
Hales, C. 2001. Does it matter what managers do? Business Strategy Review, Vol. 12, No. 2, pp.50-58.
Ham, C. 2003. Improving the performance of health services: the role of clinical leadership. Lancet, Vol. 362, No. 9380, pp. 1978-80.
Harrison, S. & Ahmad, W. 2000. Medical Autonomy and the UK State 1975 to 2025. Sociology, Vol. 34, No.1, pp. 129-146.
Kanter, R.M. (1993) Men and Women of the Corporation, 2nd edn. New York: Basic Books.
Kieran, W. & Rundall, T. 2001. Evidence-based Management: From Theory to Practice in Health Care. The Milbank Quarterly, Vol. 79, Issue 3, pp. 429-457.
Laschinger, H. & Shamian, J. 1994. Staff nurses’ and nurse managers’ perceptions of job related empowerment and managerial self efficacy. Journal of Nursing Administration, Vol. 24, No. 10, pp. 38–47.
Leatt, P. 1994. Canadian physicians in health care management: Physicians as Managers, roles and future challenges. Canada Medical Association Journal, Vol. 150, No. 2, pp. 171-176.
Llewellyn, S. 2001. Two way windows: clinicians as medical managers. Organisational Studies, Vol. 22, No. 4, pp. 593-623.
Marshall, M. 2003. Trends in doctor-manager relationships. British Medical Journal, Vol. 326, pp. 646-649.
Martin, J., 1992, Cultures in Organizations: Three Perspectives. New York: USA Oxford University Press,
Mintzberg, H. 1994. Managing as blended care. Journal of Nursing Administration, Vol. 24, pp. 29–36.
Mintzberg, H. 1997. Managing as blended care. Journal of Nursing Administration, Vol. 24, pp. 29–36.
Mintzberg, H. I982 Covert leadership: notes on managing professionals. Harvard Business Review, Vol. 76, No.6, pp.140–147.
Mintzberg, H., 1973, The Nature of managerial work. New York: Harper and Row.
National Health Service. The NHS in England. Web.
NHS England. The NHS in England. Web.
Nowak, D. 2006. Doctors on Strike — The Crisis in GermanHealth Care Delivery. New England Journal of Medicine, Vol. 355, No. 15, pp. 1520-1522.
Persson, O. & Thylefors, I. 1999. Career with no return: roles, demands, and challenges as perceived by Swedish ward managers. Nursing Administration Quarterly, Vol. 23, No.3, pp. 63–80.
Saarikoski, M., Leino-Kilpi, H. 2002. The clinical learning environment and supervision by staff nurses: developing the instrument. International Journal of Nursing Studies. Vol. 39, Issue 3, pp.259–267.
Sackett, D., & Rosenberg, W. 1995. The Need for Evidence-based Medicine. Journal of the Royal Society of Medicine, vol. 88, No. 11, pp. 620–4.
Sanders, B., Davidson, A. & Price, S. 1996. The unit nurse executive: a changing perspective. Nursing Management, Vol.27, pp. 42–45.
Sausman, C. 2001. New roles and responsibilities of NHS chief executives in relation to quality and clinical governance. Quality Health Care, Vol. 10(Suppl 2), pp. 13–20.
Scarbrough, H. & Burrell, G., 1996, The Axe man Cometh: the changing role and knowledge of middle managers’, in S. Clegg and G. Palmer (eds) The Politics of Management Knowledge. Thousand Oaks, CA: Sage.
Schneller, E.S. 1991. The leadership and executive potential of physicians in an era of managed care systems. Hospital Health Service Administration, Vol. 36, No. 1, pp. 43-55.
Shortell, S. & Kaluzny, D.1994. Health care management: Organisational design and behaviour. Albany, NY: Delmar.
Shortell, S., Morrison E. & Friedman B. 1990. Strategic Choices for America’s Hospitals: Managing Change in Turbulent Times. San Francisco, CA: Jossey-Bass.
Skytt, B., Ljunggren, B., Per-Olow, S. & Carlsson, M. 2008. The roles of the first-line nurse manager: perceptions from four perspectives. Journal of Nursing Management, Vol. 16, pp. 1012–1020.
Smith, J. & Preston, J. 1996. Communications between professional groups in an NHS trust hospital. Journal of Management in Medicine, Vol. 10, Iss: 2, pp.31 – 39.
Strathem, J. 1994. (in Du Plat-Jones, J. 1999) Power and representation in nursing: a literature review. Nursing Standard, Vol.13 is 49), 39–42.
Surgeon, K. 2000. Managing in a Professional Bureaucracy. International Journal of Health Care Quality Assurance, Vol. 3, Iss. 2, pp. 1978-80.
Thomas, R. & Dunkerley, D. 1999. ‘Careering Downwards? Middle Managers’ Experiences in the Downsized Organization. British Journal of Management, Vol. 10, pp. 157–169.
Thorne, M. 2002. Colonizing the new world of NHS management: the shifting power of professionals. Health Services Management Research, Vol. 15, No. 1, pp. 14-26.
Thorne, M. 2000. Cultural chameleons. British Journal of Management, Vol. 11, No. 4, pp. 325–339.
Upenieks, V. 2003. Nurse leaders’ perceptions of what comprises successful leadership in today’s acute care environment. Nursing Administration Quarterly, Vol. 27, pp. 140–152.
Vastola, P, & Tosolini, G. 2005. Quality improvement, training and clinical governance: the role of the chief medical officer and his staff. Sanita Publications, Vol. 61, No. 2, pp. 213-33.
Walshe, K. & Rundall, T. 2001. Evidenced-based management: from theory to practice in healthcare. The Milbank Quarterly, Vol. 79, No. 3, pp. 429-457.
Warwicker T. 1998. Managerialism and the British GP: the GP as manager and as managed. St Mary’s Wing, Whittington Hospital, Middlesex University, London, UK. Journal of Management in Medicine, Vol. 12, No. 6, pp. 331-48.
Weiner, J., Shortell, M. & Alexander, J. 1997. Promoting clinical involvement in hospital quality improvement efforts: the effects of top management, board, and physician leadership. Health Service Reserve, Vol. 32, No. 4, pp. 491–510.
Whittington, R., Mcnulty, T. and Whipp, R., 1994, ‘Market Driven Change in Professional Services: Problems and Processes’, Journal of Management Studies, 31(6): 829–45.
Willcocks, S., 1994, The Clinical Director in the NHS: Utilizing a Role-theory Perspective. Journal of Management in Medicine, Vol. 8, Iss. 5, pp.68 – 76.
Williams, L. & McMurray, A. 2003. Factors affecting the innovative practice of nurse managers in health organisations. Contemporary Nurse, Vol. 16, No. 1–2, pp. 30–39
Williams, A., McGee, P., & Bates, L. 2001. An examination of senior nursing roles: challenges for the NHS. Journal of Clinical Nursing, Vol. 10, No. 2, pp. 195-203.
Willmot, M. 1998. The new ward manager: an evaluation of the changing role of the charge nurse. Journal of Advanced Nursing, Vol. 28, pp. 419–27.
Witz, A., 1994, ‘The Challenge of Nursing’, in J. Gabe, D. Kelleher and G. Williams (eds) Challenging Medicine, pp. 23–45. London: Routledge.
Wooldridge, B. & Floyd, S. W. 1990. The strategy process, middle management involvement, and organizational performance. Strategic Management Journal, Vol. 11, pp. 231–41.
Yin, R. 2009. Case Study Research: Design and Methods. California: Sage Publications.
.