The quality of patient care and its outcomes in the system of healthcare depends on the application of evidence. There exist diverse possibilities to implement evidence in health care. It can positively influence both health care delivery and the health of the population (Titler, 2014). There is a need for strategies that can link research and practice and thus “realize and maximize the benefits of research through improved health outcomes, better health services, and products, strengthened healthcare systems, and more effective health service delivery (Scott et al., 2012, p. 2). This area of study is known as knowledge translation. Its major purpose is to bring together research and practice (Scott et al., 2012). The implementation of knowledge translation is supposed to stimulate professional, financial, organizational, and regulatory interventions. It is expected to influence healthcare professional behavior which includes changes in decision making, treatment, and management (Scott et al., 2012). Translation science cab is defined as “the investigation of methods, interventions, and variables that influence adoption by individuals and organizations of EBPs to improve clinical and operational decision making in health care” (Titler, 2008, p. 3).
Titler (2008) claims that there is a variety of evidence-based practice models. She also states that translation science needs guidance by one of the conceptual models which have an impact on the perception of evidence-based practices. The Agency for Healthcare Research and Quality (AHRQ) funded some translating-research-into-practice studies which included such conceptual models as “adult learning, health education, social influence, marketing, and organizational and behavior theories” (Titler, 2008, p. 3). One of the primary purposes of translation of evidence into practice is the improvement of clinical outcomes.
Translation of Evidence to Improve Clinical Outcomes
Description
Knowledge translation is treated as the process of creation of research knowledge, its circulation, and adoption into clinical practice (Curtis, Fry, Shaban, & Considine, 2016). It is expected to contribute to the positive changes in the health care service and thus the improvement of patients’ clinical outcomes. According to the Joint Commission (as cited in White & Dudley-Brown, 2012, p. 61), “patient outcomes management and the application of evidence to practice are powerful tools that can improve quality of care.” The desired patient outcomes determine the organization of care and demand constant improvement of intervention strategies and the application of innovative techniques. Institute of Medicine defines quality (as cited in White & Dudley-Brown, 2012, p. 61) as the “degree to which health services for individuals and populations increase the likelihood of attaining desired health outcomes and are consistent with current professional knowledge.” Patient safety is one of the quality constituents. It is important to evaluate the possible care outcomes not in isolation but as related to the care interventions.
Heater, Becker, and Olson (as cited in White & Dudley-Brown, 2012, p. 65) admit that research findings reveal the influence of research-based nursing practice on patient outcomes. Research based on a meta-analysis evaluated the impact of the research-based nursing practice on patient outcomes if compared to usual nursing care. The analysis compared eighty-four studies, both published and unpublished. The independent nursing interventions were assessed and their outcomes were divided into areas of influence. They included behavioral, knowledge, physiological, and psychosocial outcomes (White & Dudley-Brown, 2012). The research resulted proved that “patients who received research-based nursing care had better outcomes than 72% of subjects who received routine, procedural nursing care” (White & Dudley-Brown, 2012, p. 66). However, evidence-based practices are not frequently integrated into the process of care by health care providers. During recent decades, there were attempts to bring the empiric knowledge obtained from the research results to practice and to narrow the gap between practice and theory inpatient care. Thus, among the first experiences of the evidence-based approach to care application was the development “of consistent expectations for the performance of cardiopulmonary resuscitation (CPR)” in the 1970s (White & Dudley-Brown, 2012, p. 66). These standards were aimed to empower training and testing the competency of health care providers. The limited research data on CPR together with the expert opinion became the basis for these standards. This intervention stimulated the development of similar standards in other fields (White & Dudley-Brown, 2012). They were helpful for nursing practice because they provided certain procedures applicable in this situation grounded on the research findings.
Even though there is a necessity to translate knowledge, not all research findings are translatable (Pearson, Jordan, & Munn, 2012). For example, Gravel et al. (as cited in Pearson, Jordan, & Munn, 2012, p. 4) single out some gaps which are obstacles to the successful translation of knowledge into the practice. Their obstacles include “the increasing volume of research evidence being produced, access to new evidence, the skills to appraise the quality of the evidence, time to locate and read the evidence, and the capacity to apply evidence (Pearson, Jordan, & Munn, 2012, p. 4) 2006). Knowledge translation can be treated as the process from initial discovery to the development of the intervention. Pearson, Jordan, & Munn (2012) distinguish three major gaps in translating research knowledge to practical implementation aimed at the improvement of patient outcomes and health care services (See Figure 1).
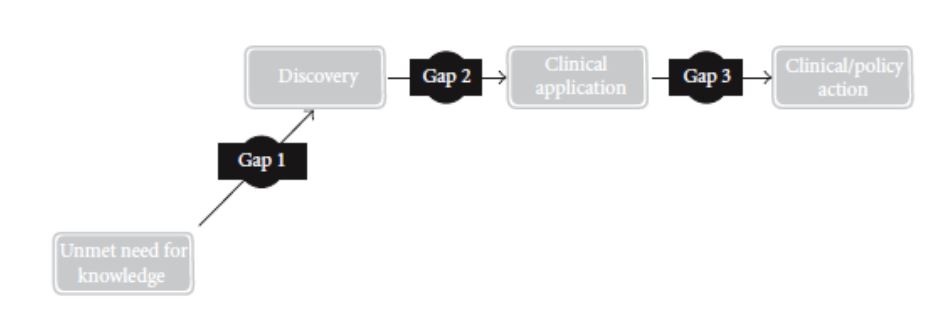
- Gap 1: From Knowledge Need to Discovery. It is related to the gap between “knowledge needs” (according to the opinions of patients, community, clinicians, etc.), and the actions provided by scholars and researchers. ring the “discovery” process. Within this gap, it is advisable to select the topic which will stimulate “active collaboration between those conducting the research and the end-users of research (clinicians, patients, community) (Pearson, Jordan, & Munn, 2012, p. 4).
- Gap 2: From Discovery to Clinical Application. This gap deals with discrepancies between “discovery research” and “clinical research.” This gap receives the most attention both on national and international levels. Nevertheless, such attention does not resolve the problem.
- Gap 3: From Clinical Application to Action. This gap is not widely addressed by researchers (Pearson, Jordan, & Munn, 2012). However, some programs aimed to bridge this gap appeared in cardiology and metabolic/human nutrition centers (Pearson, Jordan, & Munn, 2012). On the whole, despite the variety of models, there is no accepted universal approach to knowledge translation. The three gaps exist regardless of the model and include “(1) the gap between the need for knowledge and the discovery of that new knowledge; (2) the gap between the discovery of new knowledge and the clinical application of that knowledge; (3) the gap between the clinical application and the development of routine clinical actions or policy” (Pearson, Jordan, & Munn, 2012, 4). The practice of science translation should be aimed at the elimination of these gaps.
Presentation of Translation of Evidence to Improve Clinical Outcomes
Translating research into practice as science developed from the descriptive studies which revealed the gaps “between what is known to be effective health care practices and the actual practices that patients receive” (Titler, 2004, p. 38). Thus, there is a big gap between the health care people get and the care they could get. Titler (2004) suggests the definition of translation of research as “the scientific investigation of methods and variables that affect the adoption of evidence-based health care practices by individual practitioners and health care systems to improve clinical and operational decision making” (p. 38). Thus, the impact of care interventions should be assessed and combined with evidence-based practices.
The international scientific community is concerned with the gaps between the research knowledge and their practical implementation. For example, in the United States, many projects were initiated to bridge the gaps between research and practice (Titler, 2004). They are supposed to focus on the significance of “linking nurse scientists in academic settings with nurses in practice to foster the use of research findings to guide nursing care decisions” (Titler, 2004, p. 39). The results of those projects proved the opportunities to change nursing practices from tradition-based to evidence-based. This fact should also stimulate health care providers to apply research findings in the everyday practice of patient care. Some strategies which are applied to promote the use of evidence-based practices were not tested properly. This fact, of course, makes their application more complicated and less efficient.
Curtis et al. (2016) state that the possibility of translation of research findings should be taken into account already in the study design. The aims of the research should also consider such possibilities. In case the researcher predicts opportunities for translation of research findings into clinical practice, these results will be more available for translation. However, the success of knowledge translation does not only depend on the researcher and the nurse or clinical practitioner. Senior clinician’s support is crucial for such initiatives (Curtis et al., 2016). The policy of administration can be stimulating for the implementation of new approaches in the improvement of patient outcomes.
One of the experiences of implementing evidence-based practice is provided by the National Nursing Practice Network (Titler, 2014). It allows its participants to access various resources and conducts online learning on the issue of evidence-based practice. Due to the network, clinicians have an opportunity to share their experience of evidence-based practice interventions. The network includes hospitals, health systems, universities, and schools of nursing (Titler, 2014). Such a collaborative nursing network allows using novice approaches to care and facing challenges of implementing evidence-based practices and science translation. Moreover, it is a source for collaborative projects within the network.
Conclusions
On the whole, the issue of translation science is a complex one. The necessity of using research findings in the practice of nursing care has been proved. However, few types of research provide distinct algorithms for the process of translation. No doubt, there is no unified approach to translating science to practice. The approach to research knowledge translation depends on the type of research (theoretical or practical, qualitative or quantitative, etc.) and the field in health care where it will be applied. Translation science interventions have different purposes. One of the main aims is the improvement of clinical outcomes. Research provides practice with the assessment of care interventions. It allows selecting the most efficient care models and intervention strategies to provide better patient outcomes. Thus, practical care can benefit from the translation of scientific knowledge providing patients with a higher level of care.
References
Curtis, K., Fry, M., Shaban, R.Z., & Considine, J. (2016). Translating research findings to clinical research practice. Journal of Clinical Nursing, 26, 826-872. Web.
Pearson, A., Jordan, Z., & Munn, Z. (2012). Translational science and evidence-based healthcare: A clarification and reconceptualization of how knowledge is generated and used in healthcare. Nursing Research and Practice, 1-6. Web.
Scott, S.D., Albrecht, L., O’Leary, K., Ball, G.D.C., Hartling, L., Hofmeyer, A. … Dryden, D.M. (2012). Systematic review of knowledge translation strategies in the allied health professions. Implementation Science, 7:70.
Titler, M.G. (2004). Methods in translation science. Worldviews on Evidence-Based Nursing, 38-48.
Titler, M.G. (2008). Chapter 7. The evidence for evidence-based practice. In R.G. Huges (Ed.). Patient safety and quality: An evidence-based handbook for nurses (pp. 1-49). Rockville, MD: Agency for Healthcare Research and Quality.
Titler, M.G. (2014). Overview of evidence-based and translation science. Nursing Clinics, 49(3), 269-274. Web.
White, K.M., & Dudley-Brown, S. (2012). Translation of evidence into nursing and health care practice. New York, NY: Springer Publishing Company.