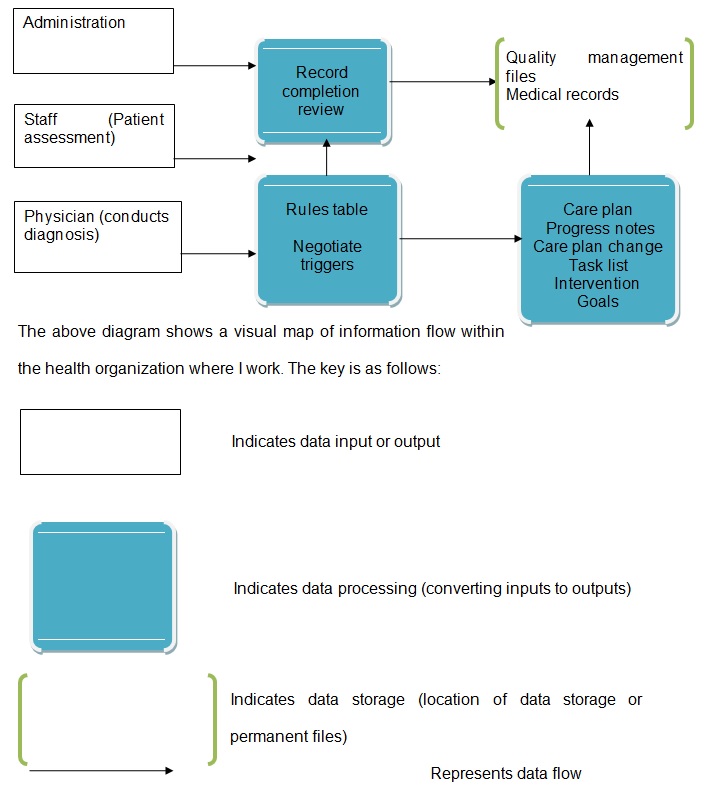
Visual Map
I work in a level one trauma center where bullets and gunshots are the diagnosis codes. The healthcare organization uses a HIT system that helps to coordinate the sharing and usage of healthcare data across departments. Healthcare technology is aimed to improve the quality of healthcare offered to patients by healthcare professionals within the organization (Buntin, Burke, Hoaglin & Blumenthal, 2011; Hersh, 2004). The types of information supported by the HIT system include the following: patients’ names, laboratory support, medical history, health condition, gender, and/or occupation, among other pieces of data. Clinical information that is stored in the database of the system helps the healthcare organization personnel to define the types of documented and delivered care.
Alerts and triggers are analyzed to determine their frequency and clinical importance within the organization. Alerts and triggers with more positive clinical outcomes are used to improve the quality of healthcare and risk management (Alexander, 2008). An alert within the healthcare organization is defined as a predetermined clinical decision that is vital in sending messages to the end-users. Therefore, an alert is an automated message. An alert could have the following clinical parameters: dehydration, weight loss, skin integrity, bleeding, and weight gain. A trigger is a logic that produces an alert that is delivered to healthcare professionals as a warning. The warning informs healthcare personnel that a patient could be developing a potential clinical problem. A trigger contains a collection of clinical rules that healthcare professionals use to conduct clinical assessments. When using a visual map to illustrate information flow within an organization, it is important to identify the origin and final destination of the information (Alexander, 2008; Buntin et al., 2011).
Laboratory results in information flow within the organization
A new patient with gunshots and/or bullet wounds is assessed by the staff on duty to record basic information like medical history, name, residence, and symptoms. The patient is then sent to a physician for medical diagnosis. However, the physician cannot offer a definitive diagnosis without laboratory results. Therefore, the patient would be sent to the laboratory department for laboratory tests as ordered by the physician. Laboratory technologists would collect a biological sample from the patient and carry out tests. The laboratory results are transmitted along with the HIT system to the physician for interpretation. The physician would diagnose the patient based on the laboratory results received from the laboratory department. The laboratory diagnosis data are processed to triggers within the processing component of the visual map (the rules table). The triggers are used to send laboratory results alerts to nurses and other professionals who develop progress notes and care plans for the patient. In addition, clinical alerts are used to develop goals, interventions, and care plans for the patient. The patient’s laboratory results are transmitted to electronic medical files (in the form of a database) where the information is stored for retrieval by authorized healthcare personnel in the future. The laboratory results are also transmitted to quality management files that are used by the quality department to assess, evaluate and improve the quality of patients’ care within the healthcare organization.
References
Alexander, G. L. (2008). A descriptive analysis of a nursing home clinical information system with decision support. Perspectives in health information management, 5(1), 1-20.
Buntin, M. B., Burke, M. F., Hoaglin, M. C., & Blumenthal, D. (2011). The benefits of health information technology: a review of the recent literature shows predominantly positive results. Health Affairs, 30(3), 464-471.
Hersh, W. (2004). Health care information technology. JAMA: the journal of the American Medical Association, 292(18), 2273-2274.