Introduction
Based on the World Health Organization (1996) definition, palliative care is the active care of patients afflicted with a chronic disease that will ultimately lead to their death. Palliative care focuses on the management of pain, other symptoms, psychological, spiritual, and social crisis. Thus, the objective of palliative care is to attain an optimal quality of life for patients as well as their families. Moreover, palliative care support can extend to the period of bereavement (Agarwal & Raamamoorthy, 2005).
According to the National Institute of Nursing Research (2009), the management of the symptoms of painful fatal illness is challenging. The prominent purpose of palliative care is pain management. Therefore, palliative care is the mainstay for the management of life-threatening diseases. Besides pain management, palliative care also helps to alleviate suffering due to other symptoms such as sleep disorder, loss of appetite, nausea, constipation, fatigue, and shortness of breath among others.
Nevertheless, because palliative care organizations seldom attain optimal pain management, rigorous research needs to be conducted to ascertain the elements which affect the provision of quality palliative care concerning pain management. This paper seeks to explore the enablers at the same time barriers to pain assessment and management in order to facilitate best quality care.
Essentially, this paper will focus on pain management as the central responsibility of palliative care service delivery. I will examine the various aspect of pain management to ascertain how they contribute to the quality of care delivery. These aspects include the patient, the service providers, and the environment within which care is provided.
Pain relief as the central focus for palliative care
Pain refers to an undesirable sensory and emotional experience related to tissue damage. Pain can be classified into acute or chronic pain depending on the duration of the experience. Acute pain refers to pain that lasts for moments or hours including those that last for weeks or few months, until the illness or the damage is cured (Bonica, 1990 cited in ICSI, 2010). Chronic pain on the other hand is a continuous or recurrent pain of intense magnitude which jeopardizes an individual’s well-being (Wisconsin Medical Society Task Force on Pain Management, 2004).
Pain can be attributed to malignancies, opportunistic infection, or complications. In the course of disease process, patients experience fluctuating levels of pain because of the various causes which will necessitate relief intervention in primary care or home care.
Pain assessment algorithm
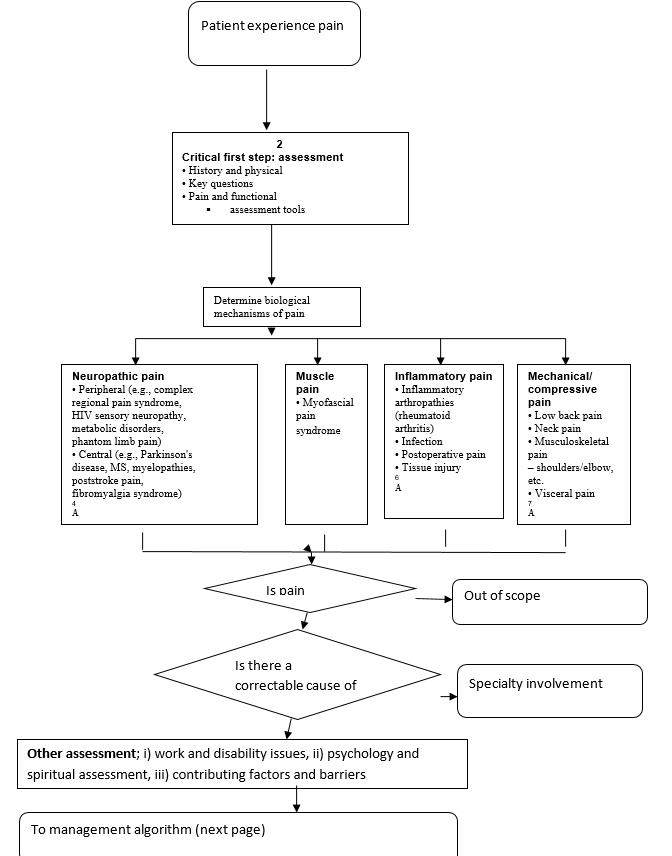
Pain assessment involves various processes and tools. First, it involves screening all persons susceptible to pain once, daily, by inquiring from the individual or family about the existence of pain, or any other form of discomfort. Another process involves the use of standard devices to determine the parameters of pain including location, influence of pain on function and routine, the various level of pain during rest and as well as activity. Also, the other parameters that are assessed are the provoking factors and quality of pain (Registered Nurses Association of Ontario, 2002).
Barriers to pain treatment
Despite the existence of a wide variety of pain management drugs, only 50% of pain control is provided for cancer patients (World Health Organization, 1996). According to the International Association For The Study The Study Of Pain (2009), barriers to adequate pain management in palliative care can be categorized into problems attributed to the various elements of pain management including and to health care delivery system, professionals, and patients.
Challenges attributed to the medical care professionals
Bruera, Willey, Ewert-Flannagan, Cline, Kaur, Shen, et al. (2005), argue that inaccurate evaluation of pain and insufficient knowledge on the side of the clinicians contributes greatly towards the undermining of pain treatment in cancer patients. Physicians and nurses make judgment that primarily determines cancer pain treatment, and development in their patient pain evaluation may lead to appropriate analgesics prescription and subsequently lead to improved pain management (Cleeland , Cleeland, Dar, & Rinehardt, 1986).
Anxieties concerning the restrictions of prohibited substances, adverse effects of analgesics, and patients’ tolerance or addictions to analgesics have also been noted to hinder effective cancer pain management. Therefore, improved training in cancer pain treatment at the various levels of professional learning is recommended (IASP, 2009).
According to Pargeon and Hailey (1999), nurses and physicians are also a source of barriers to ineffective pain management of patients. This normally occurs if such professionals are deficient in terms of the knowledge needed to manage pain. In addition, this could also be a result of misconceptions regarding the side effects and effects of medication. Moreover, health care professionals that are deficient in the assessment procedures of pain could also end up delivering insufficient pain management.
Sun et al (2007) argue that insufficient knowledge regarding the management of pain by health care professionals could also result in poor communication with the other members of the team involved in the pain management exercise within the health care system. Misconceptions by health care professionals regarding the management of pain may also hinder the desire by the patient to assess pain management services. Moreover, Jacobsen et al (2008) further assert that the healthcare professionals might also have misconceptions about the pharmacological effects of the drugs available to facilitate the management of pain.
Challenges attributed to the patients
A patient’s attitude towards the care providers contributes a lot to the success of pain management. For instance, they may not want to complain of pain since they want to forge the impression that they are “good” patients or they may not wish to deviate the physician’s attention from managing the primary disease (IASP, 2009).
(Hodes, 1989) claim that in certain circumstances the patient may perceive pain as an unavoidable aspect of cancer proliferation, and they may not want to accept that their abnormality is progressing. Also, according to (Jones, Rimer, Levy, & Kinman, 1984.) anxiety by patients concerning early pain management will hinder future pain control because they may develop tolerance. Frequently, patients may loathe taking pain prescriptions while others fear developing dependence on the analgesic (Anderson, Richman, Hurley, Palos, Valero, Mendoza et al., 2002). The patient may develop worries of unmanageable adverse effects leading to poor conformity to prescription regimen.
Challenges attributed to the health care delivery system
A strict regulatory working environment that pressures physicians concerning their prescribing habits further accounts for shallow management of cancer patients. Restrictive regulation of prohibited substances coupled with scarcity of treatment may amount to obstacles to patient’s management. According to the findings of a study of Wisconsin physicians, because of concerns of regulatory inspection, the majority of the respondents decreased the prescription regimen or indicated an inferior drug for patient management (IASP, 2009).
Moreover, cancer pain management is given low priority in the health care delivery system and in the training program for medical professionals. Most health and nursing textbooks allocate just a few pages to modern pain and symptom management procedure (IASP, 2009). Also, health policy matters relevant to pain such as ethical and legal matters, regulatory aspects, care accessibility, and cost have similarly been undermined (IASP, 2009).
When an individual is not in a position to adequately access health resources meant to facilitate the managing of pain, this could as well hinder efforts to control the pain (Kazanowski & Lacetti, 2002). It is important that patients gain access to health care services so that they cannot only get information on how best to manage their pain through educational forums, consultations and referrals, but also by actually having their pain managed.
Environment
The important role played by the environment in as far as the issue of effective management of pain is concerned cannot be overstated. In this case, environmental factors include among others cultural and social contexts of the place where the pain is taking place. In this case, the physical environment may take the form of long-term care. On the other hand, the social support that the ensuing interpersonal relationship that the individuals in need of pain management enjoy, entails the social environment. Moreover, beliefs, personal values and practices as impacted by religion, ethnicity and care constitute the cultural environment (Jacobsen et al., 2008).
The health care provider must provide an environment that is quiet and serene at a time when they are assessing the pain of a patient. Such factors as noise, privacy invasions could make the patient quite uncomfortable, in effect interfering with the process of pain assessment. This could also result in the poor assessment of the causes of the pain (Kazanowski & Lacetti, 2002).
Collaboration at the organizational level
For purpose of ensuring that patients under pain management care get high-quality treatment as they approach the end of their life stage, there is the need to ensure that collaboration is cultivated among the various organizations involved. As Pargeon and Hailey (1999) have noted, it is important to audit the education of peers, patients, as well as the professionals, and the necessary feedback obtained. In addition, we now have different organizations that have been established with a view to ensuring that the pain relief services that are accessible to the patients are effective. Examples here include Chronic Pain Management Services, Cancer Pain Management services, Acute Pain Teams, as well as the Palliative Care Organizations, among others (Buckley, 2008).
Organizational barriers often entail rules and regulations that underlie the health care system under which the pain management initiative is being undertaken. The management of pain could for example be hindered by authority regulations seeking to control the procedures, policies and guidelines of treatment (Carr, 2008). Another good example is uncalled for policies within health care system that could result in holdups in opioid administration to patients experiencing severe pain.
Enablers to effective pain assessment and pain management
Sun et al (2007) argue that rigorous research needs to be conducted to ascertain the elements which favor or which do not favor pain management in palliative care. This has necessitated the adaptation of evidence-based approach to palliative care delivery, exemplified by the Cochrane Collaboration, which has been accompanied switch of focus to patient-centered health results. This extended point of view has augmented the necessity for tools to monitor and regulate pain management and to advance clinical decision making from an outcome basis of and patient-centered. This is paramount in a patient afflicted with a lethal disease (Macintyre, Schug, Acott, Visser, & Walker, 2010).
Clearly, in the course of improving the quality of life of patients in their terminal phase of disease it is prominent for the service providers to focus on the elements that are proposed to be in alignment with the objective of the palliative care provider at the same time with the expectation of the patient. These elements include education; patient-based medical results (Macintyreet al., 2010). Additionally, Sun et al., (2007) argue that it is more appropriate to recognize the obstacles that impede effective pain relief so that accurate diagnosis can be established.
Education
If both the patient and the care providers are conversant with the management goals, chances of success, side effects, likely risks, and benefits, it will lead to positive attitude and that will help in pain management. Care instructors should give information via booklets, one on one teaching methods as well as video (Macintyre et al., 2010). Eventually, all the above mention techniques can help in decreasing some of the challenges that impede quality care delivery in the form of pain treatment. Progressive education of the providers may encompass the provision of the most efficient protocols of analgesics prescription founded on outcome-based research.
Further Macintyre et al (2010) argue that education should not only target the patient but also should cover the health care providers such as the nurses, physicians, and other members of the workforce. Besides, staff education should emphasize teaching safe and efficient analgesic prescriptions.
Organization and teamwork
To achieve the best quality care delivery with regard to pain management collaboration amongst the staff should be boosted. According to Pargeon and Hailey (1999), intensive patient and specialist education, as well as peer audit and outcome, should be highly implemented. As a matter of fact, numerous organizations have been established to provide safe and efficient pain management services and implement the models described above. Such organization comprises Acute Pain Teams (APTs), Primary Care Teams, cancer Pain Management Services, Palliative care organizations, and Chronic Pain Management Services (Buckley, 2008).
The organizational obstacles encompass rules and regulations of medical care system the within the health care institution. For instance, ineffective pain treatment can be attributed to the authority board which regulated the treatment rules, processes and protocols (Carr, 2008). Some inappropriate policies that may delay opioid administration to patients with intense pain portray best how organizational protocols can adversely influence the pain treatment process.
Role of nurses in palliative care
Nurses play a significant role in the palliative care provision for terminally sick patients. Nurses use most of their time attending to terminally sick patients. It is paramount for the nurses to know the standards and protocols of cancer pain treatment set by the World Health Organization, including the analgesic ladder. According to Brown (2004), nurses can assume diversified roles when attending to patients in palliative care. These responsibilities range from being the patient’s educator, advocate, and consultant. It is a prerequisite that a nurse should be equipped with good communication skills to enable him/her to ease the patient’s anxiety related to diagnosis, prescription regimen, and extra factors. Moreover, by being interdisciplinary in regard to care delivery, nurses should act on patient’s behalf to ensure availability of care services to the patient (Middleton-Green, 2008; & Munden et al., 2003).
Conclusion
Pain adversely influences the lives of many people by making it unbearable. Thus, it is the duty of every medical practitioner, particularly those who work in palliative care organizations to determine the factors that impede the delivery of the best quality pain management. Top-quality palliative care management can be attained if thorough health assessment protocols to identify cases of pain are applied. The assessment of pain should seek to identify and overcome the three major factors that have been identified to challenge effective pain management.
In order to improve the quality of life of terminally-ill patients, sufficient knowledge needs to be gathered by conducting rigorous research to allow formulation of evidence-based strategies that fit particular circumstances to overcome the barriers to best quality pain management. Since the nurses are key players in pain management, the health institution should invest a lot in uplifting the knowledge of the nurses, so that they would be equipped with skills to tackle such problems in the future.
Reference List
Agarawal, S. P. & Raamamoorthy, K. (2005). Manual for palliative care. Directorate general of health services ministry of health and family welfare government of India. p. 6.
Anderson, K. O., Richman, S. P., Hurley, J., Palos, G., Valero, V., Mendoza, T. R., Gning, I., & Cleeland, C. S. (2002). Cancer pain management among underserved minority outpatients: perceived needs and barriers to optimal control. Cancer, 94:2295–304.
Bruera, E., Willey, J. S., Ewert-Flannagan, P. A., Cline, M. K., Kaur, G., Shen, L., Zhang, T., Cleeland, C. S., Cleeland, L. M., Dar, R., & Rinehardt, L. C. (1986). Factors influencing physician management of cancer pain. Cancer, 58:796–800.
Buckley, J. (2008). Palliative care: An integrated approach. United Kingdom: Wiley Blackwell.
Carr, E. (2008). Barriers to effective pain management. Journal of Preoperative Practice, 17(1), 45-63.
Hodes, R. (1989). Cancer patients’ needs and concerns when using narcotic analgesics. In: Hill CS, Fields WS, editors. Drug treatment of cancer pain in a drug-oriented society.New York: Raven Press.
IASP. (2010). IASP pain terminology. Web.
Institute for Clinical Systems Improvement. (2009). Assessment and management of chronic pain: scope and target population. New York: Wiley.
Jacobsen, R., Møldrup, C., Christrup, L., & Sjøgren, P. (2008). Patient-related barriers to cancer pain management: A systematic exploratory review. Scandinavian Journal of Caring Sciences 23(1), 190–208.
Jones, W., Rimer, B., Levy, M., & Kinman, J. (1984). Cancer patients’ knowledge, beliefs, and behavior regarding pain control regimens: implications for education programs. Patient Educ Couns, 5:159–64.
Kazanowski, M. K., & Lacetti, M. S. (2002). Pain. New Jersey: Slack.
Macintyre P. E., Schug S. A., Acott D. A., Visser, E. J., & Walker S. M. (2010). Working group of the Australian and New Zealand College of Anaethetists and Faculty of Pain Medicine. Acute Pain Management: Scientific Evidence (3rd ed.), ANZACA & FPM, Melbourne.
Middleton-Green, L. (2008). Managing total pain at the end of life: a case study analysis. Nursing Standard, 23(6), 41-47.
National Institute of Nursing Research. (2009). Palliative care: the relief you need when you’re experiencing the symptoms of serious illness. U.S. department of health and human services; National Institute of Health. Maryland; NIH publishers.
Pargeon, K. L., & Hailey, B. J. (1999). Barriers to effective cancer pain management: A review of the literature. Journal of Pain and Symptom Management, 18(5), 358-368.
Registered Nurses Association of Ontario. (2002). Nursing best practice guideline: assessment management of pain. Ontario: Sage.
Sun, V. C.-Y, V., Borneman, T., Ferrell, B., Piper, B., Koczywas, M., & Choi, K. (2007). Overcoming barriers to cancer pain management: An Institutional Change Model. Journal of Pain and Symptom Management, 34(4), 359-369.
Wisconsin Medical Society Task Force on Pain Management. (2004). Guidelines for the assessment and management of chronic pain. BMJ, 103:15-43.
World Health Organization. (1996). Cancer pain relief and palliative care, 2nd ed. Geneva: World Health Organization.