Healthcare organizations occasionally experience errors due to individual problems of the medical team, system factors, or policies. Having a prompt medical error report system can help in mitigating the consequences. Thus, instead of blaming, it is better to use the root-cause analysis (RCA), establish the factors and timing of the mistake, and invent preventive strategies. Gathering and analyzing information and then visually representing it in a flow, chat helps in the continuous enhancement of patient-centered care. Moreover, the RCA approach expands accountability to everyone while encouraging teamwork and effective communication.
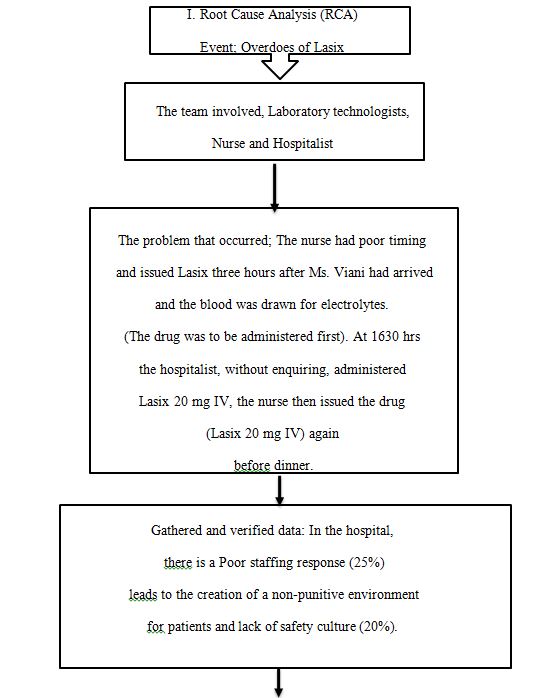
Root Cause Analysis
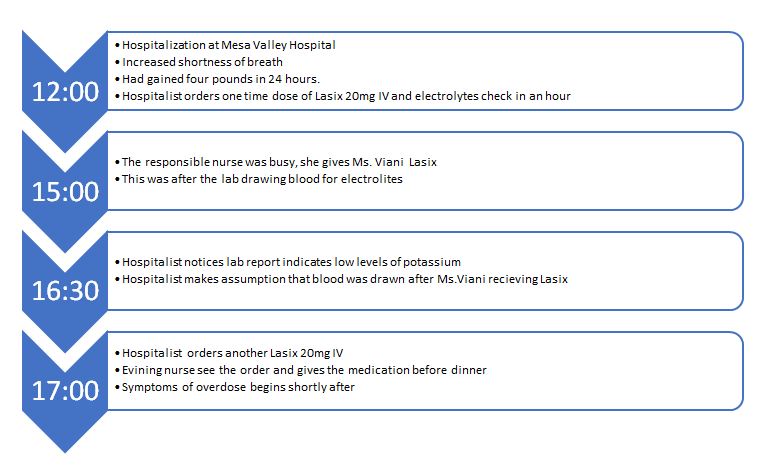
Time line Analysis
Factors
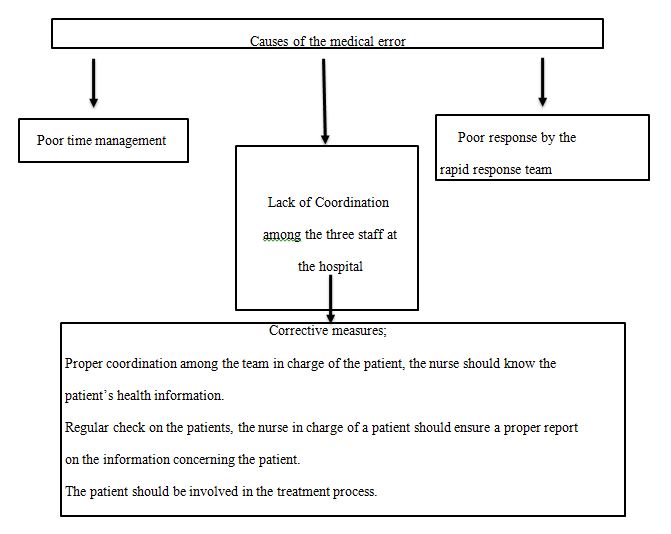
The contributing factors are directly related to humans and include poor organization, fatigue, and distractions. The drug overdose occurred due to poor teamwork and communication between the hospitalist, laboratory technician, responsible nurse, and the evening nurse. The four were working on the same patient, but they constantly failed to tell each or report about the development of the case. For example, the hospitalist had already given Ms. Viani Lasix but failed to inform the responsible nurse. Moreover, instead of confirming, the hospitalist makes a critical decision based on assumption. For example, after noticing that the laboratory report indicates that the patient has low potassium levels, she thinks that the test was taken before medication and proceeds to give another dose. Thus, the organization was poor and compounded by an ineffective transition between the staff.
Causative
The main causative factor is the high workload which makes the staff barely find time to concentrate on one patient. A good illustration is when Ms.Viani gets to the hospital, the responsible nurse is busy and cannot attend to her. Furthermore, a small number of staff is expected to serve many patients, causing sluggishness and shortcuts. For example, the response after Ms.Viani started showing symptoms of overdose was slow because people were attending other patients. The policy of faulting the hospitalist is punitive and may further discourage the healthcare team. Since system factors contributed to the error, it was not right to make the hospitalist face full liability for the mistake made by several people.
Patient and Family
The medical staff failed to involve the patient in the treatment process even though she was conscious and of sound mind. While the hospitalist, nurse in charge, and evening nurse were giving orders for medication, they did not consult to check if she had any allergies and confirm the services she had already received. Moreover, the patient was unaccompanied by any relative or friend at the hospital. Even after her admission to the inpatient service, the staff did not bother to ask for their accompanying relative. Perhaps if the nurse told the patient about the drug, she would remember to inform the next medic. Alternatively, if their significant other were present, they would have asked questions about what their patient was given.
Evidence-Based Patient Safety Improvement Strategies
The RCA helps in identifying mistakes and adopting better patient-centered safety strategies. An evidence-based approach that has been verified to be effective for an etiopathogenesis of a specific condition is vital (Donaldson et al., 2020). In addition, the formula of plan-do-study-act (PDSA) cycles is proven to enhance the quality of care in healthcare organizations. In this case, the RCA reveals human and systematic factors that the nurse leader should address to avoid future mistakes. The team should discuss strategies to make them more effective in their work. For example, they may develop a handling report where each professional writes and signs what they have done to the patient. After implementation, they have to study through evaluation and assessment to determine its effectiveness before going to the final strategy to integrate it into the program.
The hospital must strategize employing more staff to eliminate other human-related issues such as exhaustion. Notably, the responsible nurse was extremely busy, and they went on to add another client to her care. In addition, the response team was late to arrive after the overdose. The hospital operations cannot be effective unless the ratio of health workers to that of the patient they serve is within the acceptable limit. Moreover, there should be role specifications so that only one nurse is responsible for giving medication to an assigned patient unless they verbally ask a colleague to help.
Reporting elements for the accrediting or regulatory agencies should include some RCA details and the measures taken to mitigate or stop the reoccurrence of the error. The State Department of Health and Human Services should be given information about the nature of the error (overdose), the staff responsible, measures taken to address the challenge, and recommendations. The rationale is that they can help implement changes, such as hiring staff to reduce workload. The Joint Commission should be told about the nature of the error, lessons, and changes made so that they advise the hospital.
Role of Patient and Family
Patients and families have a role to be actively involved in the treatment process by asking questions about all the medical procedures and rationale. For instance, the patient should enquire about the tests done, the drugs prescribed, and the reasons. It is vital for the client to inform the nurses about the drugs they are taking. If they have any allergies or are already using some drugs, they should make sure that they inform the medics to help with the assessment and prescription of alternative treatment. In cases where the patient is unable to communicate because of pain, unconsciousness, and age, the family member should be active in following up on the treatment and helping the medics with relevant details about the patient.
In addition, the family should contact the medics promptly in case of an emergency where the patient is not in a position to respond. For instance, after the overdose, Ms.Viani tried to reach the call bell, but she felt lightheaded and fainted. If there were relatives taking care of her, they would have prevented her from falling and having sprained wrist and laceration. Furthermore, they would have called for an emergency nurse on time. The family members of the clients are also responsible for paying for the services that the medical experts recommend so that nothing hinders the treatment. Thus, patients need to be accompanied by significant who help provide information and act as untrained caregivers.
Strategy Measurement
The hospital administrators can measure the strategy qualitatively through medics’ interviews and patient reviews. In addition, there will be quantitative measures through incidence report data collection, which is evaluated monthly to determine the percentage of error that occurred. The primary measures will be the frequency of incidences, several positive remarks from patients, and the level of satisfaction and teamwork by the medical professionals. If, after implementation of the strategy, the percentage of errors reduces, nurses are more satisfied, and clients give frequent positive feedback, it will be evidence of its effectiveness.
Disclosure
It is vital to report the medical error on Ms. Viani, following the hospital’s recommended protocols and procedures. The key elements to consider are the hospital authority, persons involved, nature of the error, timing, and how it was resolved. The preparation and method of the disclosure are critical in helping the patients and families understand. Preferably, the responsible nurse should wait until the patient is stable and then use a face-to-face approach to reveal all the facts leading to the error and apologize. The communication should be done in a private room and may include a counselor or mediator depending on the intensity of the aftermath.
Patient Safety Culture
Healthcare organizations should be guided by values, beliefs, norms, and policies that form the foundation of a patient safety culture. A quick survey of Mesa Valley Hospital shows that the nurses are concerned about the patients and have empathy. However, due to poor teamwork, communication, and transition, the quality of care is not as client-centered as it should be. The hospital can improve on staff cooperation, reporting, and transitions. The outcome of implementing the patient safety policy will be an enhanced quality of life, reduced days of hospitalization, and minimal readmission. The method to enhance a patient safety environment is training all staff on how to implement patient safety measures.
Communication
Effective communication is when the right message is delivered to the intended personnel on time, to allow them respond or act accordingly. Clarity and continuity are vital for effective communication and better patient care. An effective tool for team building and communication is brief intervention with clarity of goals, roles, and transition plans for all staff. The strategy integrates these attributes to ensure safer patient care by promoting collaboration and cooperation of the health team workers. Evidence from a systematic review shows that after follow-up, the functioning healthcare team were better team players who supported clients (Kilpatrick et al., 2020). Using analytical frameworks such as the percentage of errors after the implementation will help assess improvement in the flow of conversation. Pre-made survey inventories are available for a formal evaluation and assessment, ensuring content validity, internal consistency, and interrater agreement (Kash et al., 2018). Moreover, through observation, the expectation is that there will be lesser conflicts and improved transition.
References
Donaldson, L., Ricciardi, W., Sheridan, S., & Tartaglia, R. (2020). Guidelines and safety practices for improving patient safety. In Textbook of patient safety and clinical risk management (pp. 3-17). Springer Nature.
Kash, B. A., Cheon, O., Halzack, N. M., & Miller, T. R. (2018). Measuring Team Effectiveness in the Health Care Setting: An Inventory of Survey Tools. Health services insights, 11, 1178632918796230. Web.
Kilpatrick, K., Paquette, L., Jabbour, M., Tchouaket, E., Fernandez, N., Al Hakim, G., Landry, V., Gauthier, N., Beaulieu, M., & Dubois, C. (2020). Systematic review of the characteristics of brief team interventions to clarify roles and improve functioning in healthcare teams. PLOS ONE, 15(6), e0234416. Web.