Introduction
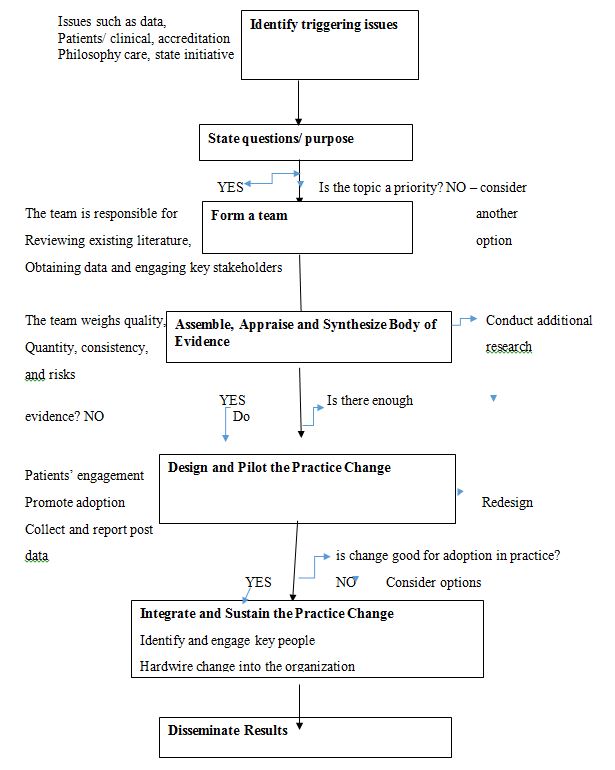
Applying a model ensures that a process is in place to guide the efforts for change. For this project, the Iowa model framework will be used. It helps guide nurses to utilize research findings to improve patient care. The Iowa model shines a light on knowledge, problem-focused triggers, collaboration, and organization using research. The model is relevant since it promotes quality care based on EBP, and the project deals with providing quality care in correctional institutions that treat people with substance use disorder.
Stages Utilized in the Model
Identifying the topic/ triggering issues. While identifying a topic, several factors shall be considered. The core issues will reflect national quality strategies such as the Consumer Assessment of Healthcare Providers and Systems survey and initiatives from accrediting agencies like the Joint Commission (Wynendaele et al., 2019).
State the question or purpose. The PICOT format can be used to focus on the body of evidence and answer the decision point question. It is crucial to decide because a low-priority project will not likely receive the necessary resources and support. Therefore, if the topic is not a priority, another question should be selected, or another issue/opportunity shall be considered.
Building a team. Interprofessional involvement and necessary skills to plan, conduct and evaluate the project are acceptable when selecting team members (Griffiths et al., 2018). The team will review existing literature, obtain baseline data, and engage essential stakeholders (Carlisle et al., 2020).
Assemble, appraise, and synthesize a body of evidence. Systemic research is conducted by the team members who weigh quality, quantity, consistency, and risks. If there is insufficient evidence, it is advisable to conduct more research. It brings new findings and results assembled with evidence from another research.
Design and pilot the practice change. The team engages patients and families and incorporates their values and preferences (Musy et al., 2021). There is also a need to address constraints, necessary resources, and approvals, so the committee should review to avoid wasting resources on unsuccessful change practices. There should also be guidance for piloting the practice change and developing an implementation plan and preparing clinicians and materials to reach the needed planned change.
Integrate and sustain the practice change. The team identifies and engages vital personnel as integration needs new change champions and groups. Incorporating this stage for integration creates linkages with the governance structure, promoting the right influence required from senior leadership. It means embedding a new practice into the organization.
Disseminate results. The results can be published internally, and lessons learned can be shared externally. The evidence should show that it can contribute to patient care. The team members should conduct audits and feedback. Through evaluation, the members can assess the program’s impact and consistency against an actual change with the desired effect.
Conclusion
The nurses’ responsibility and core duty are to provide high-quality health care to patients. The organization can only achieve this by giving them an effective evidence-based program. For this to be implemented, all institution personnel must prioritize the systems and ways to successfully manage the tasks outlined in the stages of the model. Nurses should be given proper training about the EBP, and the Iowa model helps improve their practice continually (Shin et al., 2018). Utilizing the Iowa model and the stages thereof is considered applicable for the goals recognized for the project implementation.
References
Carlisle, B., Perera, A., Stutzman, S. E., Brown-Cleere, S., Parwaiz, A., & Olson, D. M. (2020). Efficacy of using available data to examine nurse staffing ratios and quality of care metrics. The Journal of Neuroscience Nursing: Journal of the American Association of Neuroscience Nurses, 52(2), 78–83. Web.
Griffiths, P., Recio-Saucedo, A., Dall’Ora, C., Briggs, J., Maruotti, A., Meredith, P., Smith, G. B., Ball, J., & Missed Care Study Group. (2018). The association between nurse staffing and omissions in nursing care: A systematic review. Journal of Advanced Nursing, 74(7), 1474–1487.
Musy, S. N., Endrich, O., Leichtle, A. B., Griffiths, P., Nakas, C. T., & Simon, M. (2021). The association between nurse staffing and inpatient mortality: A shift-level retrospective longitudinal study. International Journal of Nursing Studies, 120(103950), 103950. Web.
Shin, S., Park, J.-H., & Bae, S.-H. (2018). Nurse staffing and nurse outcomes: A systematic review and meta-analysis. Nursing Outlook, 66(3), 273–282. Web.
Wynendaele, H., Willems, R., & Trybou, J. (2019). Systematic review: Association between the patient–nurse ratio and nurse outcomes in acute care hospitals. Journal of Nursing Management, 27(5), 896–917. Web.
Appendix A