Introduction
Writing a family history is a rather important procedure that can reveal key health concerns and enable someone to become more aware of any potential health threats. Such a history can show family members, as well as care providers, the areas that require greater attention. The determination of the risk of diseases is one of the pivotal goals in creating a family history. In this regard, the present paper will discuss hereditary patterns, disease transmission, and feasibility of using the Surgeon General’s family history tool in the context of family analysis.
Heredity Patterns
The concept of hereditary patterns refers to those diseases and health conditions that may be inherited by future generations. In particular, the specification of such factors is beneficial in understanding what serious diseases and complications may occur in one or another family member. As argued by Wu et al. (2014), the quality of the family history assessment tool is reliable as it is based on numerous studies. Therefore, the information provided by the mentioned tool can be regarded as credible and thought-provoking.
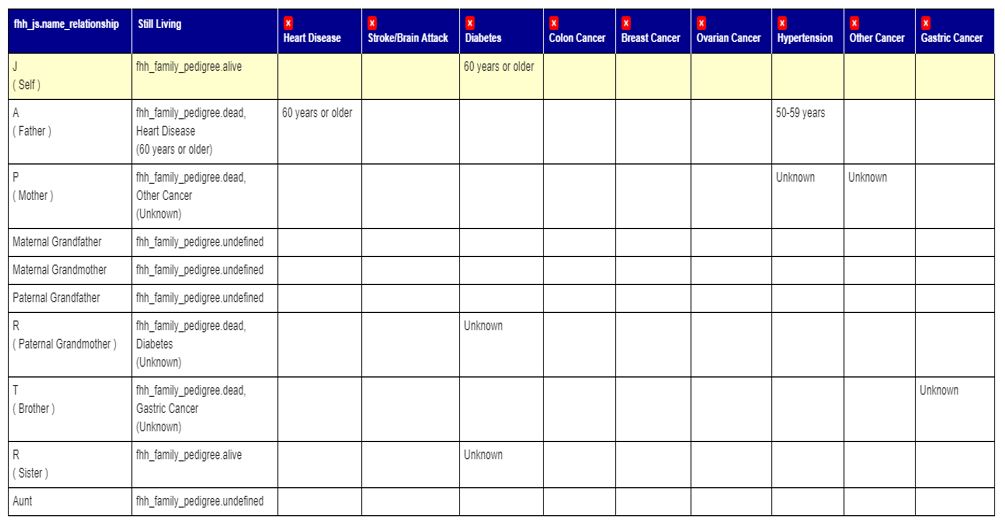
With regard to the given family, it seems essential to briefly identify the health issues of the patient and her family members. Mrs. J is aged 65 and suffers from diabetes; she has one sister who is also diagnosed with diabetes, and one brother who died from gastric cancer. Both parents are deceased – a mother died from endometrial cancer and had hypertension, and a father suffered from heart disease and also had hypertension. Among the sisters and brothers of the parents, the following diseases were noted: diabetes, breast cancer, heart disease, renal failure, and hypertension. Table 1 in the Appendices presents the full picture of the family’s health history.
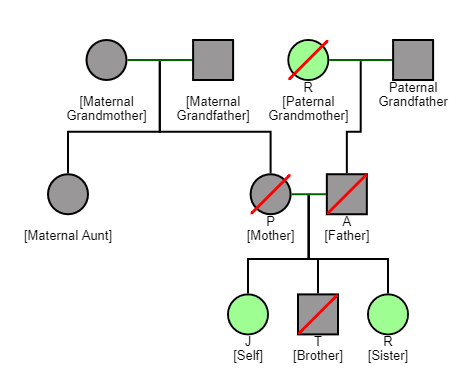
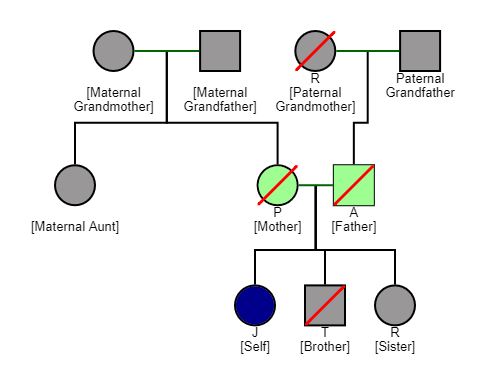
Based on the Surgeon General’s family history tool, it is possible to distinguish between such hereditary patterns as diabetes and hypertension. The patient’s paternal grandmother had diabetes, while the next generation was not marked with this disease (see Diagram 1). Nevertheless, they still were the transferees of diabetes down to the next generation; both the patient and her sister developed this condition. Following this patter, one may assume that children of the preceding generation will not be diagnosed with diabetes, while their children will be at an increased risk. The latter is associated with the fact that the disease can be transmitted through a generation.
The second hereditary condition is hypertension (see Diagram 2) as both the mother and father of the patient suffered from this particular health condition. In addition, the father’s brother also has hypertension, as well as other diseases that are not present in other family members. Even though several family members have the above disease, it is still difficult to confidently claim that hypertension is a hereditary illness in this family. Currently, scholars cannot conclusively state that this is the case because the increase of blood pressure involves not only one disease but several factors (Lieb et al., 2013). Therefore, it is obvious that the development of hypertension is determined by the action of not one but a number of genes that can interact with each other, which also has a different effect on the health of the patient (Lieb et al., 2013). In addition, the manifestation of the action of genes depends on environmental conditions – nutrition, stress, and emotional health, thus creating a complex picture of inheritance predisposition to hypertension.
Risk of Disease Transmission
When speaking of the risk of disease transmission to other or new family members, one should state that the risks of diabetes, hypertension, and cancer transmission are high in the given family. It is impossible to state that the mentioned diseases are inherited in the given family, even though the predisposition to the development of the identified conditions may be transmitted, as not only one cell but a group of them is responsible for the development of illnesses.
In this family, diabetes risk is 60-80 percent of the total likelihood of getting sick. If a person in previous generations has or had diabetic relatives, he or she is exposed to risks identified on the basis of several regularities (Leong, Rahme, & Dasgupta, 2014). For example, in this present case study, an insulin-dependent form can be transmitted through a generation. In other words, if grandparents are ill with diabetes, and their children are healthy, their grandchildren may get sick. The probability of inheritance of a child with diabetes of the first type in cases of illness in one of the parents is 5 percent. If the mother is sick, the risk of the child’s illness is 3 percent, if the father is sick it is 9 percent, and with both parents it increases to 21 percent (Leong et al., 2014). Excess weight and unhealthy lifestyle choices speed up the onset of the disease. When assessing risks, not only close relatives are considered. Taking into account all the relatives that have diabetes of one type, the more sick people with diabetes in the family, the higher the risk of getting sick.
As for hypertension transmission rates, there is evidence of a higher percentage. Looking at the percentage, the heredity risk factor will be equal to 60-80 percent of the total probability of getting sick. Indeed, Mendlowitz regards heredity of decisive importance in the onset of hypertensive disease (as cited in Peacock, Diaz, Viera, Schwartz, & Shimbo, 2014). Pickering also considers the role of heredity in the genesis of essential hypertension to be proven, but emphasizes the lack of adequate control in this type of research (as cited in Peacock et al., 2014). It is specified that in the case of the inheritance of this disease, there is a transmission of a dominant type with an incomplete manifestation of the gene.
It has been established that hypertension affects many members of the same family, but how it is transmitted from parents to children is still unclear. Nevertheless, it is possible that some mechanisms leading, ultimately, to increased arterial pressure are controlled by hereditary factors (Mancia et al., 2013). It is known that hypertension in families where relatives suffer from high blood pressure develop this disease more often than members of other families. Having parents with hypertension, children are four times more likely to suffer from it than others (Mancia et al., 2013). It is important to note that genetically a person cannot inherit hypertension, but only the predisposition to it due to the peculiarities of metabolism and neuropsychic reactions. With the onset of hypertension, there is a contributing situation for the development of type 2 diabetes.
At the same time, the Surgeon General’s family history tool provides the opportunity to assess colorectal cancer risks. According to Giardiello et al. (2014), the so-called Lynch syndrome, also known as hereditary nonpolyposis colorectal cancer, is a disease with an autosomal dominant type of inheritance, accounting for 3-5 percent of all cases of colorectal cancer. The presence of colorectal cancer can be suspected on the basis of the family history and confirmation by means of genetic testing. Patients should be monitored for tumors in other locations, especially endometrial and ovarian cancers (Giardiello et al., 2014). Considering that this family has one relative with endometrial cancer and one with rectal cancer, the risk of developing similar diseases is relatively high. Therefore, relatives of the patients with rectal cancer should perform a colonoscopy every 1-2 years beginning with the third decade of life, and annually from the age of 40. Women should be examined annually for endometrial and ovarian cancer. Genetic testing is important to determine the diagnosis.
Feasibility of Using the Surgeon General’s Family History
Taking into account that the Surgeon General’s family history tool enables the discussion of both hereditary patterns and transition risks for the given family, its use in nursing practice cannot be overestimated. There are a large number of diseases to which a person has a genetic predisposition. The development of illnesses related to these is accompanied by the interaction of hereditary factors, including genes and mutations, and environmental aspects. Many of the most common chronic ailments, like diabetes and hypertension, tend to be linked to familial accumulation, though not explicitly expressed genetically.
It is believed that all diseases and malformations, occupying the largest place in human pathology, are almost always the result of the combination of genetic and environmental factors. This means that mere hereditary influence is not enough for the development of such diseases. However, the impact of nutrition, physical activity, and other issues is essential. The earlier a disease manifests in a particular patient, the more difficult it is, and the more sick relatives he or she has, the higher the genetic predisposition and the inheritance risk for future children in this family. Here is another important difference of multifactorial diseases from strictly hereditary: if the risk increases with the boost in the number of patients in the family in the first case, then in the second, it remains unchanged.
The use of the mentioned tool is necessary to assist family members in identifying possible future risk and by being able to take preventative measures. Since a predisposition is formed by a multitude of genes with a weak individual contribution of each of them, it is possible to make a qualitative genetic portrait of predisposition to this or that disease. However, it should be remembered that treatment can only be effective if it is prescribed in time, and this is possible with early diagnosis of the disease, before the body has undergone irreversible changes. In this regard, the use of the family history assessment tool is helpful to become aware of existing threats and to be able to develop relevant preventative measures.
Conclusion
In conclusion, it should be emphasized that the presented family has hereditary patterns of diabetes and hypertension. The former condition is associated with a non-direct transition, when grandparents and grandchildren develop the disease, and parents are not diagnosed with diabetes. It is revealed that the Surgeon General’s family history tool is a reliable and relevant instrument to help family members and care providers in assessing risk factors in a timely manner. Therefore, it is proposed to utilize the above tool in nursing practice as a means of determining patients’ genetic predisposition issues.
References
Giardiello, F. M., Allen, J. I., Axilbund, J. E., Boland, C. R., Burke, C. A., Burt, R. W.,… Levin, T. R. (2014). Guidelines on genetic evaluation and management of Lynch syndrome: A consensus statement by the US multi-society task force on colorectal cancer. Gastroenterology, 147(2), 502-526. Web.
Leong, A., Rahme, E., & Dasgupta, K. (2014). Spousal diabetes as a diabetes risk factor: A systematic review and meta-analysis. BMC Medicine, 12(1), 12-24. Web.
Lieb, W., Jansen, H., Loley, C., Pencina, M. J., Nelson, C. P., Newton-Cheh, C.,… Hall, A. S. (2013). Genetic predisposition to higher blood pressure increases coronary artery disease risk. Hypertension, 72(2), 995-1001. Web.
Mancia, G., Fagard, R., Narkiewicz, K., Redon, J., Zanchetti, A., Böhm, M.,… Galderisi, M. (2013). 2013 ESH/ESC guidelines for the management of arterial hypertension: The task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Blood Pressure, 22(4), 193-278. Web.
Peacock, J., Diaz, K. M., Viera, A. J., Schwartz, J. E., & Shimbo, D. (2014). Unmasking masked hypertension: Prevalence, clinical implications, diagnosis, correlates and future directions. Journal of Human Hypertension, 28(9), 521-528. Web.
Wu, R. R., Himmel, T. L., Buchanan, A. H., Powell, K. P., Hauser, E. R., Ginsburg, G. S.,… Orlando, L. A. (2014). Quality of family history collection with use of a patient facing family history assessment tool. BMC Family Practice, 15(1), 31-39. Web.
Appendices