Villa Health Remote Collaboration Scenario
In the media scenario, various stakeholders are looking for a solution concerning Caitlynn, a two-year-old patient who has pneumonia. Caitlynn has been admitted for the second time in six months at Valley City Regional Hospital. With the intervention of Dr. Erica Copeland and Virginia Anderson, there are various measures taken to see how the issue can be combatted since Caitlynn is not doing well, according to her mother, Janice. The child’s health complication is related to cystic fibrosis as Dr. Copeland says and they all embark on methodologies that can help get a better solution.
From the case study, a reader can see Dr. Copeland and Ms. Anderson calling various professionals on skype, including Madeline Becker and Rebecca Helgo, among others. The partnership, which is evident in the scene, depicts a remote collaboration in healthcare. This video presents a proposal of an evidence-based plan (EBP) that will improve Caitlynn’s medical situation and identification of benefits of remote collaboration in the scenario.
Evidence-Based Care Plan to Improve the Patient’s Safety and Outcome
The safety and outcome of the care that Caitlynn undergoes can be improved by a raft of elements that are important in nursing cystic fibrosis (CF). It is important to first highlight the extent to which the child has risks to her safety from the current chronic illness she has (Sumner & Walshaw, 2018). CF is caused by a mutation in the gene of cystic fibrosis transmembrane conductance regulator (CFTR), which occurs in the mucus-producing body cells (Wei Chern, 2021). The clinical manifestation is a long-lasting lung disease which brings the idea of pneumonia that Caitlynn was diagnosed with during her previous admission. As the scenario presents, her sweat glands have been affected and that is why Dr. Copeland insists that the child’s temperature must be checked. This video proposes impaired gas exchange as the EBP to improve outcomes and safety for Caitlynn.
Impaired Gas Exchange
This EBP strategy will work for the patient as she will maintain optimal gas exchange which shall be evidenced by oxygen fullness of almost 90% and relaxed breathing (Bartlett et al., 2019). Additionally, the plan will ensure that Caitlynn has no further worsened in her level of consciousness as the EBP will create an advanced baseline heart rate, among other issues. Therefore, the desired outcome here will be to improve her outcome from Dr. Copeland’s intervention measures. Several nursing interventions will be necessary to conduct as far as the chronic issue is concerned.
During the plan, it is important to monitor respiratory and heart rate to detect any alterations. Under this intervention, there is a guarantee of a high heart rate because the system will be compensating for early hypoxia (Bartlett et al., 2019). It is also important to assess any deviations in the status of respiration, for instance, pallor, cyanosis, awareness level, and breathing difficulty, if any. The reason for doing that is that Caitlynn has high chance of adjusting to the breathing pattern over time as one way of enabling gas exchange. The plan is essential because it shows oddities that may show respiratory cooperation, hypoxia, and hypercarbia.
The other task under the impaired gas exchange will be to track transcutaneous carbon dioxide. A caregiver needs to do that because underlying hypercarbia may be present because the scenario shows Caitlynn having moderate CF (Sumner & Walshaw, 2018). If the levels increase, it means that the child may have a progressive acute infection and possible respiration failure. At this point, the EBP guides a professional to offer physiotherapy and other prescriptions to ease the problem.
The plan also involves intervention such as monitoring arterial blood gases and saturation of oxygen and provision of adequate relaxation between activities when the child is active during the day. This ensures that oxygen supply is increased without fatigue. Another recommendation that should be made to improve Caitlynn’s condition is to place her in a semi-Fowler position (Bartlett et al., 2019). That will facilitate lung expansion and reduce the chances of airway collapse which prevents Caitlynn from dyspnea.
During caregiving, it is important to administer oxygen therapy that Dr. Copeland proposed which helps in relieving dyspnea and maintaining sufficient oxygenation in the entire body. Here, the goal is to increase her comfort, and oxygen saturation must be equal to or greater than 90% (Bartlett et al., 2019). Lastly, a nurse should make efforts to reach care personnel to have critical monitoring of noninvasive ventilation that assists with nighttime ventilatory requirements. Therefore, the EBP will perfectly work to improve the condition that Caitlyn has.
Ways in which an EBP Model was used to Develop the Plan
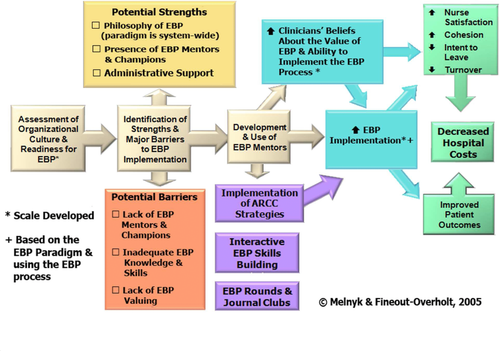
This video employed some metrics from Advancing Research and Clinical Practice Through Close Collaboration (ARCC). First, it enabled the assessment of the culture and organizational readiness in implementing the potential plan in the case of Caitlynn (Melnyk et al., 2016). First, Valley City Regional Hospital is an outgoing healthcare institution under team leader Dr. Copeland. There is a culture of embracing clinical procedures that have evidence of combatting a certain issue. The presence of some professionals such as Virginia Anderson, Marta Simons, Madeline Becker, and Rebecca Helgo shows that the group could easily adopt the proposed care plan. ARCC also guides in identifying facilitators and barriers of the EBP process whereby the facilitators would be the stakeholders, as shown in Figure 1 (Melnyk et al., 2016). Although some barriers such as the internet and time, could be evident, the individuals are willing to set time for the scheduled clinical procedures.
Through ACRR, it is easy to know who could be mentors for the process and in this case, Dr. Copeland and Anderson have a leading role as they can keep in touch with Janice, the mother of Caitlynn. The model also assisted in realizing the possibility of implementing the plan through the interest and professional commitment that are bound by ethical considerations (Melnyk et al., 2016). Lastly, through the model, careful articulation on how evaluation of outcomes from the practice is feasible. In this case, all the stakeholders are professionals and the patient’s parents are willing to co-operate.
The Most Relevant Evidence While Making Decisions for the Plan
In the plan, two pieces of evidence seemed to be most relevant in combatting the child’s situation. First, the adaptation of breathing patterns from the assessment of deviations in respiratory status was critical. The reason why this evidence appears to be most relevant is that in that case, Caitlynn would show abnormalities in respiration and thus, apply the adequate prescriptions that ensure her status is improved (Sumner & Walshaw, 2018). The important factor to consider here is the clinical manifestation of the improved state of illness for the young patient.
Second, the maintenance of adequate oxygenation is also notably relevant. Due to the administration of oxygen therapy, the caregiver can balance the oxygen levels in Caitlynn, who has CF. The evidence is encouraging since the patient’s care providers will be able to see whether she has reached the 90% level (Sumner & Walshaw, 2018). With the two pieces of evidence in place, the EBP proposed in this video will be effective and thus, improve patient outcomes.
Benefits and Strategies to Mitigate the Challenges of Interdisciplinary Collaboration
Benefits of interdisciplinary Collaboration
Through interprofessional collaboration in healthcare, there is potential for improved care and outcomes. For instance, Madeline Becker, a social worker at McHenry, is offering insurance information regarding Caitlynn’s parents, whereby she informs the others of the need to have money for the issue (Wei Chern, 2021). Through such interaction, the parents will understand the required steps that will lead to insurance coverage as one way to treat their child. The other benefit is that such collaboration reduces medical errors as there is a comparison of ideas from different professionals with diverse information and expertise power. In the scenario, there is a doctor, a pediatric caregiver, and social workers who think critically about how they can assist Caitlynn.
Strategies to Mitigate Challenges of Interdisciplinary Collaborations
For a successful interprofessional collaboration, it is important to provide a platform for social interaction. In the scenario, the stakeholders would communicate via emails, text messages, and Skype. The other strategy is to recognize the capability of other professionals by giving them time to elaborate and question various issues (Wei Chern, 2021). The media has Dr. Copeland asking the other professionals for clarification concerning CF protocol. Lastly. It is essential to share knowledge through proper communication. It is risky to share data that is not credible or work by giving doubting information.
References
Bartlett, L., Wooldridge, L., & Evans, S. (2019). P053 Evaluation of cystic fibrosis nursing standards for newborn screened diagnosis – do we deliver? Journal Of Cystic Fibrosis, 18(7), S71-S72. Web.
Melnyk, B., Fineout-Overholt, E., Giggleman, M., & Choy, K. (2016). A Test of the ARCC model improves the implementation of evidence-based practice, healthcare culture, and patient outcomes. Worldviews On Evidence-Based Nursing, 14(1), 5-9. Web.
Sumner, C., & Walshaw, M. (2018). P235 The cost of caring: Nursing experiences of palliation within cystic fibrosis care. Journal Of Cystic Fibrosis, 17(6), S125-S126. Web.
Wei Chern, A. (2021). Healthcare professionals’ experiences on interdisciplinary collaboration in a medical department of a Malaysian General Hospital. Medicine & Health, 16(1), 246-255. Web.