Outline
Introduction – background of the problem of HIV/AIDS in South Africa, extent of prevalence of the disease, what is HIV/AIDS, the impact of the disease on the health system of the company and structure of the dissertation
Literature review – epidemiology of HIV and AIDS in SA; demographic features; prevention and treatment programs
HIV/AIDS – History and Origin of the disease; demographic and health effects of the epidemic
Salient features of the healthcare system in SA: status of public healthcare and challenges facing the system: ways to mitigate the challenges: Nurse-based treatment programs
Changes in the healthcare system because of increased incidence of HIV/AIDS: changes in role and responsibilities of nurses
Strategies for treatment and prevention: managing HIV/AIDS as a chronic disease: prevention strategies
Abstract
The healthcare system in South Africa is struggling to meet the increased demand for health services because of the devastating impact of HIV/AIDS. The government has the goal of respect of meeting its post-apartheid mandate of providing equitable health services to all. However, the health system is understaffed and under-resourced. The problems encountered in the provision of healthcare drive the government to have a thorough relook at the reorganization of the health system in the country.
In this context, this study examines the state of HIV/AIDS in South Africa with a specific focus on the challenges faced by the healthcare system and the strategies that the government, communities and society need to follow to treat and prevent the incidence of HIV/AIDS. The study finds the bio-medical prevention strategies are comparatively better and effective in preventing the spread of HIV/AIDS and it suggests the implementation of a combination prevention strategy, which includes successful HIV behavior-change programs.
Introduction
The AIDS epidemic has been one of the most destructive health crises of recent times. It is ravaging families and communities throughout the world by its dreadful effect on the health of people. An estimated population of more than 33.4 million was infected with HIV/AIDS in the year 2008 globally. More than 25 million people have lost their lives because of this disease since the year 1981. There is an alarming growth in the number of people, who are newly infected with HIV.
It is estimated that around 95% of the people with HIV/AIDS live in the sub-Saharan Africa, Eastern Europe or Asia. African countries are the ones that are severely affected and many other countries are also affected to some extent by the disease. Despite the efforts of the countries to lower the effects of the disease, a large mass of people had contracted the disease and the impact on the society continues to affect them. South Africa is one of the worst affected countries by the HIV/AIDS epidemic. In this country, as estimated 5.7 million people have been identified to be living with HIV and AIDS in the year 2009, which represents the most number of number of people living with HIV infection than in any other country.
The killer disease adversely affected the lives of families in different ways. Mother-to-child transmission is found to be one of the main infection route. South Africa, being a developing country, HIV/AIDS has a significant impact on the healthcare system of the country. This research attempts to present a detailed account of the impact of HIV/AIDS on the healthcare system of South Africa.
Background of the Problem
Among the social challenges of the present era, Acquired Immune Deficiency Syndrome (shortly called AIDS) is one of the leading epidemic causing untold miseries to millions of adults and children throughout the world with more number of people affected in the sub-Saharan African countries. This socio-medical problem has been the center of attention of all countries around the globe. The electron microscopic virus of AIDS known as “Human Immune Deficiency Virus” (shortly called HIV) has already infected millions of people and the incidence is increasing in an alarming rate in all the countries. AIDS cannot be considered a simple medical problem.
With its associated morbidity and mortality, this epidemic has made every aspect of the life of an individual vulnerable to great damage (Morrison et al, 2002). The infection with AIDS/HIV is not just a cultural issue or a result of moral decadence but is aggravated by social and economic problems of the country, which are the contributing factors. Therefore, there is the need to look into the epidemic from a socio-economic perspective for reducing the incidence of the infection.
Although the epidemic is not limited to one geographical location in the world, it has proven to cause greater damage to the country of South Africa. The epidemic has proven to be a threat to the economic development of the country, because of its ramifications on the economic well-being of the people and the communities. In this context, this research examines the impact of HIV/AIDS on the healthcare system of South Africa, being one of the countries, worst hit by the epidemic.
Statement of the Problem
HIV/AIDS has become a global pandemic and it has spread to every corner of the world. It has become a widespread and fundamental threat to the human development, especially in the sub-Saharan Africa. South Africa is experiencing the most dreadful effects of the epidemic in the world (Jackson, 2002). The country has the highest infection rates with as many as one in every three adults is infected with the disease (Clark, 2002).
Millions of children have become the victims of the killer disease and it has knocked off several years in the life expectancy of the people. AIDS has become a significant threat to food security. It affects the productivity and availability of human resources and blocks the development of the economy (Jackson, 2002). Apart from the effect on the economy, it leaves a mark on the individual and the family, which affects people in different ways.
The impact of HIV/AIDS has reached through to the macroeconomic level and it has its effect on the global economy. The epidemic is a long-term development disaster being witnessed in a massive scale and South Africa is enduring the most of it. The epidemic has an effect on the functioning of the healthcare department of South Africa by enlarging the need for healthcare both quantitatively and in complexity. It has the effect of a decrease in the provision of healthcare by affecting the people and functioning of the healthcare workers. Another factor, which makes the study of the issue of HIV/AIDS in South Africa important, is that two thirds of all new infections happen among people aged between 15 and 24.
It is estimated that on a global level, more than 50 percent of the HIV infections have been found in people under 25 years of age, with 60 percent of infections occurring in females under the age of 20. The epidemic thus affects the hopes and lives of a generation by killing the breadwinners of families. The problem has become beyond control in the context of South Africa in terms of the available healthcare services to contain the spreading of the infection and it makes this study significant.
Research Questions and Sub Questions
This research attempts to answer the following main research question.
What is the impact of HIV/AIDS on the healthcare system of South Africa?
This main research question leads to the following research sub questions, which will be answered through this research.
- What is HIV/AIDS?
- What are the prominent characteristics of South African healthcare System?
- How has the South African healthcare system changed because of the increased incidence of HIV/AIDS in the country?
- What are the strategies that need to be implemented by the South African healthcare system to manage HIV/AIDS effectively?
Significance of the Study
The magnitude of the impact of HIV/AIDS on the healthcare system of South Africa has assumed a large proportion that the country is unable to control the spread of the disease effectively. The number and performance of healthcare workers has been deteriorating and this problem has been associated with enlarged expenses, more particularly when there is no adequate financial provision for ensuring provision of health services.
Factors like shortage of staff, limitations on supplies and medicines and problems of maintaining adequate health infrastructural facilities have been attributed to the fact that the government of South Africa is unable to place a high priority on containing this epidemic. Another dimension of this problem is that the increase in costs to restrict the spread of AIDS reduces supplies in other sectors and there is disproportionate increase in expenditure on HIV/AIDS related illnesses as compared with other illnesses. Provision of services in the areas of increased supply of safe blood, applying new medical protocols and procedures and prevention of transmission of HIV from mother to children has increased the cost of healthcare services.
The provision of new HIV/AIDS therapies including antiretroviral drugs has also contributed to the increased cost of healthcare services. This calls for a complete analysis of the impact of HIV/AIDS on the healthcare system of South Africa and suggestions for effecting improvements in the healthcare system to make services available to more number of affected people. A critical evaluation of the impact of the incidence of HIV/AIDS on the healthcare system of South Africa and recommendations for effecting improvements in the provision of healthcare services is the central focus of this study.
Organization of the Study
For making a comprehensive presentation, this research report is organized to have different chapters. Chapter One presents a background and significance of the study. This chapter also lays down the research questions and sub questions proposed to be answered by the research. Chapter Two contains a review of the available literature on the topic of study to add to the existing knowledge on the subject. While Chapter Three explains what HIV/AIDS is, Chapter Four presents the salient features of the healthcare systems of South Africa. Chapter Five describes the changes in the healthcare system of the country of South Africa because of the incidence of HIV/AIDs. Chapter Six suggests few strategies to improve the healthcare system of South Africa to manage the HIV/AIDS effectively. Chapter Seven concludes the report by summarizing the salient issues discussed within the text of the research report.
Literature Review
HIV/AIDS is the leading cause of death in South Africa. An estimated population of nearly 5.7 million people were living with HIV and AIDS in South Africa in the year 2009. This number is more than the population affected by the disease in any other country. The number of deaths occurred in the year 2008 was estimated to be around 250,000 in 2008 in South Africa. The prevalence of the disease is found in more than 15% among the age group of 15 – 49. It is found that almost one in three women in the age group of 25 – 29 and over 25% of the men in the age group of 30 – 34 are affected by HIV/AIDS.
The spread of the disease has brought drastic increase in the number of deaths in the country. There has been a sharp increase in the number of deaths from 316,559 in the year 1997 to 607,184 in the year 2006. The young adults are the prominent among the people who shoulder the burden of increasing mortality rate. In the year 2006, 41 percent of deaths occurred among 25-49 year old people, which increased from 29 percent in the year 1997. South Africa’s HIV and AIDS epidemic has a devastating effect on the healthcare system of the country. This review focuses on the findings of the past literature on the effect of HIV/AIDS on the South African healthcare system.
HIV and AIDS Epidemiology in South Africa
A thorough understanding of the nature, dynamics and characteristics of HIV/AIDS is important to review its impact on the health services of a country. According to UNAIDS and WHO, the prevalence rates and population affected form the basis for describing the extent of the spread of the epidemics. These agencies are of the opinion that HIV and AIDS is not of same magnitude in all the countries because of the dynamic nature of the epidemic, and there is a tendency for it to move from one category to another.
“Even within a country, there may be a series of multiple, changing and overlapping micro-epidemics, each with its own nature (the populations most affected), dynamics (patterns of change over time) and characteristics (severity of impact). By this definition, the South African HIV and AIDS epidemic is generalised. It is firmly established in the general population and sexual networking in the population is sufficient to sustain the epidemic independent of sub-populations at higher risk of infection. A numerical proxy of HIV prevalence consistently >1% in pregnant women has been used to qualify a generalised epidemic (World Bank and WHO use >5%). By this definition alone therefore, South Africa has a generalised epidemic” (SAFAIDS, 2007).
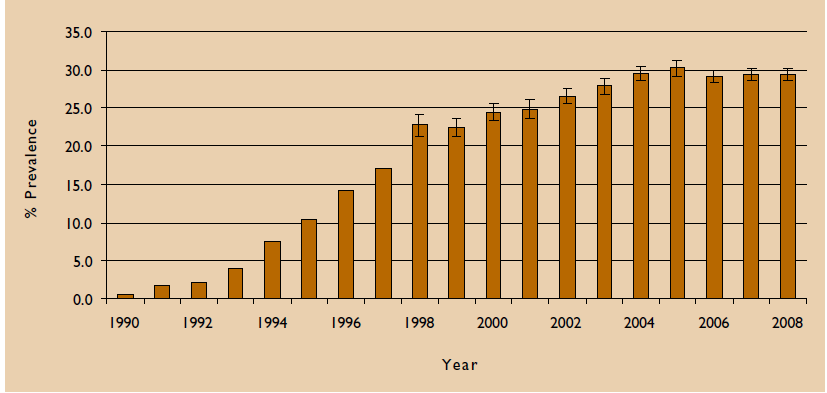
The government of South Africa has been continuously monitoring the HIV prevalence through antenatal HIV and syphilis prevalence surveys, which have been conducted periodically since 1990. The government also conducted population-based surveys and national prevalence survey of youth to control and monitor the spread of HIV/AIDS. Figure 1 illustrates antenatal trends among women during 1990 to 2008.
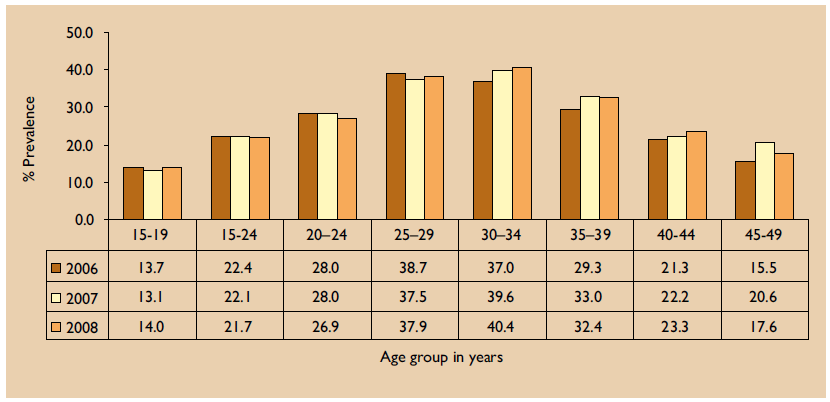
The following figure illustrates the HIV incidence among women in different age groups during the years 2006 to 2008.
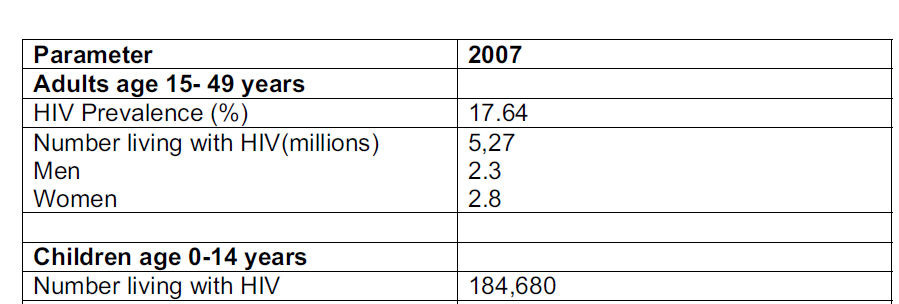
Extrapolation of HIV prevalence to the general population based on antenatal surveys using UNAIDS Spectrum model estimated the total number of people likely have been infected by HIV as of 2007 in South Africa at 5.27 million. While the real proportion of population who might have been infected by HIV might be more, this estimation has been considered as traditional in comparison to the previous estimation of 5.41 million in 2006. The number of people within the age range of 15-49 who are affected by HIV inspection was calculated at 17.64%. The following table exhibits the estimated number of people infected by HIV in other categories.
This study of the epidemic exhibits that HIV incidence continues to act as a public health issue in South Africa. It is important to note that there are several HIV epidemics occurring simultaneously in the country and there is no precise definition of their distribution. Although the National HIV and Syphilis Prevalence Survey conducted by National Department of Health in South Africa suggests that the HIV epidemic in the country is showing a downward trend there is no single factor that could be attributed for the actual decline in the incidence.
The study identified sexual acts leading to AIDS and contact with people like different sex-partners, lorry drivers and miners, who are highly risky people to have sex with as the factors that contribute to the spreading of the epidemic in the country. The study also identified factors like “youth sexual behaviour; reduction in premarital vs. extramarital sexual behaviour; sexual abstinence; mutual faithfulness to one partner; knowing someone who died of an HIV related illness and fewer primary core carriers” (National Department of Health, 2008), as the ones responsible for a decline in the HIV infection.
The diversity in the socio-economic and cultural factors of South Africa has a serious impact on sexual risk behaviors. However, there are prevalence variations between provinces and within districts, which needs an in-depth understanding of the sexual behaviors/characteristics of communities. “Another important observation in 2007 is that HIV prevalence trends amongst participants in the age group 15-19 years continue to show a significant decline from 16.1% in 2004, to 15.9% in 2005, to 13.7% in 2006, to 12.9% in 2007” (National Department of Health, 2008). A decline in prevalence in this age group is suggestive of a decline in HIV incidence.
This reduction also indicates the impact of intervention programs. “The HIV prevalence estimate in older age groups (30 34 and 35 39 years) is a concern as it remains at similar levels with a tendency towards an increase” (National Department of Health, 2008).
Impact of HIV/AIDS on Health Systems
HIV/AIDS has a significant impact on the functioning of health systems, since there is an increased demand for services in respect of both quality and complexity. The epidemic by its impact on the number of health workers and their performance leads to considerable reduction in the supply of services. The procedures involved in the health care for HIV/AIDS entail large costs, particularly when the developing countries do not have adequate financial resources for providing health services. Governments in Sub-Saharan African countries including South Africa place a low priority on health and welfare because of shortage of staff, supplies and medicines and limited maintenance of health infrastructure.
The impact of structural adjustment programs have forced governments to cut back recruitment of new staff or filling of vacant positions caused by attrition and this has also led to shortage of staff. As the AIDS epidemic increases the costs it leads to reduction in the supply in all other sectors of the economy. As a natural consequence, AIDS will increase the share of healthcare in the total national expenditure.
There are a number of factors, which have contributed to major changes in the landscape of health and disease and the need for providing service to control the spreading of the diseases. These factors include the resurgence of previously well-controlled diseases like malnutrition, tuberculosis, diarrhea and other infectious diseases, whose prevalence has enlarged because of the presence of HIV/AIDS.
“This has further caused a “crowding out effect” by HIV/AIDS patients of patients suffering from other illnesses. On the services side, there is an increased demand for safe blood supply, need for new medical procedures and protocols, voluntary counseling and testing (VCT), prevention of mother-to-child transmission of HIV, and the provision of new HIV/AIDS therapies including antiretroviral drugs,” (Tawfik & Kinoti, 2001)
Assessment of existing health facilities suggest that the epidemic creates a crowding out effect on patients suffering from seemingly less severe conditions than HIV/AIDS. This acts to deny them their right to get good healthcare. In South Africa where the epidemic of HIV/AIDS is growing faster than any other country in the world, patients are turned away from the hospitals for want of additional beds (Russell, 2000).
In order to understand the effect of HIV/AIDS on healthcare system in South Africa it becomes necessary to review the progress made by the country in improving health.
Demographic Features
Out of more than 40 million people infected by HIV all over the world, more than five million people are living in South Africa, which constitutes about 10 percent of the total population o the country. In the year 2000, the epidemics of HIV/AIDS accounted for 38 percent of total premature deaths, in which 47 percent were females and 33 percent were males. The increase in the incidence of the epidemics has caused considerable increase in the workload for the healthcare workers.
As seen from the data for the rural district of Hlabisa having a population of 222,000 people, the prevalence of HIV infection increased from 4 percent in 1992 to 35 percent in the year 2002. The number of clinic visits resulted in an increase of 88 percent between the years 1991 and 2001 (Dedicoat et al., 2003) and the hospital admissions rose to 81 percent between 1991 and 1998. This increase has resulted in stress and exhaustion among the healthcare workers.
Even among the healthcare workers, 16 percent of them were found to be showing positive test results for HIV (Bateman, 2004). The results of a national study conducted among 222 health care facilities, which represented public and private sector facilities have confirmed these findings (Shisana et al., 2003). The spread of HIV/AIDS is expected to affect a significant work force of the country over the next decades and create more orphans under the age of 15 years.
“The reduction in the workforce, the increased human and financial resources required to provide care for people living with AIDS, and the needs of orphans will profoundly affect all aspects of social and economic development and the lives and well-being of all” (Benatar, 2004).
This has created a mounting pressure on the healthcare workers and system of the country.
HIV Prevention and Treatment Programs
There have been wide criticisms within the country as well as at the international level about the approach of the government of South Africa in controlling the epidemic of HIV/AIDS. Although the global scientific community has provided overwhelming evidence suggesting the link between HIV infection and AIDS, the government has denied such link. The government failed to promote a prevention campaign over the past decade and the ineffective treatment has contributed to the denial by the government of the existence of HIV pandemic. It also led to the perpetuation of the stigma associated with HIV and AIDS.
It is pointed out that the government has handled the prevention of the transmission of HIV from mothers to children badly. One of the most important advances in the medical management of HIV infection is the ability to reduce vertical transmission of HIV infection. There is the need to promote widespread use of effective preventive measures to prevent the infection among infants during delivery or infancy. It is to be noted that among the infected children mortality rate is 91 percent by the age of eight years (Karim,et al., 2002).
In the context of South Africa, there are a number of obstacles, which operate to frustrate the introduction and maintenance of comprehensive and effective programs for the prevention of the transmission of HIV and for treatment of the infected patients with antiretroviral drugs.
“Such obstacles include a high prevalence of high-risk sexual behavior, extensive sexual violence against children and unempowered women, constraints on financial and human resources, an inadequate health care infrastructure, resistance to adopting bottle feeding rather than breast-feeding, concern about the potential adverse effects of antiretroviral-drug therapy in poor and nutritionally vulnerable populations, concern about promoting drug resistance, and fear of not meeting constitutional requirements for equity,” (Benatar, 2004).
In addition, there has been resistance to introduce antiretroviral treatment in view of the high-cost involved and because of suspicion on the ulterior motives of the firms in the pharmaceutical industry. There was also resistance from powerful nations and multinational drug companies against importing affordable generic drugs. However, there have been changes in the attitudes of all the stakeholders for rectifying and improving the situation to make local production of generic drugs possible and thereby to cause substantial reduction in the prices of essential drugs.
In South Africa as well as in other African countries, a purely biomedical approach to address HIV and AIDS has deflected the attention from focusing on other social issues such as “extreme poverty, poor sanitation and nutrition, dysfunctional families, a lack of recreational facilities, sexual promiscuity, and high crime rates.” These problems are widespread in South Africa, which has been affected greatly by the global economic forces, which have aggravated disparities in wealth and health and which are relevant for controlling the infectious diseases. The history of tuberculosis clearly illustrates this situation (Gandy, 2003).
Another factor that affects the proper treatment for the epidemic is the theft of drugs from the public health system and the growth of crime syndicate (Shaw, 2002). A large number of illegal immigrants who enter the country in search of treatment also have a harmful effect on an effective antiretroviral treatment program, which is monitored inadequately.
HIV/AIDS
The objective of this chapter is to present a descriptive report on HIV/AIDS and the effects of this disease on human beings.
Almost all major infectious diseases had more than one associated epidemic in the form of the illness itself and the reaction of the society to such illness. The fear of being infected and lack of knowledge on the causes for the infection have often led to insensible and even uncivilized practices to contain the infection. HIV/AIDS has also been one of the subjects of forceful reporting by accepted media and even by academic literature (Morrison et al., 2002).
There has been a wide variety of responses in the context of culture and society with respect to the cause and effect of HIV/AIDS epidemic. For instance, the cultural responses for the killer disease have been associated with gay men, who were heavily impacted by the disease. Lack of complete knowledge about then infection and its cause and impact has been one of the reasons for the attribution of different dimensions to the disease. This chapter provides a detailed account of the disease.
HIV/AIDS – a Background Note
Human Immune Deficiency Virus (HIV) works to destroy the immune system of human body. Consequently, even the minor and least lethal ailments may turn out to be fatal for the person infected with the virus. The patients may not recognize the HIV infection for many years, as they may remain symptom-free for a prolonged period. This period where the patients are unable to recognize the infection is known as “carrier state”. This is the most dangerous phase in the process of HIV infection. The people who are called the carriers may transfer the virus present in their bodies to another healthy individual unintentionally or unknowingly. For example, the virus may be transferred by donating blood.
A carrier of HIV may appear to possess a perfectly normal health or one may be subjected to minor ailments, which are otherwise negligible. These minor ailments often are noticeable except in a high-risk population. The late sequel of the disease process is called the AIDS. As can be inferred from the name AIDS is not a single disease. It is a complex medical phenomenon of many associated pathologies.
These pathological incidences are strongly connected with psychological and social disturbances. A person may take seven to ten years to contract a full-blown AIDS disease. Despite extensive medical research, it has not been possible to find a definite cure for AIDS. The available medicines are merely palliative in nature used to lower the speed of the disease process and contribute to improvement in the quality of the life of the patient as much as possible.
AIDS has been discovered in early 1980s and since then the proliferation of the disease has shaken the entire world. According to research on the genetic details of HIV, the virus has been found to be older than probably a century. Until the mid 1970s, there has been only 0.001% of the total population of the world, which was infected by HIV. The rapid social changes that took place in several parts of the world after 1970 have made the HIV surge. Factors like urbanization in African countries, economic and social globalization involving increased traveling by people all over the world, flood of intravenous drug users in the United States and Europe have accelerated the spread of the virus among many people. Changing sexual practices was another important reason for the increased incidence of HIV infection.
AIDS leads to the progressive loss of CD4+ helper/inducer cells in the human body. These cells are important subset of T.Lymphocytes, which are responsible for the functioning of vital functions in the immune system of the human body. Severe immune suppression is the main consequence of AIDS. It also leads to constitutional disease and neurological complications. In addition, opportunistic infections and neoplasm are also the result of AIDS in persons with intact healthy immune function. The specific means that leads to the ruining of the immune system has not been completely defined. Nevertheless, abundant scientific reports and data evidence the finding that the infection with HIV is the underlying cause for the contraction of AIDS by human beings.
The consequences of HIV/AIDS have made the disease a global epidemic requiring increased focus and provision of healthcare to contain the spreading of the infection. The increased responses to the containment of HIV epidemic have obtained global attention on dealing with not only the cause of the epidemic but also with its consequences on human health. The consequences are referred to as the “impact” of AIDS disease.
In the past, there has been lack in the global approach to handle the cause and consequences of the socio-medical problem like AIDS. However, with the alarming consequences of the spreading disaster of HIV, new global strategies have been evolved towards dealing with the cause and impact of the disease in an effective manner. The strategies have the objective of decreasing or preventing the spread of the infection among different communities. HIV has become a major cause of adult mortality in many countries. The effects of this epidemic can be psychological, social, and economic deterioration apart from causing major disturbances to individuals and their families.
Origin of HIV/AIDS
The issue of the origin of HIV has to be addressed from beyond a purely academic perspective, to gain an understanding about the ways in which the virus originated and the ways in which it evolved. This understanding is crucial in the development of a more effective treatment of the disease in the future by developing an appropriate vaccine against HIV. The knowledge on the origin and emergence of AIDS becomes important for mapping the future course of the epidemic and for developing effective interventions to contain the spreading of the infection.
HIV virus is a part of the group of viruses known as lentiviruses (Pelchen-Mathews, 2003). This group of viruses is found in a number of other primates other than human beings. These viruses as a group are known as simian (monkey) viruses (SIV). In this case their origin is normally denoted by a subscript.
The fact that certain viruses can cross over to human beings from animals is known for a long period and this process is referred to as zoonosis. HIV has been concluded to have crossed over from chimpanzees to human beings, when a human killed a chimp and have eaten it for food. There are researches, which have concluded that HIV has crossed over iatrogenically via medical experiments. One of the well-publicized theories has indicated that polio vaccine has played a significant role in the transfer of the virus.
Demographic and Health Effects of HIV/AIDS
Countries that have been hit hard by the epidemic of HIV/AIDS have suffered from problems like surge in mortality rates and drop in the life expectancy rates. Nevertheless, because of high fertility of the women with more average number of births per woman, the countries in sub-Saharan African region, which have lesser number of people living has not been affected by HIV/AIDS and there has been no reduction in the number of people. In other nations of this region, the growth in population has shown a dramatic decline or the growth has ended. However, the total increase in number of people in this region surpasses other regions of the world.
Even after taking into account, the AIDS-related mortality, the population of the African countries is expected to increase to more than 1.5 billion in the year 2050. AIDS has had a devastating effect on the well-being of the societies. HIV/AIDS has ranked fourth in the causes for death across world and the epidemic stands first as cause of death in sub-Saharan African region. In the year 2005, UNAIDS has arrived at a figure of 3.1 million adults and children, who died because of this epidemic and of whom more than 2 million deaths occurred in the sub-Saharan Africa including South Africa.
People affected by HIV/AIDS are susceptible to developing other illness and infections easily because of the suppression in their immune system. Consequently, the AIDS epidemic has increased the incidence of pneumonia and tuberculosis in many of the countries including South Africa. The mortality rates among children under the age of 5 years are significantly higher than what would have been without AIDS. Without adequate life-saving drugs, one third of the children born with AIDS transmitted through their mothers die within one year of their birth and almost 60% of the children die before the age of five.
The increase in the deaths caused by AIDS has resulted in reduced living year rates among countries. The effect of AIDS-related deaths has been felt on the age structure of the population in the severely affected countries such as South Africa. In developing nations where there is low levels of HIV and AIDS, most of the deaths happen among people with either extreme of ages. However, where there is higher incidence of HIV/AIDS, the disease primarily strikes adults during their prime-working age. This means that people who are young adults or adolescents are the ones who are affected by the epidemic. This incidence shifts the usual pattern of deaths and distorts the age structure in those countries where HIV/AIDS has predominant prevalence.
Since AIDS, deaths occur mostly in the 25-45 age group, communities having high incidence of the epidemic tend to lose disproportionate number of parents. There will be a high toll among experienced workers, which creates gaps that the society will find it difficult to fill. Women are more vulnerable than men are to the ill effects of the epidemics in some of the regions. Deaths occurring among women leave the families without the prime caregivers. In the sub-Saharan Africa, where heterosexual contacts are the main reason for the spread of the virus women are infected at higher rates than men are.
“Households experience the immediate impact of HIV/AIDS, because families are the main caregivers for the sick and suffer AIDS-related financial hardships. During the long period of illness caused by AIDS, the loss of income and cost of caring for a dying family member can impoverish households. When a parent dies, the household may dissolve and the children are sent to live with relatives or left to fend for themselves” (Johnson, 2009).
Healthcare systems also are affected largely by the enormous demands for treatment of HIV/AIDS epidemics. The epidemic has crippled the health system in South Africa, where the health systems were already weak before the spread of epidemics. Expenses incurred for the treatment of the epidemic has increased alarmingly because of the opportunistic infections caused by AIDS. Allocating more resources for treating HIV/AIDS has reduced the resources available for other health concerns. With public funds for health care becoming scarce, the healthcare costs for treatment of HIV/AIDS are increasingly thrust on the private sector and households and individuals are made to take the burden of treatment.
Business and agriculture are some of the sectors that are affected seriously by HIV/AIDS. There are serious concerns to the employers in the form of loss of workers, absenteeism, increasing costs of extending healthcare benefits including the provision of drugs for AIDS and the settlement of death benefits. Loss of farm workers affects the economic viability of small firms and there is compromise of commercial agriculture. According to a study by Food and Agricultural Organization (FAO) in ten African countries, which are most severely affected by HIV/AIDS, there will be a reduction of agricultural workforce between 10 percent and 26 percent by 2020.
Because of the adverse impact of HIV/AIDS on the business and agricultural sector the economic stability of the nations are affected largely. In many highly affected countries such as South Africa, it is estimated that there would be a loss of 1 to 2 percent of annual GDP as compared with a hypothetical situation where there is no AIDS. The longer-term impact may be more serious than estimated by the analysts. “It is difficult to account for the loss of human capital as children’s education, nutrition, and health suffer directly and indirectly due to AIDS. The effects of lower investments in the younger generation could affect economic performance for decades” (Ashford, 2006).
Salient Features of South African Healthcare System
HIV/AIDS will have its impact on the health sector because of two reasons –
- it will result in an increase in the number of people seeking healthcare services and
- it is expensive to provide health care services to AIDS patients than for most other illnesses or diseases.
The governments may have to face with trade-offs along at least three different dimensional aspects. They are
- treating HIV/AIDS patients versus preventing the further infection of the disease,
- treating HIV/AIDS patients versus treating people for other diseases and
- public spending for promoting health versus spending for other social objectives.
The governments are obligated to maintain a healthy population which is an important objective on the own right of the government, which is also crucial for the economic development as a productive workforce is essential for rapid development of the economy.
Different hospitals in the country report on large number of patients admitted with HIV/AIDS disease. For instance, in Durban 40% of the adult medical in-patients were admitted with HIV-related illness in the King-Edward VII hospital during 1997 and this situation has worsened over the years. The percentage of HIV-related patient admissions in another province of Guateng varied between 26 and 70 percent during 1997.
In another Hospital in Soweto 30% of the children under the age of 6 years admitted were infected with HIV. A case study conducted with respect to a rural hospital in the province of Hlabisa reports that there has been dramatic increase in the total number of admissions during 1991 to 1997 and this increase was in the region of 57%. Out of the patients admitted, 55 percent of the adult medical patients were reported to have HIV infection, 42 percent of the females and 26 percent of the children admitted were reported to have been infected by the disease.
“A cost-effectiveness analysis undertaken there found that the number of maternal transmission cases would be reduced by 11 percent at a cost of US$53,509, and would be reduced by 37 percent at a cost of US$263,510, by following a course of antiretroviral therapy during pregnancy. The study concluded, however, that finding these funds would be very difficult” (Bollinger & Stover, 1999).
An unpublished study estimated the costs of AIDS treatment reported that the cost would vary between US $ 21,800 and US $ 43,700 per case on an average over a period of 13 years. The study also reported that only a small percentage of the population could really afford to receive the most comprehensive treatment and 40 to 50 percent of the population might not receive any treatment at all. 20 to 25 percent of the population who are working in informal sectors of the economy might receive treatment to a limited extent and 12 to 20 percent are likely to receive adequate treatment. Another recent study estimated the cost of antiretroviral therapy to cost anywhere between $ 60 and $ 600 per month and most of the South Africans suffering from HIV/AIDS might not afford this cost.
Status of Public Healthcare
Literature from countries across the world suggests that the provision of healthcare in developing countries such as South Africa faces similar challenges in respect of cost to quality ratios. These challenges have an impact on the perceived quality of service extended to patients as a component of the general healthcare service provisions (Ramani, 2004; Mostafa, 2005). There are wide variations in the expectations and priorities on the healthcare service delivery in different countries.
These expectations and priorities often are linked to the cultural background and the prevailing healthcare systems. Eiriz and Figueiredo (2005) and Sajid and Baig (2007) are of the opinion that the healthcare service providers have to maintain a higher level of service quality and at the same time they should take up the responsibility of monitoring the expectations and experiences of the patients on a continuous basis. In the context of South Africa and several other developing nations, the state is the primary provider of health services. This position of the state makes the patient in a government-controlled hospital as the primary client.
Consequently, assessment of the services provided by the state hospitals and recommendations made based on such assessments will help the managers and policymakers of the hospitals to render higher quality service to the patients and meet their expectations. However, the aspect of balancing between the quality and cost elements is of importance in taking decisions for providing effective service in the context of developing countries.
South Africa as a developing country with the non-homogeneity in its population consisting of several cultural groups has been challenged with specific transformation issues, characterized by several swift changes. Since the end of apartheid, the government of South Africa has faced the challenge of providing equitable access to quality healthcare to a majority of its population. The healthcare system in South Africa remains under-resourced and over-used despite the consistent attempts of the government to bring major transformation to the existing healthcare system.
One can observe significant differences in the quality of healthcare services provided by the government and private healthcare service providers in almost all the countries (Jabnoun and Chaker, 2003). This difference will be more in the emerging nations. The healthcare system in South Africa is not an exception where the difference in the quality of healthcare service provided by the government differs greatly from that provided by private sector.
The healthcare system of South Africa is made of a huge state organization and a comparatively smaller private operations. However, the private sector is fast growing in providing services to the people. Healthcare takes many forms including basic primary healthcare, which is offered free of cost by the government extending up to highly specialized healthcare services provided using hi-tech facilities in the private sector. Such hi-tech facilities are provided to those people, who can afford to such services.
While the public sector healthcare services remain under-resourced and over-used, the fast-growing private sector, which is run purely on a commercial basis, extends services to the middle and high-income earners. People in these income-groups are in general members of various medical schemes and this segment constitutes 18% of the total population. The private sector extends healthcare services to foreigners, who are keen in getting top-quality surgical services at affordable prices. A majority of healthcare professionals of the country prefer to work with private sector, as it is lucrative for them.
Even though, the government provides for more than forty percent of the total healthcare costs, the public health department is subjected to constant stress, as it has to provide services to more than three fourths of the people. Barring this fact, majority of the funds are utilized in the private health segment, which caters to serve only 20% of the total people of the country. Under apartheid all, the best medical care facilities were reserved for taking care of the needs of the white minority. Although this situation was changed after apartheid, the conditions in public hospitals have remained same without improvement.
With large number of poor and unemployed people, the government has to take a heavy responsibility for providing health services. In addition to the problem of ageing of healthcare facilities, which require repairs or replacements, the HIV/AIDS epidemic of the country, which is the largest in the world has put enormous strain on the public healthcare system. The system is more strained because it is fragile with its overwhelmed and underfunded hospitals and clinics. An estimated one-eighth of the population is HIV positive and requires constant medical attention. This has made South Africa the highest spending nation on healthcare among other African countries. According to World Development indicators for the year 2008, the country spends 8.7% of its GDP on medical care for the people.
The problems in the public healthcare are compounded by the fact that medical professionals prefer to work in private sector because of the low wages offered by the public sector and they leave public sector. “The South African Medical Association’s report in 2008 said doctors in the public sector were underpaid by up to 200 per cent compared with their counterparts in the private sector” (Mutasa, 2009).
Challenges facing the Health System
After the first elections in South Africa held in the post-apartheid during 1994, the healthcare system of the country was not organized properly to meet the needs of the total people living in the nation. During the apartheid, a vast majority of the public represented by black South Africans were not able to access the healthcare services. After the elections, the inheritance of disparity existed with a central health department, which lacks adequate health care service provisions and hospitals in a number of villages and local areas. It was the objective of the new democratic country to bring a complete change in the healthcare system.
Healthcare for pregnant women was provided completely free. The cost of healthcare services to the rest of the population was subsidized on a sliding scale and the costs payable were to be decided on the financial position of the individual and his ability to pay for the service.
In the present day’s context, South Africa provides primary healthcare mainly using a number of local clinics. The government has built or upgraded more than 1,600 medical centers between the period 1994 and July 2007. South African government functions under a federal set up and the central public health services division establishes the procedure of care; but the local authorities are made in charge for providing the healthcare to the public. As noted earlier, 20% of the population access private sector for their healthcare needs.
Despite the intentions of the democratic government of South Africa to provide complete medical care, the public healthcare system continued to remain overburdened since its inception. The system has not caught up with the total health needs of the country. The assessments made by the health officials of the government and the Health Systems Trust, an independent health policy and research institute of South Africa reveal that the health system is overburdened because of the magnitude of the population it intends to serve. The public healthcare system has to face the challenges of lack of adequate facilities, poor resources and lack of adequate medical personnel.
The complexities in extending healthcare to a country with a large number of unemployed people were multiplied, when the HIV/AIDS epidemic infected a large proportion of the people and the incidence went unattended for a long period. Only in the year 2003, the South African government proclaimed that antiretroviral treatment to HIV affected people will be extended. This could be achieved only after a long campaign by different AIDS campaigners and activists.
However, the consequences of the delayed response by the government to the epidemic were severe. A report was published in the Journal of Acquired Immune Deficiency Syndromes in October 2008 on the findings of a study conducted by Harvard School of Public Health. The report indicates that more than 330,000 people have died in South Africa between 2000 and 2005 and these deaths have been caused by the inaction of the government to put into practice a suitable antiretroviral treatment program to protect the people from infection.
Department of Health states that despite South Africa having the huge antiretroviral program, the country has also a large number of people affected by the epidemic. As pointed out by a report of the Health System Trust in 2008, during the year 2007, 42% of the 889,000 South Africans who tested positive to HIV started treatment only in 2007. The South African healthcare organization suffers from a significant disadvantage of lesser number of health work force.
According to the organization “Doctors Without Borders,” the private sector offers higher salaries to the doctors and employs more than fifty percent of the doctors of South Africa. Private sector also employs more than two-thirds of the nurses, which has created a severe shortage of labor in the public health care system. Some of the most talented doctors leave the country to work in other countries for higher compensation.
Changes in the Healthcare System as a result of Incidence of HIV/AIDS
Impact of Increased Incidence of HIV on Healthcare System
For the reason that HIV/AIDS largely affects the lives of the people in South Africa, it becomes essential to talk about the impact of HIV/AIDS on the health system of the country. The last decade between 2001 and 2009 witnessed a certain amount of stability in the prevalence of the disease in the country. The proportion of the population in the age range of 15to 49 who were infected with HIV rose from 15.3% to 17%, which is comparatively lower. The percentage of people who test HIV positive in the total population increased by one percentage point from 9.3% to 10.6% during the same period, which amounts to a total population of about 5.1 million people in the country (Statistics South Africa, 2009).
Nula (2000) observes that this disease has been an undercurrent influencing all facets of the lives of the people in South Africa. At one point of time, it was feared that there will be only very less number of Blacks, who would reach old age because of the incidence of HIV/AIDS. This position was supported by the life expectancy report for the year 2008. Barron & Roma—Reardon (2008) note the expected life years of Black people was less by 22 years as compared to White people and less by 18 years as compared to Asian people.
The political leadership in South Africa ignored the dangers of the spreading of HIV/AIDS for many years after the African National Congress came to power in 1994. Mandela was given the insurmountable task of converting South Africa in to a democracy, in which the prevention of HIV/AIDS was given a least priority. The then President Thabo Mbeki’s disagreement to the issue resulted in the epidemic unattended resulting in certain devastating period, during which all programs to contain the spread of the disease were disregarded. There was sheer confusion about the disease and the spread of the virus resulted only in fear and stigma associated with it. This allowed the prevalence of the virus to grow into an epidemic, which the country is still fighting against (Barron & Roma-Reardon, 2008).
According to the report of the Health Systems Trust (2009), since 1994 there were many policies and regulations implemented to reduce the health disparities that were in existence during apartheid era. However, the trend towards increased equity that was prevalent during the first five years appears to have suffered a decline. The National Health Accounts Project disclosed that the country experienced a reduction in the spending on healthcare per person since the year 1997.
An enlarged disparity in regional reserve allotment was also witnessed and even spending per person on primary health decreased since 1997. There was a major transformation of the local governments to establish a District Health System (DHS). The government implemented the Municipal Structures Amendment Act of 2000 to transfer significant amount of powers on provision of healthcare to the regional authorities, with a view to set up the DHS. The objective of this move was to allow the regional governments to hold more power for the provision of public healthcare.
There was a strong opposition for this move, as it was believed that this would promote further fragmentation of the health system. “In order to address this issue, the Minister of Health and Members of the Executive Council for Health demarcated the new local government boundaries. The number of municipalities was reduced from 834 to 285. Although this made sense conceptually to reduce fragmentation, it created its own challenges. Some health districts were now too large to be manageable and had to be divided into smaller sub-districts.” (Kon, 2010)
“According to the 2000 South African Health Review, the move to a District Health System caused not only confusion, but duplication of services, wasted effort and time, and has had a negative impact on the morale of already overburdened health workers , specifically those in the public health care sector” (Kon, 2010; Ntuli, 2000).
As pointed out by the South African Health Review (2008), the public healthcare sector in South Africa continues to remain under-funded and under-staffed. Inequalities in healthcare provision and financing among various zones characterize the system. There are ensuing inequalities between the public and private sector healthcare delivery. There is the additional force of HIV/AIDS and other infectious illnesses on the healthcare provision. Despite these pressures and challenges, the government has introduced certain measures, which are likely to have an impact in the long run.
“Some of these include: the Nursing Act of 2005 that introduces community service for nurses, the mandate for community service for new doctors, the establishment of rural and scarce skill allowances to attract and retain health workers in rural areas, the creation of the National Community Health Worker Policy Framework (NCHWPF), which provides community health workers to primary health facilities, and a new wage structure for nurses.” (Kon, 2010).
The healthcare system of South Africa is struggling to respond to the burden of the devastation caused by the epidemic of HIV/AIDS. At the same time, the system has been respecting its post-apartheid directive of providing equitable healthcare services to all the citizens.
There has been significant and alarming increase in the dimensions of HIV/AIDS epidemic in South Africa. It includes the prevalence of HIV in adults up to 18.1% of the population, which amounts to an estimated 5.7 million people living with HIV/AIDS. It also had the impact of a drastic fall in the life expectancy. With these ramifications, the healthcare system which is already under-resourced up to a marked level, has been put to severe pressure because of the fact that an increasing number of people are in need of care and treatment for HIV.
There has been prevalence of HIV among doctors and nurses at the same level as it is found among the general population. This has led to increased rates of ill health and absenteeism among those people who are responsible for providing the required healthcare services. This situation combined with a brain drain of the medical professionals has resulted in a vicious circle, in which the epidemic causes a crisis in the health workforce and at the same time the inadequacy of health workforce works as a major impediment in the prevention and treatment of the disease.
These problems facing the South African healthcare system, which are unparalleled and caused by the increased incidence of HIV, have forced the government to rethink and reorganize the health care system completely. It also resulted in a reevaluation of the responsibilities of nurses in providing medical attention in major diseases. Traditionally the healthcare system of South Africa has been based on the services provided mostly by nurses.
The nurses are more in numbers as compared to doctors with a ratio of 5 to 1. Despite the fact that the nurses attend to the healthcare needs for a large number of people, it has become evident that the nurses do not possess adequate authority and they lack resources to perform their functions efficiently. “This has become starkly evident within the context of HIV/AIDS, where expanded training, task shifting, and remuneration, as well as revision of regulatory and legislative policies have been necessary to enable nurses to respond effectively to the epidemic” (Jennifer et al, 2009).
“The widespread implementation of interventions to prevent mother-to-child transmission (PMTCT) in 2002 and to provide antiretroviral therapy (ART) in 2004 initially focused on physician-led services at the tertiary level. Nurses were charged only with diagnosing HIV infection and referring patients up to higher levels of the health care system” (Jennifer et al., 2009). However, this system has been found to be of no practical utility, because of the fact that the prevalent health care system was mostly taken care of by nurses, in which the nurses provide services to a large number of people in the local areas.
“Increasingly, the scale-up of HIV services is being reconceptualized to match both the urgent need for prevention, care, and treatment and the national vision of decentralized primary health care. Of note, HIV scale-up has triggered innovations in nurse training, task shifting, retention, and scope of practice that need not remain HIV-specific. Lessons learned in the context of HIV have the potential to enhance nursing practice and human resources for health more generally, strengthening South Africa’s health systems and improving access to effective health services” (Jennifer et al, 2009).
Changes in Role and Responsibilities of Nurses
Training of healthcare professionals including nurses has become an urgent need with the emergence of the new epidemic. Developing knowledge and expertise on the prevention and treatment of HIV among the healthcare workforce has become a national priority, which was highlighted in the National HIV/AIDS Strategic Plan of the government of South Africa. Accordingly, the government introduced new qualifications in PMTCT and ART for nurses and the training was conducted mostly by NGOs. In the healthcare system, which shaped up after the increased incidence of HIV/AIDS, the newly qualified nurses started playing a significant role with their knowledge and skills relevant to HIV.
In the reorganized healthcare system, these nurses are made responsible for directing HIV testing and counseling services. They also prepare the patients for receiving ART therapy initiation and they diagnose and manage the side effects of the medication and therapy. The nurses collaborate with midwives to provide PMTCT services to the pregnant women in perinatal period. They are also responsible for providing early infant diagnosis services. “They refer up those who need ART initiation and those with advanced illness and complications” (Jennifer et al., 2009).
Development of Healthcare Workforce
In South Africa, after a severe burden was felt on the healthcare system, the government embarked on the development of new cadres of healthcare workers with the objective of providing “patient education, counseling, adherence support and community outreach.” For example, there are “lay counselors” who are entrusted with the job of conducting sessions for voluntary testing and counseling services for the patients on a group and individual basis. They are also mandated to teach the people about HIV and its prevention. They also teach the need for HIV testing and clinical follow up.
“These counselors, who are supervised by nurses, also provide a critical link to the community on issues of disclosure, safer sex practices, reducing stigma, and adherence to treatment. Peer educators have also played key roles in HIV programs. In the mothers2mothers program, HIV-infected mothers are hired to mentor pregnant women newly diagnosed with HIV. These mentor mothers identify themselves in antenatal clinics as HIV positive, using their own openness to break barriers of silence and stigma” (Jennifer et al. 2009).
The mentor mothers provide an exclusive support by conducting individual and group counseling sessions. This way the nurses’ time is made free to concentrate on the medical care to pregnant women. Although the increase in the new class of employees makes the nurses free from non-clinical jobs, such appointments increased the responsibility of the nurses to oversee the work of these employees.
Constraints in Improving the Healthcare System
After a prolonged period of state denial and poor implementation of policies and programs to improve public healthcare, there has been a decision to scale up antiretroviral (ART) therapy. The new resolve also included the improved access to condoms and improved control on tuberculosis. The government in the year 2003 decided to enable the public to have free access to ART. After this decision, approximately 488,439 people have enrolled within 4 years (Abdool Karim et al., 2009). The coverage for ART rose from 4.9% in 2004 to 40.2% in 2008 (Adam & Johnson, 2009). There was still a problem with these improvements, in that they were not felt equitably.
Most rural provinces such as Limpopo and the Eastern Cape Province, which experience persistently high level of poverty were the ones that had the lowest levels of ART coverage (Hoogeveen & Ozler, 2006). On the other hand, urban provinces were getting better coverage. At the same time, urban access to HIV, services remain highly inequitable. Such access varies from place to place in the cities. For instance, residents of urban informal settlements, many of whom represent the internal migrants from rural areas find it difficult to access the required healthcare services for treating/preventing HIV/AIDS (Vearey et al. 2010).
According to Kober & Van Damme (2004), there are constraints to equitable ART delivery in the form of “weak capacity of health systems, poor district and facility management and the migration of skilled health service personnel.” There are other factors affecting the provision of healthcare service such as poor drug distribution and an inadequate culture of service delivery (Schneider et al., 2006). The objectives of HIV/AIDS and STI strategic plans of the government for the plan period 2007-2011 are to bring down the HIV incidence rate by 50% and to implement ART to 80% of the population who are in need of ART coverage. However, the government was unable to reach these targets, because of the fact that long-standing inequities continue to have significant influence on the distribution of the healthcare services properly to the needy people.
Migration of people from villages to cities exacerbates this issue, since most of the skilled people leave rural areas migrating to urban areas. In addition, migrants moving to urban areas normally enter the city through informal settlements located in peripheral areas. These settlements present a wide range of health risks including prevalence of HIV at higher rates coupled with poor access to healthcare. Those migrants who are infected with HIV and possibly facing death due to HIV or tuberculosis decide to return to rural areas from where they originally migrated (Clark et al., 2007). “These added dimensions have a profound impact on the effectiveness of equitable health planning in both urban and rural places, including the provision of ART services” (Collinson et al., 2010).
Strategies for Effective Management of HIV/AIDS by the South African Healthcare System
As a response to mitigate the crisis of the epidemic HIV/AIDS in South Africa, there is the need to undertake a critical task of developing scalable systems to ensure sustainable and effective delivery of antiretroviral (ART) drugs in a variety of settings, which are acutely resource-constrained.
Managing HIV/AIDS as a Chronic Disease
With the administration of modern ART treatments, the country can expect higher survival rates. However, there needs to be an effective management of patients who qualify for ART treatment. This entails a lifetime commitment by both patient and providers in the complex treatment with significant side effects. A system of efficient chronic care calls for a comprehensive clinic redesign. It also involves a division of labor that allows non-physicians to assume greater responsibility for the routine care of the patients. While the HIV/AIDS epidemic presents a unique set of challenges, in order to ensure a prolonged and healthy survival of patients treated with ART, a comprehensive management strategy should be developed.
An effective management strategy aims at increasing the number of “informed, activated patient population and knowledgeable, proactive, protocol-driven care providers” who would be able to work in aiding the treatment of HIV infected population. For this, the design of care in the clinic should take into account the different needs of the patients and in the process utilizing the spectrum of the skills of the personnel available in the clinics. The strategy should be to accomplish the six attributes of care – care, which is patient-centered, effective, safe, efficient, timely and equitable.
Redefining Health Care Organization
The introduction of new health services stresses an already overburdened health system. In this situation, the introduction of effective disease management practices for ART treatment delivery enables the strengthening of the system. For facilitating this process, the healthcare leadership must make an excellent HIV/AIDS care an objective of the health system. The leadership should provide adequate resources to initiate continued ART care. For example, the resources should include provision of data systems, data entry personnel and counselors. The healthcare leadership should remove the barriers to clinic redesign and provide active support for the implementation of ongoing treatment of ART programs.
Designing Clinic System
The clinics are the transition point for changing the palliative care of AIDS to comprehensive management of HIV/AIDS. As a strategy for effective management of HIV/AIDS, there must be a redesign of the structure of the care delivery needs. While many of the initial phases of ART rollout in South Africa are mostly doctor-based, a more nurse-based focus is needed, since the service delivery is covered more by primary care settings.
“New and existing patients who are being prepared for ARVs will have different needs from patients who are being seen repeatedly for ARV maintenance therapy, or patients with HIV who do not qualify for treatment. Patients on chronic therapy can be triaged in streams that stratify patients who need routine care and surveillance (‘fast-track’) from those who require more complex care or a change in management (e.g. consideration for up- and down-referral)” (Barker, 2004).
There must be a reassessment of the role of different caregivers. This would enable an assessment of additional resources, which are needed to increase the clinic capacity. When the clinics become overburdened and progressively more dysfunctional, the caregivers will be made to burdened with inappropriate task. Therefore, there is the need to define the role of every member of the care unit. This will significantly enhance the efficiency of the clinic.
Improving Clinic Protocols
The management must encourage the clinics to adopt the best available guidelines for providing ART therapy and HIV care. The clinics should have instituted clear algorithms for better disease management. Patient encounter forms can be introduced to support these algorithms by enabling collection of proper information and to provide prompt care considering the specific needs of the patient’s treatment stage. It is also important that the protocols should be updated and adapted on a periodic basis through a systematic process, which is facilitated by the data collected in the clinic.
Encouraging Patients to adopt Self-Management Support
Management of HIV/AIDS can be made more effective by encouraging patients to take an active role in the management of their disease. A process must be established whereby patients become informed and involved in to routine clinic management, with the use of counselors and teaching sessions. It is necessary that self-management strategies are documented and reinforced in the subsequent visits of the patients to the clinics. Certain forms of standardized assessment of the knowledge of the patients and barriers to the addition of their knowledge can promote better-designed service delivery. There must be sufficient motivation to the patients and their adherence to self-management initiatives can be enhanced by enabling them to watch improvements in their disease indices.
Increased Use of Community Resources
In addition to the support from the health services, increased use of community resources will also help in improving the effectiveness of the management of HIV/AIDS in the country. The community organizations can help in various activities like support for disclosure, stigma reduction, assisting in palliative care and adherence support. When the clinic care is linked with community resources, there will be an effective chronic disease management. The organizations may undertake increased home visits and partnerships with community activity groups will help improving an effective service delivery.
Prevention Strategies
The objectives of any prevention program are to reduce the risk behaviors and to address vulnerability. An effective prevention program must be capable of understanding and addressing the behaviors of peoples and must address their vulnerabilities. The prevention programs must involve and evolve out of the same community, the behaviors of which the programs aim to amend. There must be multiple partners and components to address the multiplicity of the issue on hand. It is to be understood that real prevention is not an easy affair but a complex task. An effective AIDS prevention program should be capable of working at various levels, which include the patient level, groups of personal level, communal level and societal level.
The efforts on preventing HIV/AIDS can be made fruitful by increasing the awareness of the people and nurturing positive attitude towards prevention tools such as use of condoms. Positive practices such as delayed sex and avoiding multiple sex partners will also help preventing the increased incidence of HIV/AIDS. The bio-medical prevention strategies are comparatively better and effective in preventing the spread of HIV/AIDS.
These include male circumcision, Highly Active Antiretroviral Therapy (HAART), prevention of mother to child transmission (PMTCT), use of condoms by both males and females, treatment of sexually transmitted infections and administration of HIV vaccines. These prevention strategies to be more effective need the understanding and cooperation of the people likely to be affected by the epidemic. In order to get the voluntary cooperation of the people for the biomedical prevention it becomes important to enhance the knowledge and awareness of the people on the evil effects of HIV.
In the opinion of the researcher, educating the people of South Africa is the toughest task because of high level of illiteracy among the people. The stigma attached to positive testing of HIV among the pregnant women is the main cause for the transmission of the disease to the infants. In this, respect the hiring of women who are HIV positive as mentor mothers to provide counseling to the women who visit the clinics appears to be an effective strategy for prevention of HIV/AIDS.
There are some behavioral HIV prevention strategies, which are also found effective, which also involves the voluntary cooperation of the people. These strategies include Abstinence only or ABC approach, voluntary counseling and testing and reducing multiple and concurrent sexual partnerships. The Abstinence only strategy includes
- “Abstinence for youth, including the delay of sexual debut and abstinence until marriage
- Being tested for HIV and being faithful in marriage and monogamous relationships
- Correct and consistent use of condoms for those who practice high-risk behaviours” (Linney, 2007).
Apart from biomedical and behavioral prevention strategies, another form of prevention was tried in the form of structural HIV prevention strategies where a microfinance program with a gender and HIV training curriculum was put to practice. This type of prevention strategy has not taken effect because of lack of financial resources.
There are different approaches to the implementation of prevention strategies of HIV namely, bio-medical approach which includes assessment, diagnosis and prescription. There is a public health approach, in which there is the need for awareness and knowledge about treatment and support for HIV infection. This requires a behavioral change communication (BCC) and the government should evolve a strategic framework for improving the communication with the public. BCC is an integral part of a comprehensive HIV/AIDS prevention, care and support program. The BCC has a number of interrelated roles to play in effective prevention of HIV/AIDS.
Effective BCC has the ability to increase knowledge, stimulate communicative dialogue, and promote changes in attitude, which are essential to ensure an effective prevention, reduce the stigma and discrimination, and create a demand for information and services. In effect, BCC can promote services for prevention, care and support.
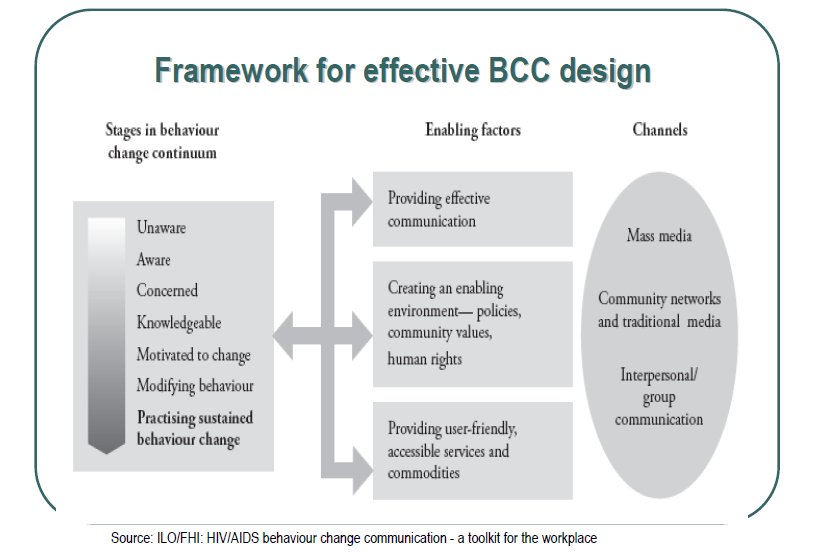
The above figure represents the framework for an effective BCC design for prevention strategies for HIV/AIDS. It is advisable to implement a combination prevention strategy, which includes successful HIV behavior-change programs. The combination strategy will deliver a combination of risk-reduction strategies, which are proven scientifically. These include one-to-one counseling, programs for small groups and community education. The community education is expected to encourage people to adopt safe sexual practices and to avoid drug uses.
The challenges facing behavioral change for prevention of HIV incidence include making the people accept for HIV testing and restricting people from indulging in risky behavior where the HIV prevention is in advanced stage. For accomplishing this, HIV prevention counseling and services must be made a regular part of the treatment for people with HIV.
Conclusion
With the continuing spread of HIV/AIDS and in the absence of a vaccine or definite cure for the disease, prevention appears to be the key strategy for containing the spread of the epidemic in South Africa. The most common reason for the transmission of HIV virus is the sexual contact. Therefore, HIV prevention can be attempted only by altering the men and women’s sexual behavior and ensuring reproductive health.
Effective prevention programs encompass such interventions, which could promote “abstaining from sex, delaying the onset of sexual activity, staying with one mutually faithful partner, limiting the number of sexual partners, consistently and correctly using condoms and counseling and testing for HIV.” The most effective combination of interventions out of these mentioned above depends on the characteristics of the group of people who have been infected with HIV. It is also necessary to consider the social, economic and cultural factors acting on applying these interventions to make the prevention programs effective.
Another key intervention to curb the spreading of the epidemic is to prevent the transmission of HIV from mothers to children. This program is an effective one in the way of saving lives. Similarly, it is possible to prevent several positive-HIV births by helping the HIV-infected pregnant women to avoid unintended pregnancies. Increased use of contraceptives to restrict such pregnancies can be considered as a cost-effective intervention than providing ART therapy during delivery and to the newborn babies of HIV infected mothers.
One of the key challenges for the future is to control the speed of the further spreading of the epidemic among infants and young adults and providing equitable treatment to millions of people already infected by the virus. In this respect the communities, government and society must ensure that prevention remains the key focus in the AIDS control programs, even then equitable treatment is extended to all the affected people.
The government must ensure that the health infrastructure is improved and the capacity to provide adequate and proper health services is enhanced. The government should work towards achieving the broad goal of reducing poverty, illiteracy among the people and it must focus on monitoring other social, economic and political factors, which work to increase the vulnerability of the people to be infected by HIV. More than anything else, the government and communities must work towards reducing the stigma and discrimination against those people who are living with HIV.
References
Abdool Karim, S.S., Churchyard, G.J., Abdool Karim, Q., & Lawn, S.D. (2009). HIV Infection and tuberculosis in South Africa: an urgent need to escalate the public health response. The Lancet, 374, 921-933.
Adam, M.A., & Johnson, L.F. (2009). Estimation of adult antiretroviral treatment coverage in South Africa. South African Medical Journal, 99(9), 661-667.
Ashford, S Lori How HIV and AIDS affect Populations. Web.
Barker M Pierre, McCannon Joe, Venter W D Francois (2004), Managing HIV as a Chronic Disease: Using Interactive Data Collection to Improve Clinical Care. Web.
Barron, P., & Roma-Reardon, J. (2008). South African health. Web.
Bateman, C. (2004). Healers ‘get real’ about tackling AIDS. South African Medical Journal, 94 (2), 74-75.
Benatar, R Solomon., (2004) Health Care Reform and the Crisis of HIV and AIDS in South Africa, The New England Journal of Medicine 351:81,92
Bollinger Lori, & Stover Johh.m (1999) The Economic Impact of AIDS in South Africa. Web.
Clark. S., (2002) HIV/AIDS in Africa, 2002 Lancet, 359 (9322) 1960.
Clark, S.J., Collinson, M.A., Kahn, K., & Tollman, S.M. (2007). Returning Home to Die: Circular labour migration and mortality in rural South Africa. Scandinavian Journal of Public Health, 35(Suppl. 69), 35-44.
Collinson M et al., (2010) Reaching the Invisible: Hidden Links of Ill Health between South Africa’s Cities and Rural Areas. Web.
Dedicoat M, Vaithilingum M, Newton R (2003). Treatment of Kaposi’s sarcoma in HIV-1 infected individuals with emphasis on resource poor settings. Cochrane Database Syst Rev 3:CD003256.
Eiriz, V., Figueiredo, A. F., (2005). Quality evaluation in health care services based on customer provider relationships. International Journal of Health Care Quality Assurance, 18(6), 404-12.
Gandy M, Zumla A, eds. (2003) The return of the white plague: global poverty and the new tuberculosis. London: Verso Press.
Hoogeveen, J., & özler, B. (2006). Poverty and Inequality in Post-apartheid South Africa: 1995-2000. In H. Bhorat, & R. Kanbur (Eds.), Poverty and Policy in Post apartheid South Africa. Pretoria: HSRC Press.
Jabnoun, N., Chaker, M., 2003. Comparing the quality of private and public hospitals. Managing Service Quality, 3(4), 290-99.
Jackson. H., (2002) AIDS: Africa Continent in Crisis. Harare: SAFAIDS.
Jennifer Dohrn., et al., (2009) The Impact of HIV Scale-Up on the Role of Nurses in South Africa: Time for a New Approach . Web.
Johnson, Leigh., (2009) Access to Antiretroviral Treatment in Adults. Web.
Karim Abdool S, Abdool Karim Q, Adhikari M, et al. (2002) Vertical HIV transmission in South Africa: translating research into policy and practice. Lancet 359:992-993.
Kober, K., & Van Damme, W. (2004). Scaling up access to antiretroviral treatment in southern Africa: who will do the job? The Lancet, 364, 103-107.
Kon R Zeida., (2010) Ethnic Disparities in Obtaining Medical Care and Perception of Health Care in Post-Apartheid South Africa. Web.
Linney Claire (2007) DISHA Abstinence-only Program Approach to reducing the Prevalence of HIV. Web.
Morrison, M. F., Petitto, J. M., Ten Have, T., Gettes, D. R., Chiappini, M. S., Weber, A. L., et al. (2002). Depressive and anxiety disorders in women With HIV infection. American Journal of Psychiatry, 159(5), 789-796.
Mostafa, M.M., (2005). An empirical study of patients’ expectations and satisfactions in Egyptian hospitals. International Journal of Health Care Quality Assurance, 18(7): 516-532.
Mutasa Haru (2009) S Africa’s Healthcare Challenges. Web.
National Department of Health, (2008), The National HIV and Syphilis Prevalence Survey South Africa. Web.
Ntuli, A. (2000). South African health review 2000. South Africa: Health Systems Trust. Web.
Pelchen-Matthews, A., B. Kramer, and M. Marsh. (2003). Infectious HIV-1 assembles in late endosomes in primary macrophages. J. Cell Biol. 162:443–455.
Ramani, K.V., (2004). Practical Applications: a management information system to plan and monitor the delivery of health-care services in government hospitals in India. Journal of Health Organization and Management, 18(3), 207-220.
Russell M. 2000. Community Based Care and Support Services in South Africa. Abstract Th Pe B5225. Paper presented at the XIII International AIDS Conference, Durban, South Africa.
SAFAIDS (2007) HIV and AIDS and STI Strategic Plan for South Africa, 2007-2011. Web.
Sajid, M.S., Baig, M.K., (2007). Quality of health care: an absolute necessity for public satisfaction. International Journal of Health care Quality Assurance, 20 (6), 545-548.
Schneider, H., Blaauw, D., Gilson, L., Chabikuli, N., & Goudge, J. (2006). Health Systems and Access to Antiretroviral Drugs for HIV in Southern Africa: Service Delivery and Human Resources Challenges. Reproductive Health Matters, 14(27), 12-23.
Shaw M. (2002) West African criminal networks in south and southern Africa. Afr Aff (Lond) 101:291-316.
Shisana, Olive. (2003). The impact of HIV/AIDS on the health sector: National survey of healthcare personnel, ambulatory and hospitalised patients and health facilities, South Africa. Human Sciences Research Council, 131-134.
South African Health Review. (2008). Health care in south Africa. Web.
Statistics South Africa. (2009). Mid-year population estimates No. P0302). South Africa: Statistics South Africa. Web.
Tawfik, Linda, & Kinoti N Stephen., (2001) The Impact of HIV/AIDS on the Health Sector in Sub-Saharan Africa: The Issue of Human Resources. Web.
Vearey, J., Palmary, I., Nunez, L., & Drime, S. (2010). Urban health in Johannesburg: the importance of place in understanding intra-urban inequalities in a context of migration and HIV. Health and Place, 16, 694 – 702.