Complexity Science and Chaos Theory
Complexity Science and Chaos Theory is a model that explains how different triggers or events catalyze significant changes in a given organization. When uncertainties occur, organizations are compelled to change in an attempt to remain competitive. These developments can be explained using the nonlinear dynamic theory. Ineffective leadership or misbehaviors in a healthcare setting can influence different practices or responses from the workers. For example, discrimination can force nurses to become less effective. Some practitioners might confront the concern in order to deliver positive outcomes. Healthcare institutions are facing numerous issues such as technological changes and workplace arrangements. Such developments or changes can have numerous implications on care delivery (Salmela, Eriksson, & Fagerström, 2013). Leaders can use Complexity Science and Chaos Theory to ensure their units are prepared against such changes.
I can use this model to become an effective charge nurse. The theory can guide me to apply adequate skills such as change management, problem-solving, motivation, empowerment, and critical thinking whenever new issues emerge in the healthcare unit. The concept encourages leaders to bring on board different stakeholders and address the existing hurdles using the concept of critical thinking (Marquis & Huston, 2015). The power of adaptability can be utilized to ensure every emerging change is analyzed and addressed immediately. The ultimate goal is to guide the targeted nurses in the unit to self-organize (Shirey, 2013). With proper support and guidance, workers in a healthcare facility can be prepared to take up new roles, utilize resources, address emerging hurdles, and maximize the health outcomes of their patients. This argument explains why the knowledge acquired from the theory will continue to support my leadership philosophy as a charge nurse.
Organizational Chart vs. Shared Governance Model
Organizational management can take different shapes depending on the existing hierarchy. The targeted organizational chart is characterized by distinct roles whereby leaders offer guidelines to their subordinates. Instructions are implemented to deliver desirable health outcomes. Different departments focusing on various roles are evident. On the other hand, the shared governance model is a powerful model whereby beliefs and core values are integrated (Marquis & Huston, 2015). Unlike in the organizational chart, the model brings together management, quality, education, research, and education roles. The coordinating council fosters communication without any form of hierarchy.
The organizational structure is hierarchical while the shared governance model is flat or decentralized. The chart gives room for unidirectional delivery of messages or instructions. This means that subordinates are monitored by those in senior positions. The shared governance model creates a new environment whereby communication takes place evenly. The communication process is decentralized. These two approaches to organizational management can deliver different goals (American Association of Colleges of Nursing, 2014). The level of decentralization associated with a shared governance model has the potential to maximize the outcomes of more patients.
Forces of Magnetism
The forces of magnetism describe environments whereby nurses’ contributions are taken seriously to maximize service delivery. The first selected force is high-quality leadership. This force outlines effective managerial practices to empower others. The second force one is that of nurses as mentors/teachers. Physicians should always mentor others, create good environments, and focus on new care delivery models. The third magnetic force is continuous quality improvement practices. This force encourages workers to embrace the best strategies, concepts, and evidence-based insights that can result in improved health services (American Association of Colleges of Nursing, 2014). The fourth force is the availability of adequate resources. This refers to nursing experts who can meet the needs of patients. The fifth magnetic force is that of interdisciplinary relationships. The force focuses on collaborative efforts aimed at fostering teamwork.
Magnetic organizations embrace these forces. They create positive cultures and empower workers to engage in lifelong learning. These practices result in high-quality medical services. Non-magnet organizations can use their forces as guidelines to develop superior cultures that can result in efficient service delivery (American Association of Colleges of Nursing, 2014). Topmost leaders should use shared governance models to promote evidence-based practices and foster communication in their facilities. The workers should be empowered to create meaningful relationships (Mindtools, n.d.). Such leaders should also analyze the attributes of magnet organizations in order to make similar improvements.
Group Management for Just Culture
The Regulatory Decision Pathway (RDP) is a model that is applied in healthcare settings to analyze sentinel events and recommend the most appropriate disciplinary actions. The tool guides different boards to determine caregivers’ behaviors and outline new strategies to safeguard members of the public (Lockhart, 2015). The adverse event that occurred in my organization was a medication error. The affected patient had been prescribed a specific medicine that led to drug-to-drug interaction. The issue was analyzed using RDP as follows:
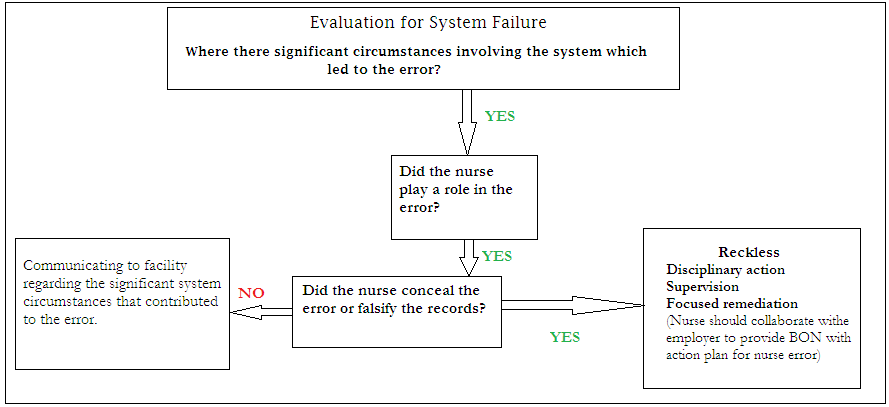
The first step was to analyze the circumstances in the unit that might have led to the error. It was observed that some medications had been mislabeled and placed in the wrong compartments. It was notable that the unit did not have adequate lighting due to power outages. The standby generator in the facility had malfunctioned. The pathway was used to examine if the nurse might have played a role in the error (Terzioglu, Temel, & Sahan, 2016). It was observed that the nurse administered the wrong drugs to the targeted patients.
However, the nurse reported the error immediately and indicated clearly that he had not falsified any journal entry. This analysis indicated clearly that the nurse had not committed the error willingly. This observation encouraged the involved players to inform the facility about the significant unit circumstances that might have led to the error. Since the nurse had not acted in a reckless manner, it was hard to take any disciplinary action against him. However, it was appropriate for the unit to promote adequate practices such as supervision and training to prevent similar sentinel events.
Role Conflict
It is agreeable that role conflict can influence this kind of situation. The presented scenario indicates that the nurse who committed the error was supposed to take care of four patients. Most of these patients required constant attention. The nurse was required to work for over 12 hours. This was the case due to the issue of nursing shortage in the facility (Terzioglu et al., 2016). She was also expected to answer emergency calls. The scenario resulted in role stress and eventually catalyzed the sentinel event.
Principles of a Just Culture
As a group manager, I would handle this sentinel event using the best approaches and principles. The principle of just culture will guide me to focus on employees’ behaviors and not organizational systems. I will remove specific policies that might be affecting the establishment of a just culture. The next step will be to design new procedures to identify and punish individuals who engage in reckless behaviors (Russell & Radtke, 2014). New practices such as drug labeling will be embraced to prevent similar errors. Nurses will be educated to be keen whenever administering drugs. The principles will be applied to promote nurses’ accountability and create a just culture.
Individual Power Plan
As a charge nurse, I have managed to take up various leadership roles successfully. This practice is guided by my personal sense of power (Kumar, Deshmukh, & Adhish, 2014). From a personal point of view, my sense of power is defined by high internal control. I believe in my actions in an attempt to achieve my aims. This notion and pursuit of power empower me to interact positively with my followers and ensure desired outcomes are recorded. This personal sense of power is characterized by openness to new experiences, conscientiousness, and self-esteem. I use this scheme to ensure every nurse delivers high-quality health services.
The motivation for Increasing My Power Base
One of my goals is to increase my power base to transform the experiences of my followers. Since I am intrinsically motivated, my internal locus guides me to remain conscientious and focus on concepts that can support my leadership objectives. This source of motivation guides me to develop dexterities that can support my objectives.
My patients’ needs encourage me to increase my power base. I always empower and address the changing health needs of underserved populations. This obligation guides me to increase my power base and influence the quality of health services. A leader with a positive sense of power applies evidence-based strategies to develop the best working environment (Kumar et al., 2014). I use this notion to strengthen my power base and create diverse teams that can meet the needs of more patients.
Plan for Enhancing My Power as a Nurse/Leader-Manager
Detailed Plan
Personal power and leadership abilities can be enhanced using evidence-based strategies. My plan for enhancing my power as a leader-manager and a nurse is characterized by five steps.
- Self-evaluation. The first step is to understand my style and level of power. This is realized using continuous self-assessment. This move can guide me to understand my capabilities as a nurse manager or leader.
- Analyzing the current situation. The second step is analyzing my situation. This stage will reveal the abilities that make me a successful charge nurse.
- Identifying gaps. The third step is identifying the gaps affecting my abilities. Issues that make me less effective are identified during this stage (Kumar et al., 2014). Analyses are conducted to identify every unsuccessful practice or approach.
- Development. The fourth step is to develop the required strengths, abilities, and dexterities. Training and can be considered during this stage. I will also identify a role model. These strategies are considered to enhance my power.
- Practice. The final stage is implementing the acquired dexterities. This is achieved through constant practicing in different clinical and leadership settings. The same plan will be adopted to increase my power as a charge nurse.
Strategies for Social Change, Empowering Others, and Personal Power Base
In order to achieve this plan, various strategies should be taken seriously (Kim, Kim, & Choi, 2016). For example, training will ensure new ideas and practices are acquired. Participating in different teams can maximize my power and eventually make it easier for me to promote social change. The idea of practice (5th step) can be considered to attract more nursing and empower them to promote social change. It is necessary to offer incentives and resources to others throughout the leadership process. These strategies can make it easier for leaders to empower others (Harris, 2016). Strategies such as lifelong learning, experimentation, and use of journal entries can be considered to build a personal power base successfully. Journal entries can be utilized to track new strengths and leadership ideas that can influence social change and empower others.
References
Harris, A. (2016). Nursing to achieve organizational performance: Consider the role of nursing intellectual capital. Healthcare Management Forum, 29(3), 1-13. Web.
Kim, M., Kim, E. J., & Choi, S. (2016). A study of the relationship between nursing performance, job satisfaction, and organizational commitment. Advanced Science and Technology Letters, 128, 94-97. Web.
Kumar, S., Deshmukh, V., & Adhish, V. S. (2014). Building and leading teams. Indian Journal of Community Medicine: Publication of Indian Association of Preventive & Social Medicine, 39(4), 208-213. Web.
Marquis, B. L., & Huston, C. J. (2015). Leadership roles and management functions in nursing: Theory and application (8th ed.). Philadelphia, PA: Lippincott, Williams & Wilkins.
Salmela, S., Eriksson, K., & Fagerström, L. (2013). Nurse leaders’ perceptions of an approaching organizational change. Qualitative Health Research, 23(5), 689-699. Web.
Shirey, M. R. (2013). Lewin’s theory of planned change as a strategic resource. The Journal of Nursing Administration, 43(2), 69-72. doi:10.1097/NNA.0b013e31827f20a9 American Association of Colleges of Nursing. (2014). Fact sheet: Creating a more highly qualified nursing workforce. Web.
Mindtools. (n.d.). Leadership skills: Become an exceptional leader. Web.