Evidence-based Clinical Guidelines: Discussion
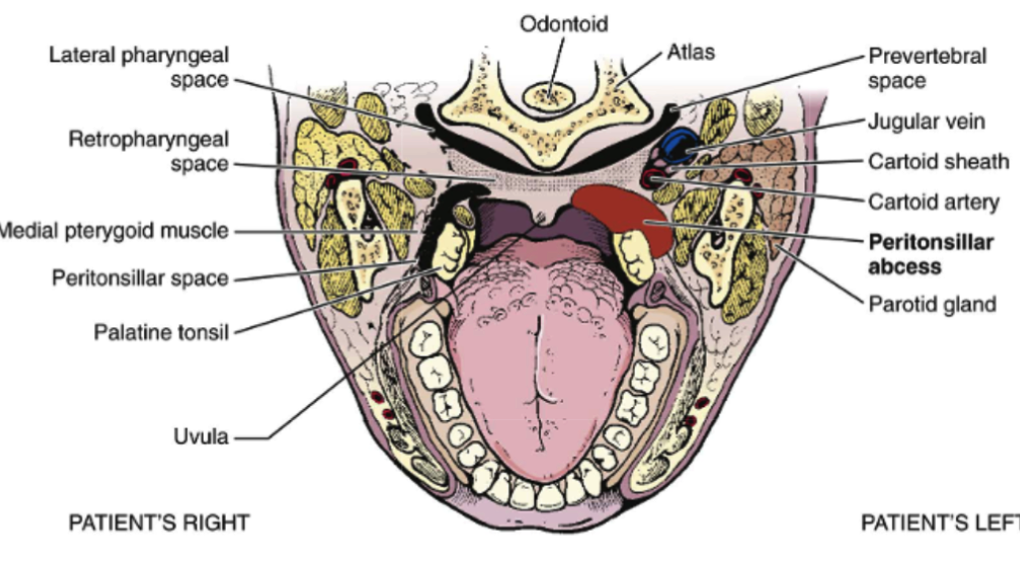
A deep head-and-neck polymicrobial infection is typically defined as a peritonsillar abscess (Afolabi et al., 2014) (see Fig. 1). As a rule, young adults are affected most by the disease (Gal, Hsu, Mallon, Mattioni, & Nagorsky, 2014). A peritonsillar abscess manifests itself in the following symptoms: a sore throat, fever, otalgia, and malaise (Afolabi et al., 2014). Seeing that there is no agreement about the approaches to managing PA, a nurse must consider a combined approach involving the needle aspiration followed by a possible drainage, with tonsillectomy used if other measures fail.
In order to address the subject matter, one should consider the resources located at National Institutes of Health (Stelter, 2014). As far as the clinical guidelines for peritonsillar abscess treatment are concerned, there are no uniform ones at present: “There is no clinical practice guideline existed, and PTA treatment varies widely among different countries” (Wang, Wang, Lin, & Chou, 2014, p. 6). As a result, the quality of the nursing services provided to the patients varies significantly based on the standards adopted in the facility (Papadakis, McPhee, & Rabow, 2014). Nevertheless, general guidelines that are common in every facility include introducing corticosteroids to the patient’s bloodstream intravenously, providing the patient with humidified oxygen, and inserting a nasal airway device into the patient’s nose (from the nostril to the earlobe) (Mandal, Kabra, & Lodha, 2015).
Advanced Practice Procedures: Plan of Care
Even though there are currently no uniform guidelines for addressing the issue of PA, there are several advanced nursing practice procedures that need to be performed on the patient. The identified practices include, but are not limited to, the following measures:
- Needle aspiration. A needle is inserted into the tissue to release the pus.
- Incision and the following drainage. The identified framework is typically viewed as more efficient than the needle aspiration process. The procedure involves releasing the pus by making an incision.
- Quinsy. Also known as the Quinsy tonsillectomy, the identified procedure implies removing the palatine tonsils in case the patient continues to experience discomfort after the drainage. The procedure is often deemed as controversial, yet it provides relief from the obstruction and allows avoiding an infection (Stern, Cifu, & Altkorn, 2015).
Advanced Technology for Monitoring and Control
To make sure that the patient’s needs are met fully and that the quality of the services meets the set standards, one will have to consider monitoring techniques and tools. For instance, the EarlySense System device should be viewed as possible assistance in managing the patients’ needs (Brown, Terrence, Vasquez, Bates, & Zimlichman, 2014).Taking oral temperatures should also be viewed as the necessary control tool.
Evidence-based Plan of Care: Steps
In order to facilitate the environment in which the patient will be relieved from pain, receive the necessary services, and recover successfully, a nurse will have to consider taking the following steps:
- Airway assessment with extensive support of ventilation and oxygenation;
- Active prevention of patient agitation by providing relaxing and soothing environment;
- Oropharynx examination;
- Introduction of the intravenous line;
- Hydration of the intravenous line;
- Administration of antibiotics (penicillin, clindamycin, etc.) (Gal et a., 2014);
- Pain control.
Controlling the levels of pain is crucial to build the atmosphere in which recovery will become a possibility. Furthermore, the speed and efficacy of the services delivery will improve the patient’s chances to recover. Additionally, the contraction of nosocomial infections should be prevented.
References
Afolabi, O. A., Abdullahi, A., Labaran, A. S., Ladan, S., Sanni, R., Muasa, E.,& Ahmad, B. M. (2014). Peritonsillar abscess in Northern Nigeria: A 7 years review. Malaysian Journal of Medical Sciences, 21(6), 14-18.
Gal, K., Hsu, K., Mallon, A., Mattioni, J., & Nagorsky, M. (2014). Peritonsillar abscess with internal carotid artery stenosis. Journal of Case Reports in Medicine, 3(235831), 1-3.
Mandal, A., Kabra, S. K., & Lodha, R. (2015). Upper airway obstruction in children. Indian Journal of Pediatrics, 82(8), 737-744.
Papadakis, M., McPhee, S. J., & Rabow, M. W. (2014). Current medical diagnosis and treatment: 2015 (54th ed.). New York, NY: McGrw-Hill.
Peritonsillar abscess drainage. (2014). Web.
Stelter, K. (2014). Tonsillitis and sore throat in children. GMS Current Topics in Otorhinolaryngology, 13, 1-24.
Stern, S. D. C., Cifu, A. S., & Altkorn, D. (2015). Symptom to diagnosis: An evidence-based guide (3rd ed.). New York, NY: McGraw-Hill Education.
Wang, Y. P., Wang, M. C., Lin, H. C., & Chou, P. (2014). The impact of prior tonsillitis and treatment modality on the recurrence of peritonsillar abscess: A nationwide cohort study. PLoS One, 9(10), 1-7.