Total knee replacement (TKR), also named total knee arthroplasty (TKA), is a common surgical procedure often performed for osteoarthritis patients or after trauma. People may suffer from severe pain during the postoperative period. Moreover, two trajectories of long-term outcomes are possible: good – people feel gradual improvement, and poor – about one-fifth of patients report subsequent chronic pain (Dumenci et al., 2020). In the second case, specialists can make a prognosis about health indicators deterioration and significant reduction of the patients’ quality of life (Siviero et al., 2020). Therefore, the issue of finding effective pain management methods after TKA is relevant for the research.
The number of cases using TKR is expected to increase worldwide and in Australia in particular. According to Ackerman et al.’s (2019) prognosis, the application of this operation is likely to increase by 276% by 2030. The cost of the procedure ranges from $ AUD19,000 to $ AUD30,000 per patient and, together with a similar operation, hip replacement, the burden on healthcare will be $ AUD5.32 billion in 2030 (Ackerman et al., 2019). The authors also note an expected increase in surgeries worldwide, including a younger population, although TKA was previously more applied to the older generation.
Experts are using various measures to help patients after TKR. The most common method is opioids, but their adverse effects raise concerns. Subsequently, the researchers consider multimedia analgesia the optimal option for drug-induced pain management (Li et al., 2019). Psychological interventions are rarely used, and their effectiveness is doubtful (Whale et al., 2019). However, psychological factors are influential in the development of chronic pain. Cognitive Behavior Therapy (CBT) aims to control such factors, which justified the study of the question: “In adult patients who have undergone trauma-induced TKA, is a CBT program effective to prevent the potential development of chronic pain?”
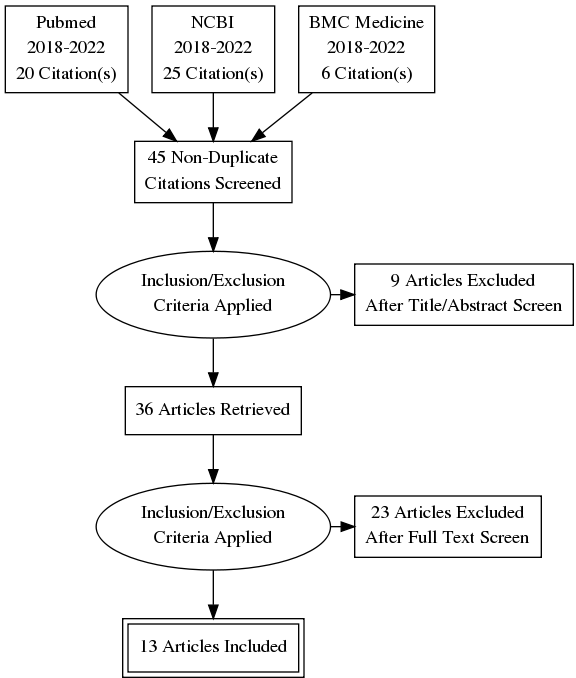
PRISMA Diagram
Review of the Literature
Pain Predictors and Chronification
As noted, chronic post-surgical pain (CPSP) is a consequence of TKA for a fifth of patients. Several predictors may suggest the likelihood of developing pain in people who need surgery. Kim et al. (2018) distinguish unlikely and potentially modifiable CPSP risk factors for TKR patients. The comorbidities, age, sex, and socioeconomic situation of the person do not change and help determine the risks. The psychological state is a modifiable factor and includes anxiety and catastrophizing pain. The latter term refers to situations where people tend to exaggerate their pain, its threat and, as a result, increase their negative attitude towards experience. It is worth noting that catastrophizing pain is an influential factor in developing chronic pain, and many studies discussed below take its effect into account. According to Kim et al.’s (2018) opinion, behavioral therapy can help manage the psychological condition. However, this source does not consider CBT broadly, limiting its use for current research.
Various studies of the psychological factors’ impact on pain management have contradictory results. The cohort study by Abrecht et al. (2019) does not provide evidence of significant psychological factors’ influence when evaluating postoperative pain predictors. Furthermore, the researchers highlight body mass index (BMI) and preoperative pain as critical determinants for pain. Although their study includes psychological factors, the authors find their impact insignificant. Terradas-Monllor et al. (2020), in turn, found that patients with high catastrophizing rates have worse health outcomes and severer resting pain. Thus, despite some underestimation of psychological factors, the research of their influence, especially pain catastrophizing, is relevant for exploring the implications of TKR.
One can distinguish several factors contributing to the chronification of pain in various circumstances. Pak et al. (2018) believe that chronic pain develops due to peripheral and central sensitization. They also note risk factors and divide them by groups – related to surgery, opioid use, and patients. The latter include personality disorders, anxiety, and mood disorders and contribute to chronic pain. Meints and Edwards (2018) also investigate the role of psychology in the development of chronic pain. They highlight distress, personal relationships, trauma attitudes, catastrophizing, patient expectations, and self-efficacy as significant risk factors for chronic pain. Thus, despite doubts, it is worth continuing to study the psychological component of pain and the development of interventions on its basis.
Cognitive Behavioral Therapy
Psychological interventions are hardly used in orthopedics, including the considered surgery TKR. A review of randomized controlled trials conducted by Bay et al. (2018) demonstrates that the use of psychological interventions is not yet supported in academia. However, the authors also note that literature on similar interventions in cases of TKA is just beginning to develop. They highlighted several methods that are most discussed and have some evidence of efficacy. Such measures include CBT, relaxation therapy, psychoeducation, and guided imagery (Bay et al., 2018). CBT attracts the attention of many researchers, and some studies of its application in TKA cases are already present.
Researchers focused on the issue of pain chronification, and its psychological predictors mention CBT as an effective method to avoid such an outcome. For example, Park et al. (2018) note that therapy can prevent chronic pain, as it helps cope with anxiety and relax. Moreover, CBT aims to establish patients’ control over stress, reducing pain intensity and the tendency to take opioids. Meints and Edwards (2018) also pay attention to CBT as it “involves reframing negative automatic conventions, such as catastrophic conventions” (p. 181). They believe that as a result, a decrease in catastrophizing will last a long time – months or even years. Consequently, there are solid theoretical assumptions about the positive effect of CBT on pain management.
Several studies prove the association of better psychological health with post-TKA outcomes. Nwankwo et al.’s (2021) cohort study examines patients’ resilience and its impact. The authors also note the influential role of catastrophizing pain in developing chronic pain. The study results demonstrate that patients with higher resilience have better outcomes after surgery. Since CBT helps patients cope with stress, therapy can increase resilience and improve the condition after TKR. However, the study of Nwankwo et al. (2021) has a limitation, emphasizing the preoperative person’s psychological health. Patients who require urgent surgery after an injury cannot be prepared for the consequences, particularly acute pain.
Pain after surgery may not only become chronic but also contribute to kinesiophobia – fear of movement and physical activity. Cai et al. (2018) conducted a randomized controlled trial, which demonstrated that CBT helps reduce pain and kinesiophobia intensity. The limitation is that the phobia itself could contribute to pain, and CBT affected it. However, given that psychological factors are important to consider in pain management, their findings are helpful for the research question.
The use of therapy is possible in combination with other methods, increasing the effectiveness of the intervention. Rognsvåg et al. (2021) proposed developing an internet-delivered CBT program to prevent chronic pain. This program combines CBT, exercise, and patients’ education, and the authors expect it to be a valuable contribution to the issue of TKA consequences. However, since their approach involves combining CBT with different procedures, it may distort the results for the current research question. In turn, Sun et al.’s (2020) study does not include other methods and compares the group involved in CBT and the group of usual care. Their results showed that therapy decreased pain during patients’ physical activity and catastrophizing, but resting pain remained at the same level. Thus, the majority of studies proving CBT efficacy still have significant limitations.
Some studies do not find substantive evidence of the CBT influence. For example, Chen et al. (2021) conducted a trial to explore the effect of therapy on the older generation – patients over 70 years who underwent TKR. CBT had no effect in reducing pain in the study group, and the difference with the control group was only noticeable in the level of anxiety. Patients’ age is a limitation of the study for the current research, but it still presents valuable results. Another trial conducted by Birch et al. (2020) found no significant effect of CBT. Study participants had moderate and high levels of catastrophizing pain before surgery, and therapy did not decrease their pain after TKR. Evaluation before surgery limits outcomes and understanding of the role of CBT in postoperative recovery for the presented research question. These studies emphasize the inconsistency of the information available to date on the effects of therapy.
The presence of conflicting evidence complicates the issue of CPSP prevention. A meta-analysis by Wang et al. (2018) provides valuable data on the efficacy of therapy in controlling persistent pain after surgery extracted from comparisons of randomized controlled trials. The authors divided the evidence found by quality – moderate and high. Studies corresponding to the first group demonstrate that CBT, relaxation therapy, and their combinations reduce persistent pain. Sources of higher quality, in turn, do not prove the positive effect of psychological support or patient psychoeducation on their pain (Wang et al., 2018). Thus, the existing literature has gaps in the study of CBT effects after TCR.
Some patterns and relative consensus are noticeable in the reviewed literature. Remarkably, many authors agree on the influence of psychological factors and especially of catastrophizing pain. However, gaps and inconsistencies are more evident – results and conclusions differ. For example, few studies have explored the CBT effect solely without other methods, and their findings are inconsistent (Birch et al., 2020; Cai et al., 2018; Chen et al., 2021; Sun et al., 2020). Some studies support the effectiveness of CBT in pain management, and some find no evidence for it. Furthermore, all studies consider patients who require TKR after osteoarthritis rather than trauma. As a result, their interventions often begin during the preoperative time, highlighting the influence of the patients’ conditions before TKR. Consequently, there are gaps in the research that need to be filled.
Translation to Practice
The study has implications for nursing work, as the theoretical basis for using CBT in pain management after TCR is compelling enough to suggest its effectiveness in practice. Nevertheless, more empirical research is needed in new areas to investigate the question posed. First, there is a need to understand differences in condition and pain level between TCA outcomes for osteoarthritis patients and after trauma. Existing research is significantly focused on the first group, hindering the effectiveness of interventions developed for the second.
Another direction for further study is the factors that affect the effectiveness of CBT in preventing chronic pain. Since the sources reviewed provide conflicting results, one can assume that CBT may be valuable for certain patients and not suitable for others. The effect of therapy can be influenced by the age of patients, personal traits, attitude towards such a treatment, the presence of specific disorders, and similar aspects. Thus, the current paper suggests the potential of CBT in preventing chronic pain for the patient in the case and indicates the need for new research in the orthopedic field.
References
Abrecht, C. R., Cornelius, M., Wu, A., Jamison, R. N., Janfaza, D., Urman, R. D., Campbell, C., Smith, M., Haythornthwaite, J., Edwards, R. R., & Schreiber, K. L. (2019). Prediction of pain and opioid utilization in the perioperative period in patients undergoing primary knee arthroplasty: Psychophysical and psychosocial factors. Pain Medicine (Malden, Mass.), 20(1), 161–171.
Ackerman, I. N., Bohensky, M. A., Zomer, E., Tacey, M., Gorelik, A., Brand, C. A., & de Steiger, R. (2019). The projected burden of primary total knee and hip replacement for osteoarthritis in Australia to the year 2030. BMC Musculoskeletal Disorders, 20(1), 1-10.
Bay, S., Kuster, L., McLean, N., Byrnes, M., & Kuster, M. S. (2018). A systematic review of psychological interventions in total hip and knee arthroplasty. BMC Musculoskeletal Disorders, 19(1), 1-11.
Birch, S., Stilling, M., Mechlenburg, I., & Hansen, T. B. (2020). No effect of cognitive behavioral patient education for patients with pain catastrophizing before total knee arthroplasty: A randomized controlled trial. Acta Orthopaedica, 91(1), 98–103.
Cai, L., Gao, H., Xu, H., Wang, Y., Lyu, P., & Liu, Y. (2018). Does a program based on cognitive behavioral therapy affect kinesiophobia in patients following total knee arthroplasty? A randomized, controlled trial with a 6-month follow-up. The Journal of Arthroplasty, 33(3), 704–710.
Chen, W., Sun, J. N., Hu, Z. H., Zhang, Y., Chen, X. Y., & Feng, S. (2021). Cognitive behavioral therapy cannot relieve postoperative pain and improve joint function after total knee arthroplasty in patients aged 70 years and older. Aging Clinical and Experimental Research, 33(12), 3293–3302.
Dumenci, L., Perera, R. A., Keefe, F. J., Ang, D. C., Slover, J., Jensen, M. P., & Riddle, D. L. (2019). Model-based pain and function outcome trajectory types for patients undergoing knee arthroplasty: A secondary analysis from a randomized clinical trial. Osteoarthritis and Cartilage, 27(6), 878–884.
Kim, D. H., Pearson-Chauhan, K. M., McCarthy, R. J., & Buvanendran, A. (2018). Predictive factors for developing chronic pain after total knee arthroplasty. The Journal of Arthroplasty, 33(11), 3372-3378.
Li, J. W., Ma, Y. S., & Xiao, L. K. (2019). Postoperative pain management in total knee arthroplasty. Orthopaedic Surgery, 11(5), 755-761.
Meints, S. M., & Edwards, R. R. (2018). Evaluating psychosocial contributions to chronic pain outcomes. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 87(Pt B), 168–182.
Nwankwo, V. C., Jiranek, W. A., Green, C. L., Allen, K. D., George, S. Z., & Bettger, J. P. (2021). Resilience and pain catastrophizing among patients with total knee arthroplasty: A cohort study to examine psychological constructs as predictors of post-operative outcomes. Health and Quality of Life Outcomes, 19(1), 1-11.
Pak, D. J., Yong, R. J., Kaye, A. D., & Urman, R. D. (2018). Chronification of pain: Mechanisms, current understanding, and clinical implications. Current Pain and Headache Reports, 22(2), 1-6.
Rognsvåg, T., Lindberg, M. F., Lerdal, A., Stubberud, J., Furnes, O., Holm, I., Indrekvam, K., Lau, B., Rudsengen, D., Skou, S.T., & Badawy, M. (2021). Development of an internet-delivered cognitive behavioral therapy program for use in combination with exercise therapy and education by patients at increased risk of chronic pain following total knee arthroplasty. BMC Health Services Research, 21(1), 1-14.
Siviero, P., Marseglia, A., Biz, C., Rovini, A., Ruggieri, P., Nardacchione, R., & Maggi, S. (2020). Quality of life outcomes in patients undergoing knee replacement surgery: Longitudinal findings from the QPro-Gin study. BMC Musculoskeletal Disorders, 21(1), 1-11.
Sun, J. N., Chen, W., Zhang, Y., Zhang, Y., Feng, S., & Chen, X. Y. (2020). Does cognitive behavioral education reduce pain and improve joint function in patients after total knee arthroplasty? A randomized controlled trial. International Orthopaedics, 44(10), 2027–2035.
Terradas-Monllor, M., Ochandorena-Acha, M., Salinas-Chesa, J., Ramírez, S., & Beltran-Alacreu, H. (2020). Assessment of postoperative health functioning after knee arthroplasty in relation to pain catastrophizing: A 6-month follow-up cohort study. PeerJ, 8, 1-22.
Wang, L., Chang, Y., Kennedy, S. A., Hong, P. J., Chow, N., Couban, R. J., McCabe, R. E., Bieling, P. J., & Busse, J. W. (2018). Perioperative psychotherapy for persistent post-surgical pain and physical impairment: A meta-analysis of randomised trials. British Journal of Anaesthesia, 120(6), 1304-1314.
Whale, K., Wylde, V., Beswick, A., Rathbone, J., Vedhara, K., & Gooberman-Hill, R. (2019). Effectiveness and reporting standards of psychological interventions for improving short-term and long-term pain outcomes after total knee replacement: A systematic review. BMJ Open, 9(12), 1-14.