- Abstract
- Introduction
- Mechanism of Action of Nsaids
- The Cyclooxygenase Pathway
- The Isoforms of COX
- The Therapeutic Effects of Nsaids
- The Negative Effects of Blocking of the Cyclooxygenase Pathway
- The Clinical Side Effects Seen Due to Nsaid Use
- What Effects Have Resulted From the Isoforms of Nsaids
- Conclusions
- References
Abstract
The use of NSAIDS has been in general medical practice for many years and its therapeutic effects documented for a long time. NSAIDs have been widely known for their analgesic, antipyretic and anti-inflammatory activities. They have been used in many clinical situations with good outcomes. The local, as well as central analgesic and antipyretic effects, have made them very popular in use both in and outside of surgical procedures. The anti-inflammatory properties have made them the drugs of choice for patients with rheumatoid arthritis. However, there are still areas that increase concern about the use of these drugs in patients. Recent studies as well as the removal of certain NSAIDs from the market rose concerns about the adverse effects of NSAIDs in the risk of cardiovascular conditions and in the promotion of renal failure and gastric complications. There is increased emphasis on using NSAIDs with caution and with much deliberation the benefits will outweigh the risks.
Introduction
NSAIDS have become one of the most prescribed analgesic drugs due to its rapid effect and other properties. NSAIDs or non-steroidal anti-inflammatory drugs are mainly used as agents to reduce patient’s fever, pain and inflammation in an area. (Ogbru, 2007, para 1) These drugs are very commonly used with regional anesthesia to relieve pain after surgeries, and are also used in combination with substances like opioids and paracetamol to achieve a balanced analgesia. NSAIDS have been used in almost all age groups, although side effects may make certain candidates not suitable for the medicine. All in all, NSAIDS have shown very good clinical results in offering relief from moderate to severe pain.
NSAIDS in combination with opioids helps in reducing the dependency effect that may develop and therefore helps the patient adapt more quickly to the reducing dose of opioids. Other indications also include chronic pain and palliative care patients. (Ogbru, 2007, Para 3)
Among the many other uses of NSAIDS include headaches, arthritis, sports injuries, and menstrual problems. Due to its property to reduce blood coagulation, NSAIDS are now widely used as preventive method to reduce stroke incidences in susceptible patients. (Ogbru, 2007,Para 2)
Arthritis is one particular area where the use salicylate derivatives and NSAIDS have been extremely beneficial. This is due to the ability of the NSAIDS to block the prostaglandin activity of the enzyme which is the primary mediators of inflammation. By further understanding the selective use of COX 2 inhibitors the physicians were able to provide a good anti-inflammatory agent to the arthritis patients with low gastric mucosa ulceration or irritation responses. (Vane and Botting, 2003, pp. 255, 256)
Mechanism of Action of Nsaids
The mechanism of action of the NSAIDS cannot be understood with out looking at the system that it works on. NSAIDS work by inhibiting the activity of the prostaglandins, which are the primary inflammatory mediators of the body. These prostaglandins are derived from arachidonic acid. The arachidonate is bis-oxygenated to form prostaglandin or PGG2. The PGG2 is then reduced to PGH2 via a peroxidase reaction. Both the steps of the formation of prostaglandin are mediated by the enzyme cyclooxygenase also known as the PGH synthase. (Myceck et al, 2002, pp. 402)
Structurally, arachidonic acid is a 20-carbon fatty acid, present as a component of the phospholipids of the cell membranes. It is particularly found in phosphatidyl inositol and other complex lipids. When phospholipase A2 and other acyl hydrolases act on the phospholipids, it causes the release of arachidonic acid. (Myceck et al,2000, pp 402)
Arachidonic acid now can follow two fates. Both however, lead to the formation of the eicosanoids. The lipoocygenase pathway comprises of lipooxygenases enzymes that act on arachidonic acid and result in the formation of 5-HPETE and 15-HPETE respectively. These are unstable forms that are immediately converted to HETES, lipoxins or leukotrienes. This conversion takes place depending on the type of tissue where the activity is taking place.
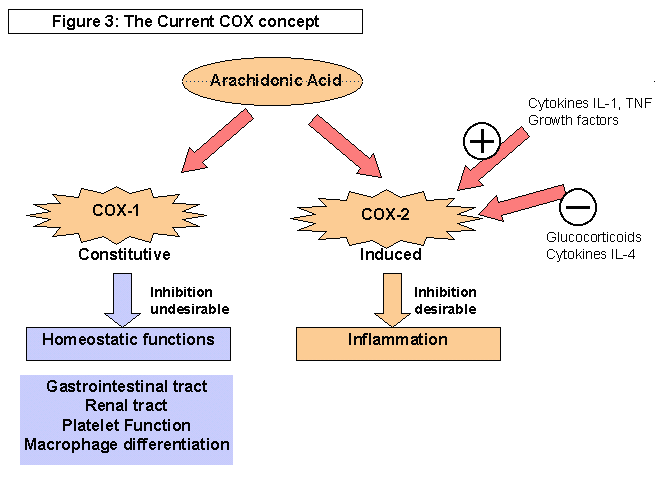
The cyclooxygenase pathway is a specific pathway that leads to the formation of ringed structures such as prostaglandins, thromboxanes and prostacyclins. Cyclooxygenase pathway consists of two enzymes, the COX-1 and the COX-2 enzymes respectively. Activity of these both enzymes differs and is of significance in pharmacology. While COX-1 functions as a protective and constructive mechanism of the body, it is the COX-2 that leads to the creation of inflammatory responses. (Myceck et al, 2000, pp 402)
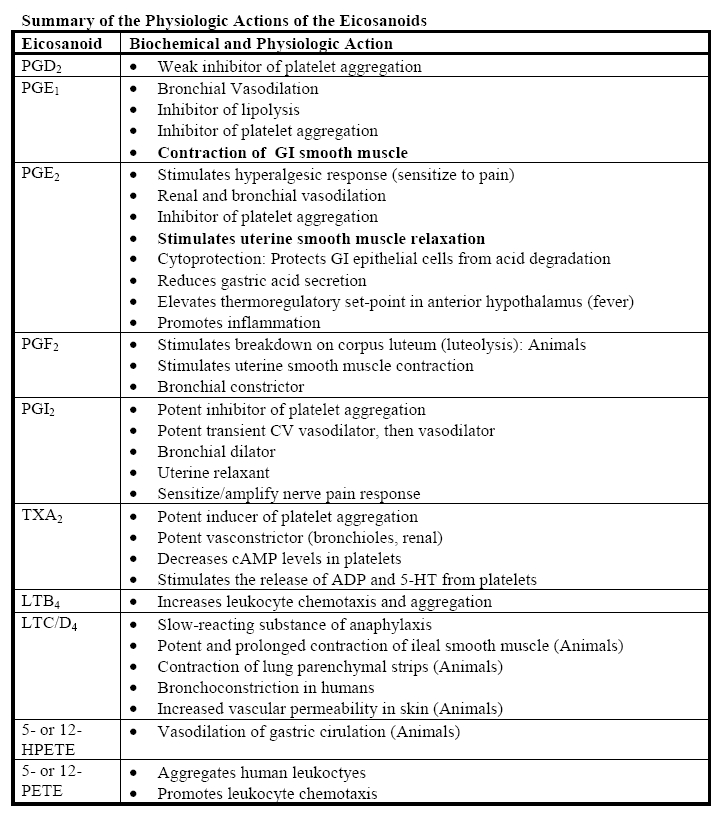
The prostaglandins thus created perform many functions. However, these actions are mediated by their ability to bind to multiple kinds of receptors which operate through the G protein pathway. These G proteins have the ability to either activate or inhibit adenylyl cyclase or stimulate phospholipase C. The result is the formation of diacyglycerol and inositol.-1,4,5 triphosphate (IP3). This formation then can lead to a myriad of functions depending upon the type of tissue in question. (Myceck et al, 2000, pp 402)
By inhibiting the activity of the prostaglandins, which mediate inflammatory responses, the NSAIDS are able to achieve their analgesic, anti-inflammatory and antipyretic responses. The analgesic action of the NSAIDS is not only dependant on the inhibition of the cyclooxygenase pathway, but also through other peripheral and central methods. COX2 activity inhibition is among the first methods of causing analgesia, along side inhibition of lipooxygenase pathway in some drugs. Another method is the interference with signal transduction caused by the G-protein. The inhibition of the prostaglandin formation within the CNS is another cause of reduced peripheral formation of prostaglandins and thereby decreasing inflammatory responses. The blockage of release of serotonin and the endogenous opioids peptides are also proposed mechanisms for the analgesic properties of NSAIDS. (Cashman, 1996, pp 14, 17, 19)
It is here that the role of another important related moiety, the endoperoxides be discussed. Prostaglandin endoperoxides are “precursors in the biosynthesis of prostaglandins and thromboxanes from arachidonic acid. They are physiologically active compounds, having effect on vascular and airway smooth muscles, platelet aggregation etc.” (Cancer web, NP, 2007)
The Cyclooxygenase Pathway
As mentioned above the release of the arachidonic acid is the prime initiator for the cyclooxygenase pathway. This arachidonic acid is present in the cell membranes of the tissues that are released if any damage is sustained to it. Enzyme that is responsible for its release is the phospholipase A2. Many phospholipase exist which act in different methods to help in the release of the arachidonic acid. (Sarkar, 2005, para 4)
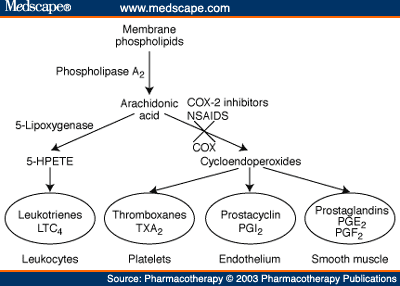
The arachidonic acid, if metabolized by the cyclooxygenase pathway, causes the production of two things. These are known as the Prostaglandin H2 or PGH2 and Prostaglandin B2 orPGB2, these being the precursors of prostaglandins Prostaglandin E 2 (PGE2), Prostaglandin F2 (PGF2), Prostaglandin I2 (PGI2) and thromboxanes. (Sarkar, 2005, Para 8)
Prostaglandins are also known as the paracrine secretions or the secretions of the local hormones. Most of the actions of these prostaglandins are localized and are only effective locally. The production of these entities stimulates the nociceptors thereby causing pain in the area. They also enhance the effects of certain chemical mediators, such as histamine and bradykinin, which is a feature in asthma. Since these prostaglandins cause vasodilatation and increase blood flow, neutrophils migration, phagocytosis, they initiate the inflammatory response in the region. (Sarkar, 2005, Para 7 and Allain, 2007, NP)
In summary, therefore, the production of the prostaglandins and the metabolites of the arachidonic acids produce inflammatory reactions, which although are a protective mechanism of the body, may become problematic in certain cases. The blockage of the cyclooxygenase system therefore reduces or even inhibits the inflammatory response o the body, an effect that is seen in the use NSAIDS. (Allain, 2007, NP)
The inhibition of this pathway therefore results in multiple effects that are either beneficial or harmful. These can be clearly stated as the therapeutic effects of NSAIDS and the non therapeutic effects of the NSAIDS.
The Isoforms of COX
COX was for the first time isolated in the year1976. Prior to this the efficacy of salicylates and salicylate like agents or NSAIDS was well established. It was initially found in the prostanoid cells in large quantities. It was later on that the presence of COX was found in many other cells and locations as well. (Vane and Botting, 1998, pp 4)
The recent researches have confirmed the presence of variable isoforms of COX. The three types are known as COX I, II or III respectively. Each has its unique typology, location and mechanism of activation and action. Type I COX is constitutive in nature, and is present in the stomach, kidneys and the thrombocytes. Type II is formed after the induction in various tissues of the body such as fibroblasts, macrophages, chondrocytes and the uterus. Mostly COX II is inductive in nature but in tissues such as the brain, kidney and the stomach, these can be constitutive. The type III is constitutive found only in brain. (Vane and Botting, 1998, pp 5)
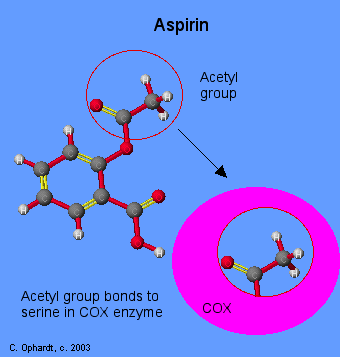
COX-1 consists of a three dimensional structure, consisting of three independent foldings. These are an epidermal growth factor like domain, a membrane binding motif and an enzymatic domain. Each fold is particular in its activity. Peroxidase and COX sites of activity are distinct from each other. The membrane binding motif is able to integrate to one leaflet of the cell membrane and is therefore termed as the monotopic membrane protein. The structure of the molecule therefore consists of three helices which are configured to form an entrance to the COX channel. This configuration allows the arachidonic acid to gain access to the site. By excluding this arachidonate from the upper portion of the channel, the NSAIDS are able to inhibit the activity of the COX-1. Other drugs also work in their respective manner to exclude access and binding of the arachidonic acid. (Vane and Botting, 1998, pp10)
These three cyclooxygenases have the same molecular weights and structure. However, the main difference is in the site of attachments of these forms. For example, the attachment site of COX 1 is smaller; therefore its interactions are limited to very few substrates. The COX 2 however, is attached to a larger site, has more reactivity than its sister molecule and therefore is able to carry out more potent actions on the sites. The main functions however, are the same. The receptor sites of the arachidonic acid on the cyclooxygenase enzyme are blocked, which prevents the mediation of the inflammatory response of the enzyme. The chemical action that is carried out here is acetylation, which is very effective for small site area of COX 1, but not so effective for COX2 inhibitors. The effects achieved are both anti-inflammatory and anti platelet, which is why the NSAIDS have become an ideal drug for the prevention of propagation of clots myocardial infarction patients. (Sarkar, 2005, Para 3)
COX 1 is present constitutionally in many tissues of the body, and produces arachidonic metabolites during homeostatic function. This isoforms is responsible to maintaining the physiological functioning of a variety of organ. This is specifically present in the gastric mucosa and the platelets. This COX 1 is important in maintaining the integrity of the gastric mucosa. In the platelets, it is responsible to produce thromboxanes A2, which helps in the aggregation of the platelets. This however, does not mean that COX 1 cannot mediate and pathological response, it only impresses that COX1 is primarily responsible for the promotion of the homeostatic function of the body. This clearly demonstrates why the COX 1 inhibitors cause increased gastric ulceration and mucosal damage to the stomach. COX 1 is also are seen to help prepare the myometrial wall in the mother for the implantation of the embryo. (Lipsky et al, 2000, pp. 915, 917 and 918)
A major difference in the identification and working of the COX 1 and 2 inhibitors is the utilization of the arachidonic acid. The COX1 uses the arachidonic acid that is derived extracellularly, while the COX2 utilizes intracellular arachidonic sources. Most of the COX 1 and COX 2 enzymes produced from different surfaces have the same structural configuration to each other, meaning that COX 1 produced from one site can also affect other sites as well. Same is true for COX 2 enzymes. COX 1 effects are immediate and timely in nature due to their smaller size and their ability to easily bind to their receptors. The COX2 enzymes however, require more time for their confirmation to the receptor and have a more prolonged effect once they get bound to the site. (Lipsky et al, 2000, pp. 915) COX-2 is induced by inflammatory stimuli and cytokins in migratory and other cells, however there function must not be limited only to inflammatory actions of the body. (Vane and Botting, 1998, pp12)
COX 2 enzymes are to some degree expressive in the normal functions of the body and therefore are not so readily available in the normal tissues due to their decreased activity. But in tissues such as the macrophages and tissues associated with inflammatory reactions, the response is created immediately. The release of prostaglandins increases this activity manifold. The researches now have clarified that COX 2 is essentially an inducible enzyme that is activated with the proinflammatory mediators. It also has shown that it is the COX 2 that is responsible for inflammation, edema, and pain in the tissues. Therefore any drugs that inhibit the action of COX2 automatically inhibit the inflammatory reactions from taking place. (Vane and Botting, 1998, pp 7)
The activity of the COX-2 selective inhibitors however, is not as potent as the glucocorticoids, as COX-2 are involved in blocking only one of the mediators of inflammation. (Vane and Botting, 1998, 10)
The role of these two enzymes is to some extent overlapping. Both of these enzymes can work either in homeostasis or in inflammatory reactions, although the strength of activity varies. COX 2 for example has shown activity in the development and maintaining of certain kidney functions. The production of prostaglandin by the COX 2 is responsible for the reuptake of sodium in the kidneys in cases of renal failure. The COX 2 production in the stomach cells is responsible for protecting the stomach from external attacks of microorganisms in the body. It also causes the presentation of fever by its activity in the central nervous system, neural adaptation and development and in local inflammation in the brain. In the uterus, the actual implantation of the embryo is made possible by the activity of COX2. (Lipsky et al, 2000, pp 914, 915, 916 and 917)
The Therapeutic Effects of Nsaids
The three primary uses of NSAIDS are antipyretic, anti-inflammatory analgesic effects. The antipyretic activity of NSAIDS is the direct result of its ability to block prostaglandin synthesis. At the initial stages of the NSAIDS development, the understanding of its full properties was inhibited by the missing knowledge about the two different kinds of cyclooxygenase inhibitors. Similarly, the effect of multiple substances on a tissue and the initiation of the protective, defensive and inflammatory reactions were not known. The understanding of the two types of COX was able to clarify the functions of each type and thereby the effects that they exerted on the tissues. NSAIDS have been shown to suppress and reverse the fever responses of the body. (Simmons et al, 2000, S 213)
The analgesic action of the NSAIDS is termed possible again to the prostaglandin inhibition. However, researches now support the multiple peripheral as well as systemic responses of the drugs on the tissues of the body. It is now established that the degree of inhibition of the COX2 inhibitors determines the level of analgesia that will be achieved. The adverse effects of the same drug however, can be determined by comparing the inhibition ratio of COX1 as well as COX 2. The central mechanism of action of these drugs also aid in reducing peripheral inflammatory response. (Cashman, 1996, pp 16) This concept of ratio between COX 1 and COX2 is significant because it helps in assessing “the balance of inhibition of the inducible COX-2. These ratios are present in varying quantities in different drugs. For example meloxicam has the ration of 0.33, diclofenic 2.2 and piroxicam 33. (Gotlieb, 2005, NP)
This central analgesic activity was proved recently by current researches. NSAIDS are seen to reduce the sensitivity of the central nervous system along with their local effects. The inhibition of the activity of the COX-2 enzyme is said to be responsible for this effect. (National Institute of Neurological Disorders and Stroke, 2001, NP)
The anti-inflammatory action of NSAIDS has been used to full benefit in cases such as post surgical care. It is however, seen to be most beneficial for cases which suffer from arthritis or other painful inflammatory conditions. Since these drugs are able to block the production of prostaglandins, the inflammation does not occur. Prostaglandins are responsible for the release of inflammatory mediators. (Vane and Botting, 2003, pp.258) PGE2 and prostacyclin are inflammatory products of the cyclooxygenase pathway. These are both potent vasodilators and hyperalgesic agents, found at the sites of injury. Their role is thought to be contributory in edema formation, erythema and in pain. They are also thought to decrease the neutrophil function and interfere with the activity of the phospholipase C enzyme. This is the main reason why NSAIDS have been recommended as the first line of treatment in acute low back pain in patients after injury. Both the analgesic and anti-inflammatory activity of the drug is able to provide immediate and sustained pain relief with a more swift recovery. (Malanga, 2007,NP)
The actions of NSAIDS are also seen to reduce the production of IgM rheumatoid factor in patients who suffer from rheumatoid arthritis. The NSAIDS “effectively remove suppressor T cells from the tonic inhibitory action of the PGE2”, which may be the reason for its unusual activity in such cases. (Goodwin et al, 2005, pp. S 50)
Recent studies have shown some very beneficial effects of NSAIDS in the treatment of conditions that were not thought of before. For example, Alzheimer’s disease, a neurodegenerative disorder, has shown signs of improving the signs of the condition as well slowing down the process. The mechanism of action is explained to be due to decreased deposition of amyloid beta in the tissues, which is a main reason for the pathogenesis of the condition. This has raised new questions about the potential role of NSAIDS in the treatment of Alzheimer’s disease. (Townsend and Pratico, 2005, pp 1593 and 1594)
Similarly, a separate study carried out Shaik et al in 2004 showed the inhibitory activity of nimesulide on the lung tumor especially A549 tumors. The inhibition was seen to be as high as 77.7%. This effect was seen without in any way affecting the COX 2 expression. This is yet another example of the therapeutic effects of NSAIDS in the treatment of multiple conditions. (Shaik, Chatterjee and Singh, 2004, pp 1526)
Another area of intense research is the role of NSAIDS in reducing the risk of colon cancer. Recurrent colon adenomas have been found to especially benefit from the NSAID therapies. This is especially the case with the chronic use of aspirin, although other NSAIDS are also thought to have a similar kind of role. These doses however are much higher for preventive purposes than the doses that are given to prevent heart complications. An apparent dose response relationship has been seen. While comparing non users, the multivariate RRs were 1.10 for women who used 0.5 to 1.5 standard aspirin tablets per week. It was 0.89 for two to five aspirin per week, 0.78 for 6 to 14 aspirins per week, and 0.68 for women using more than 14 aspirins per week. (Barclay, 2006, NP, para 5)A successful outcome requires that the drug be used early, with prolonged and consistent use. (Barclay, 2006, NP)
The Negative Effects of Blocking of the Cyclooxygenase Pathway
The blockage of the cyclooxygenase pathway although has certain therapeutic advantages, nevertheless, the blocking of any nature’s natural mechanism of the body leads to negative effects as well. Since inflammation is a manner of the body to react to any insult that it has sustained, suppression of this response can lead to negative outcomes. One of the common problems seen with the continuous use of aspirin or any other NSAID is the high rates of gastric erosion. This can cause gastric ulcer formation, and which can later on lead to the hemorrhage, a serious complication with high chances of mortality. (Derle, Gujar and Sagar, 2006, pp 410) Gastric hyperemia can be seen with in one to four hours of ingestion of two aspirins. These can result in erosions if the frequency is increased to four times in 24 hours. Gastric erosions and ulcers develop especially in those patients, whose bodies fail to adapt to the dosages of NSAIDS. Erosions can take place is approximately 30 percent of the patients. However, these are usually asymptomatic in nature. (Clearfield, 1992, para 3)
The Clinical Side Effects Seen Due to Nsaid Use
There are many reported clinical side effects of the NSAIDS and their use therefore should be carried out with caution. The biggest side effect is the effect on the gastrointestinal mucosa. These include both the COX 1 as well as COX 2 inhibitors. The drugs inhibit the COX 1 in the gastrointestinal tract, the main reason for the development of ulcers. The risk of gastrointestinal ulcer is increased significantly and can lead to life threatening complications like gastrointestinal hemorrhage, perforation and obstruction. Other complications related to gastric mucosa include occult bleeding with anemia, gastritis and epigastric pain, dyspepsia, duodenal ulcers which can hemorrhage and perforate and ulcerative esophagitis. (Derle, 2006, pp 411)
This fact has also been proved by the experiment of Vane and his colleagues in 1999, where they carried out two assay systems to identify the roles of COX1 and COX II in the causation of gastric damage. The assay carried out was William Harvey Modified Assay, and various NSAIDS were used for their role on the gastric mucosa working. The study was able to prove that the inhibition of the COX II inhibitor is the primary reason for the development of gastrointestinal problems among patients. (Vane et al, 1999, pp 7563)
About 15-30% of the patients who take NSAIDS regularly can develop gastrointestinal ulcers. The economical implications of this problem are also very large. For reduction in the use of NSAIDS and use of selective COX2 inhibitors have shown better results in the prevention of GI symptoms and have helped reduce the numbers of annual patients who come in for ulcer complaints. The ulceration potential however, is variable for variable drugs. Ibuprofen is thought to be least irritant to the gastric mucosa, followed by diclofenic and naproxen, and piroxicam and ketorolac pose the greatest risk of causing GI symptoms. However, the effect of dosage and its frequency is also a very significant element in the irritation potential of a drug. Many physicians recommend the use of acetaminophen as the better alternative to other NSAIDS due to its least irritation potential. Alongside, physicians recommend the use of anti ulcer therapies which may include proton pump inhibitors, prostaglandins, histamine H2 blockers and antacids. (Ong et al, 2007, pp 25)
NSAIDS have also been found to increase the risk of coronary diseases. The trial in discussion was carried out Rofecoxib which was seen to increase the risk of serious coronary heart disease by nearly twofold. Other drugs found to be of danger included naproxen which was found to have no cardio protective effect. Many drugs in the recent years have been taken back particularly due to this negative effect and this includes many COX 2 inhibitors. (CERTs Research, 2003, para 9)
The gastric effects are more likely to be seen in patients who are over 65 years of age, who have previous history of peptic ulcer disease, patients using corticosteroids, anticoagulants or those taking aspirin. If long term use of NSAIDS has been in use, then the risk increases significantly. Any regime that has been carried out for less than ten days is not associated with any toxic effects, and is easily tolerated, except in the susceptible patients. (Ong et al, 2007, pp 29)
In brain, the complications are thought to arise due to increase in the water retention which can cause cerebral edema. The renal adverse effects caused by NSAIDS include renal arteriolar constriction, renal tubular necrosis, and congestive cardiac failure, cirrhosis of liver, renovascular disease, renal failure, hyperkalemia, renal papillary necrosis, acute interstitial nephritis, nephritic syndrome and renal lesions. (Derle, 2006, pp. 411)
Cardiovascular risks are another complication that is expected in the use of NSAIDS. COX2 inhibitors and other NSAIDS in studies have shown high risk of causing serious vascular events. This has been reported to be as high as 40% in such cases.
Gastrointestinal perforation, hemorrhage and ulcer formation risks increase in patients who take aspirin for rheumatoid arthritis. Those that are using corticosteroids or anticoagulants alongside are at an even more of a risk. Renal failure can ensue in such patients, with congestive heart failure as another of such complications. Drugs such rofecoxib have the highest potential of causing cardiovascular events, followed by diclofenic, meloxicam, and ibuprofen. This finding has increased much concern among the physicians who have been prescribing NSAIDS as chronic use medications, especially in the prevention of cardiac events, like myocardial infarction. The increase in the cardiac events is many time higher than the placebo controls that have been used. (NPS, NP, 2006)
There is an established relationship between the COX and the membrane phospholipids in the mammalian cells. The rat cell studies have demonstrated a close metabolic relation ship of both and COX is seen to be regulatory in nature for the phospholipids, especially the phosphotidylcholine or the PC. Phosphotidylcholine is a major membrane phospholipid in mammalian cells, and is seen to have a metabolic relationship in the maintenance of PC synthesis and the prostaglandins endogenously synthesized by COX in rat renal papilla. COX 2 inhibition affects the metabolism of PC significantly, while is done so marginally with COX1 inhibition. The study that was conducted by Tome et al (2003) was able to show that COX2 mediated PG2 synthesis is a PC regulator rat tissues. This theory was also able to establish the possible reason of renal toxicity that is seen in the mammals due to the use of NSAIDS. (Tome et al, 2003, pp 252)
The current literature is filled with articles that explain the effect of aspirin and other NSAIDS on the activity of the platelets and how this can be used to an advantage. Aspirin is able to reversibly inhibit the activity of the cyclooxygenase and inhibits thromboxane production. The thromboxane activity decreases in 7 to 10 days. This leads to the thinning of the blood or the decrease in the coagulation of the platelets, which can help prevent any serious sequelae in atherosclerosis or heart patients. Those patients with high C reactive protein levels in the blood are seen to benefit the most from aspirin therapy. (Jneid et al, 2003, pp 1148) The benefits of aspirin in the study analysis among men were seen to be in those patients whose C proteins levels were in the highest quartile. The study suggested the major mechanism of action of aspirin through its anti-inflammatory effects. (Jneid et al, 2003, pp 1148)
However the role of COX 2 in the promotion and in the prevention of thrombogenesis is still unclear and may even be conflicting at times. It may show a different activity in different states of the vessels, for example in endothelium in healthy or diseased conditions and in atherothrombosis. The role of various mediators such as endoperoxidase is also under review, but so far the limited knowledge about the effects of these mediators in the progression of thrombus and platelet formation. (Kloner, 2004, pp 57)
What Effects Have Resulted From the Isoforms of Nsaids
The introduction of COX 2 inhibitors has increased the use of NSAIDS to some extent. This is because COX 2 inhibitors have shown good response against gastrointestinal ulcer formation. The efficacy of these drugs in this regard has been compared to the use of proton pump inhibitors in protecting the GI mucosa from erosion and ulceration.. (Ong et al, 2007, pp 28)
The COX 2 inhibitors are responsible for a variety of functions in the body. Some of these actions are homeostatic, but largely these actions are proinflammatory in nature.
The three different forms of the COX are the main way of classifying these drugs into genres. For example, the COX1 inhibitors are known as the conventional NSAIDS. The COX2 inhibitors are termed as the coxibs and the COX 3 inhibitors are known as acetaminophen. This difference in the makeup is the main method of identifying their indications for use. Primarily, these differences in the makeup of the drugs lead to variable potencies and duration of actions, and the methods of elimination from the body. Other methods of distinction include the potential to cause ulcers or cause bleedings. (Ogbru, 2007, Para 3)
The COX method of classification is but one method of classifying NSAIDS. The previous was the receptors on which certain NSAIDS acted on. The other method is classification based on the chemical structure of the NSAID. Most of these are carboxylic acids, but others are enolic acids. The carboxylic acids include the salicylates, carbocyclic and heterocyclic acid derivatives, fenamic acid derivatives, propionic acid derivatives, and phenyl acetic acid derivatives. The enolic acids contain oxicam derivative and pyrazoles. The entire above mentioned are the acidic drugs of NSAIDS. The non acidic drugs in NSAIDS include nabumenton. (Derle, Gujar and Sagar, 2006, pp. 409-410)
The recent research has shown that it is the COX 2 inhibitors that mediate a more intense response in the body regarding pain and inflammation. This may explain the relatively lesser functioning and efficacy of the COX 1 inhibitors in the relief of pain in the patients. (Vane and Botting, 1998, pp. 11) Also, the COX 2 inhibitors are less likely to cause irritation of the gastric mucosa. There is suggestion that COX 2 inhibitors can be less damaging to renal function. These drugs have also shown a less negative response on the adherence of the platelets, and therefore do not contribute to the increased bleeding times and clotting times. (Hoff, 1999, NP)
Recent studies have resulted in a fierce debate about the safety of the COX 2 inhibitors use. The particular drug in question was the refocoxib drug that was introduced into the market the company Merck. The aim of this drug was to reduce the negative effects of the NSAIDS on the gastrointestinal mucosa. This drug was therefore introduced in the market for the treatment of acute pain, menstrual pain and rheumatoid arthritis. The researches in the drug as well as other similar class of drugs showed that these patients were twice at risk of a heart attack than those taking placebos. This risk was seen to be as high as 5 times in the case of refocoxib, along with a high risk of stroke, venous thrombosis and hypertension. Due to these extremely disturbing findings, the class of this drug was removed from the market. (Fouad, 2004, pp 214)
Conclusions
NSAIDS remain a drug of choice in many cases of pain, inflammation and fever. These drugs have for years prevented many patients from pain and symptoms associated with severe disease, cancer and surgery. Arthritic patients and those suffering from cardiac complications are another set of patients that benefit from the use of NSAIDS. NSAIDS show promise in the reduction of colon cancers and help to improve the ophthalmic complications that are associated with increased intraocular pressures.
Yet their side effects and their toxicity is a factor that in many cases is overlooked. This has led to high incidences of the gastric mucosa ulceration, which in turn causes significant morbidity and mortality among the patients. The introduction of the COX2 inhibitors was thought to be a safer alternative to the COX 1 inhibitors due to their selective activity in reducing pain and nociceptor activity. The effects were even documented to be superior to the activity of non selective COX inhibitors. However, the withdrawal of the recent refocoxib and similar drugs along with proof of twice the increase of heart and other related complications have increased concern about the use of these drugs in normal practice. This also brings to light the number of patients around the world who are using NSAIDS as chronic medication for a variety of reasons, and raises concern about the number of unexpected and preventable deaths that the use of NSAIDS can lead to. Until there is conclusive evidence that NSAIDS negative effects have been eliminated and their beneficial properties retained, the continuation of this drug use is risky. It therefore becomes the clinician or the health provider’s responsibility to ensure that NSAIDS are prescribed only if the risks. Other wise other safer alternatives should be brought into consideration.
References
Sarkar, Amrita (2005) Effect of NSAIDS on Cyclooxygenase 1. Web.
Simmons, Daniel L., Wagner, David and Westover, Kenneth (2000) Non-Steroidal Anti-inflammatory Drugs, Acetaminophen, Cyclooxygenase 2, and Fever. Journal of Clinical and Infectious Diseases, 2000; 31 (Suppl 5): S211-8.
Ong, C. K.S., Lirk, P., Tan, C.H., and Seymour, R. A. (2007) An Evidence Based Update on Nonsteroidal Anti-Inflammatory Drugs. Clinical Medicine and Research, Vol. 5 No. 1: 19-34.
CERTs Research: Nonsteroidal Anti-inflammatory Drugs (NSAIDs) (2003) Program Brief. Agency for Healthcare Research and Quality, Rockville, MD. AHRQ Publication No. 06-P001. Web.
Gotlieb, David (2005) COX1 and 2: The Cyclooxygenase Systems. Web.
Definition Prostaglandin Endoperoxidase. Cancer web(2007). Web.
Derle, DV, Gujar, KN and Sagar, BSH (2006) Adverse Effects Associated With the Use of Nonsteroidal Anti-inflammatory Drugs: An Overview. Indian Journal of Pharmaceutical Sciences, Vol. 68, Issue 4 page 409-414.
Fuoad, M. (2004) The Withdrawal of Rofecoxib (Vioxx) from the Market: Questioning the Safety of Other Anti COX 2 Drugs. ASJOG, Vol. 1, 2004, pp 214-215.
Hoff, G L. (1999) Non Steroidal Anti Inflammatory Drugs: Where are We Today? Orthopedic Technology Review, Vol. 1, No. 3. Web.
Melanga, Gerard (2007) Non-Steroidal Anti Inflammatory Drugs (NSAIDS) in the Treatment of Acute Low Back Pain. Web.
Hani Jneid, Deepak L Bhatt, Roberto Corti, Juan J Badimon, Valentin Fuster, and Gary S Francis (2003) Aspirin and Clopidogrel in Acute Coronary Syndromes. Therapeutic Insights from the CURE Study Archives of Internal Medicine, Vol. 163, No. 10, 1145-1153.
Clearfield, Harris R (1992) Management of NSAID Induced Ulcer Disease_ Non Steroidal Anti Inflammatory Drugs. American Family Physician. Web.
DeRuiter, Jack, Principles of Drug Actions, fall (2002) Web.
Goodwin, James S., Ceuppens, Jan L. and Rodriguez, Martin A. (2005) Inhibition of Rheumatoid Factor Production by Non-Steroidal Anti-Inflammatory Drugs. Journal of Inflammation, Vol. 8.
Cashman, JN (1996) The Mechanism of Action of NSAIDS in Analgesia. Drugs, 1996, supplement 5: 13-23.
Vane, John R. and Botting R M (1998) Mechanism of Action of Anti-inflammatory Drugs, 1998. International Journal of Tissue Reaction, 1998; 20(1):3-15.
Vane, John R., Matthew L. Madsen, Philip M. Robertson, Regiman M. Botting and Daniel L Simmons, (1998) Induction of an Acetaminophen-Sensitive Cyclooxygenase with Reduced Sensitivity to Non Steroid Anti Inflammatory Drugs. PNAS, Vol. 96. Issue 6, 3275-3280.
Vane, John R, Timothy D. Warner, Francesco Guilliano, Ivana VOjnovic, Antoaneta Bukasa, and Jane A Mitchell (1999) Non Steroid Selectivities for Cyclo Oxygenase 1Rather Than Cyclooxygenase 2 are Associated with Human Gastrointestinal Toxicity; A Full in Vitro Analysis. PNAS, Vol. 96, Issue 13, 7563- 7568.
Vane, John R and Botting R M (2003) The Mechanism of Action of NSAIDS. Thrombosis Research, Vol. 110, Issues 5-6, 255-258.
Townsend, Kirk P and Pratico, Domenico (2005) Novel Therapeutic Opportunities for Alzheimer’s disease: Focus on Non Steroidal Anti Inflammatory Drugs. The FASEB Journal, 2005, 19: 1592-1601.
Barclay, Laurie (2006) Aspirin or NSAIDS May Reduce Risk of Colorectal Cancer. Web.
Shaik, Madhu Sudhan, Chatterjee, Abhijit and Singh, Mandip (2004) Effect of a Selective Cyclooxygenase-2 Inhibitor, Nimesulide, on the Growth of Lung Tumors and Their Expression of Cyclooxygenase-2 and Peroxisome Proliferators- Activated Receptor-γ. Clinical Cancer Research Vol. 10, 1521-1529.
Fernández-Tome, María, Kraemer, Leticia, Federman, Sebastián Cembal, Favale, Nicolás, Speziale, Emir and Sterin-Speziale, Norma (2003) COX-2 Mediated PGD2 Synthesis Regulates Phosphatidylcholine Biosynthesis in Rat Renal Papillary Tissue. Biochemical Pharmacology, Vol. 67, Issue 2, 245-254.
Myceck, Mary J, Harvey, Richard A, and Champe, Pamela C, (2000). Lippincott’s Illustrated Reviews. Pharmacology, 2nd Edition. Lippincott Williams and Wilkins.
National Institute of Neurological Disorders and Stroke (2001) Popular Pain Analgesics Found to Affect Central Nervous System: Study Identifies Both Peripheral and CNS Mechanisms of Action of NSAID Use. Web.
Ogbru, Omudhome (2007) Nonsteroidal Anti Inflammatory Drugs. Web.
Allain, P., (2007) Cyclooxygenase Inhibitors, NSAID- General Features. Web.
Lipsky, Peter E., Brooks, Peter, Crofford, Leslie J., DuBois, Raymond, Graham, David, Simon, Lee S., van de Putte, Leo B. A., Abramson, Steven B. (2000) Unresolved Issues in the Role of Cyclooxygenase-2 in Normal Physiologic Processes and Disease. Arch Intern Med. 2000; 160:913-920.
Kloner, Robert A. and Dai Wnagde (2004) Relationship between Cyclooxygenase-2 Inhibition and Thrombogenesis. Journal of Cardiovascular Pharmacology and Therapeutics, Vol. 9, No. 1, 51-59.
Leslie, William, Drajer, Deborah, Frame, David and Subongkot, Suphat (2003) Selective CycloOxygenase-2 Inhibition; a Target in Cancer Prevention and Treatment. Pharmacotherapy 23(1): 9-28, 2003.