Abstract
Communication is a key component of any type of relationship. When it comes to the patient-nurse relationship, the quality of communication serves as an indicator of patient satisfaction. In the postoperative setting, pain management is one of the prioritized issues. However, patients with limited English proficiency (LEP) may struggle to communicate their pain. Mere reliance on such ways of pain manifestation as body language, facial expressions, or vital signs is not as sufficient as a patient’s self-report. The implementation of the Universal Pain Assessment tool is intended to help care providers assess pain according to patients’ needs related to language.
The goal is to use a simple and reliable tool, customized to the patient’s language that will enable nurses to assess pain earlier and more effectively for timely and adequate interventions. Studies have shown that limited LEP is linked to higher levels of pain, greater barriers to pain management, and lower patient satisfaction. The implementation of a cross-culturally adapted pain scale will minimize the language barrier, eliminate a patient’s level of anxiety, and improve the overall quality of health care provided to the population with LEP.
Introduction
The issue of timely retrieval of health-related information from patients is the core of the successful and effective work of health care professionals. The relationship based on clear communication between patient and nurse is an essential contributor to safe health care and successful recovery. In recent years, more and more professional and scholarly attention is paid to the question of effective therapeutic communication.
Researchers agree that nurses play the role of patients’ advocates and must facilitate professional and therapeutic relationships with them (Amoah, 2019). However, numerous obstacles might impede both nurses’ care and patients’ reporting a problem. Many people face significant constraints related to health conditions and cultural particularities that might obstruct the smooth exchange of information. One such issue is language proficiency.
Language as a mediating means that helps to establish a meaningful connection between people is of critical importance to the health care setting. In the USA, patients with a low level of English language knowledge feel anxiety and intimidation when communicating with a nurse or a doctor. Indeed, the multi-cultural society that the USA is becoming now includes diverse foreign-born patient groups whose level of English language proficiency is insufficient. As a consequence, a significant number of people fail to engage in health care and do not receive timely identification of a health problem and care provision.
Moreover, when it comes to reporting pain, which is one of the critical determinants that help medical workers locate the problematic health issue, Limited English Proficiency (LEP) patients are exposed to delayed consulting, diagnosis, and treatment.
The problem of the timely assistance of patients experiencing pain is pertinent to the provision of care to patients who recover after surgeries. Postoperative health care is centered on monitoring patients’ healing, the recovery process, and comfort. At the same time, pain is an inevitable element of postoperative recovery, which must be accurately and timely addressed by medical personnel.
In the case of non-English speaking patients or those with LEP, the process of communication becomes a challenge for both nurses and patients. The health care workers’ command in foreign languages might be insufficient, and continuous use of the services of a translator might be both time- and resource-consuming. Thus, the difficulties in communicating pain with foreign-born patients in the postoperative setting obstruct the identification of necessary means of care that complicates nurses’ work and causes discomfort, anxiety, and suffering to patients.
In general, universal pain assessment tools are applied to populations with limited communication abilities, such as patients with intellectual disabilities and people with temporomandibular joint syndrome (Dugashvili, Van den Berghe, Menabde, Janelidze, & Marks, 2017). In other words, the universal pain assessment is currently applicable in cases when a patient is either physically unable to utter words or his or her speech clarity is diminished due to intellectual impairment.
Non-verbal communication plays a more significant role in the process of information exchange with such patients. With the help of universally understandable tools, nurses can collect pain-related data from the patient and assess his or her level of pain accurately and realistically. However, when a patient with no impairment of either intellectual development or articulatory apparatus is served at a health care facility, his or her ability to communicate pain-related information is similarly inefficient.
The combination of the two aspects, the postoperative setting and the lack of proficiency in the English language, is at the center of the proposed research. Patients who have limited abilities to communicate in English are exposed to diminished quality of health care and are at risk of being underserved. It might have particularly adverse outcomes for the population served at postoperative units.
At the same time, the growing number of foreign-born citizens with LEP seeking medical help imposes difficulties in the work of nurses and doctors. Their execution of professional duties is paralyzed by the complicated process of therapeutic communication with the help of interpreters if such are available at a given time. Therefore, it is evident that there is a need for the development of a pain assessment tool that would address these difficulties and provide an opportunity for timely and effective patient care.
Problem Statement
Today, high-quality professional health care is a priority in the USA medical sphere. Health care providers must ensure that the health needs of all the patients are met. Therefore, due to the growing number of citizens with LEP, the underserved population increases. The communication of painful experiences in the postoperative setting is a crucial element of patients’ well-being and comfort maintenance. The problem under investigation involves a language barrier between patients with LEP and nurses that imposes anxiety and failure to report pain characteristics on the patients’ part and to conduct pain assessment and provide timely and relevant care on the nurses’ part.
The majority of inter-cultural tools either involve verbal communication with the help of an interpreter or require a patient to speak a particular level of English. Thus, it is vitally important to develop and implement a simple and effective universal pain assessment tool capable of easy retrieval of information from LEP patients and providing nurses with sufficient knowledge about patients’ pain levels. The problem will be tackled using qualitative research, which will allow for developing a universal pain assessment tool and testing it in a postoperative setting. The results will demonstrate the effectiveness of the intervention in the facilitation of nurse-patient pain-related communication.
Background
The issue of therapeutic communication is well-researched and marked by some insights that clarify the scope of barriers that prevail in nurse-patient communication. According to Amoah et al. (2019), several patient-related obstacles might be identified as those obstructing the effective exchange of information between health care employees and patients. They include “personal/social characteristics, patient-nurse relationship, language barriers, misconception, and pain” (Amoah et al., 2019, p. 4). All of these issues might cause misunderstanding or become a reason for ineffective communication. When applying these findings to the investigated problem of pain assessment of non-English speaking patients in postoperative units, the collision of two barriers, including pain and language, becomes a significant concern.
Indeed, people recovering from surgical interventions commonly experience severe pain and need assistance in its management. As Amoah et al. (2019) state, when a patient is in pain, he or she experiences mood changes; consequently, the style and clarity of communication might be impaired. For a patient and a nurse who does not speak the same language at a sufficient level, the issue of pain might be crucial within the realm of therapeutic communication. In such a situation, durable verbal communication with the help of an interpreter might result in unfavorable patient outcomes. These considerations are particularly appropriate within the context of the health care system of Hudson County.
Currently, the population of Hudson County, to which New Jersey belongs, consists of multiple ethnicities and races. According to the statistical, demographic data presented by the United States Census Bureau (2018), Hudson County is a home to a population, 42.8% of which are foreign-born individuals, while the percentage of the same population across the United States equals 13.5%. Importantly, the diversity here is marked by the prevalence of Hispanic residents. There are 42.9 % Hispanic or Latino compared to a nationwide percentage, which is 18.3% (United States Census Bureau, 2018, para. 3). Such demographic characteristics imply a variety of non-English speakers who might struggle to communicate in English in different public settings, including health care.
Moreover, Hudson County is a major port of entry for immigrants to the United States. It also is a significant employment center that provides workplaces for immigrants from foreign countries. Among the most common nations of birth for foreign-born residents of Hudson County, Cuba, the Dominican Republic, Ecuador, Philippines, and India are the leading ones in the number of migrants.
These people reside and work in Jersey City and other municipalities of Hudson County; thus, they are entitled to access quality health care. Therefore, it is a priority for the local health care facilities to address the culture and language-related concerns of this large population. Since the majority of foreign-born residents have limited expertise in the English language, Jersey City Medical Center will benefit from a pain assessment tool that is easy to use and customized according to the patients’ language.
The inability of patients with LEP to communicate in English imposes anxiety and discomfort in relationships with nurses at medical institutions. For the development of an effective and universal pain assessment tool, it is necessary to prioritize the ethnicities that have the largest number of residents. Since the majority of foreign-born residents of Hudson County perceive Spanish and Hindi as their native languages, the tool customized according to these languages would be the most applicable. There have been multiple successful attempts to translate pain assessment interventions into foreign languages to facilitate the quality of service to patients with LEP (Bansal, Gudala, Lavudiya, Ghai, & Arora, 2016; Gudala, Ghai, & Bansal, 2017; Martin-Fernandez et al., 2017; Mokhtarinia, Hosseini, Maleki-Ghahfarokhi, Gabel, & Zohrabi, 2018).
However, most of the assessment tools involve active verbal communication or descriptive written means that help nurses to extract information concerning pain. On the contrary, a simple universal pain assessment tool might provide a more effective and time-efficient opportunity to minimize verbal interaction with a patient who does not speak English and assess pain in a timely and accurate manner.
Mostly, the universal pain assessment is used to assess pain for patients with limited communication abilities. It has been identified that pain in patients with intellectual disabilities is less frequently identified due to the difficulties of communication (Doody & Bailey, 2017). Since communicative failure is likely for the population with LEP, the same issue with pain identification is relevant. However, despite the existing barriers, early assessment of pain is crucial because it helps to “enhance the quality of life for those with intellectual disability” (Doody & Bailey, 2017, p. 159). Pain assessment is the initial and most important step in the provision of care that is aimed at achieving relief.
When this procedure is conducted by improper means due to the complicated communication with non-English speaking patients, there occurs a high probability of inadequate pain management. As a consequence of that, “unrelieved pain may cause unnecessary suffering, anxiety, fear, anger, and depression to the patients” (Christie, Oluseyi, & Olufunke, 2018, p. 165). Therefore, the universal pain assessment tool is the best option to identify pain in patients with LEP and avoid possible complications associated with inadequate pain management.
Such a universal pain assessment tool embodies non-verbal means of information exchange that is easy to understand for the multi-cultural and poly-linguistic population. According to Christie et al. (2018), pain should be assessed based on both quantitative and qualitative dimensions. Therefore, a verbal description is vital in the evaluation of pain characteristics and provides a nurse with an opportunity not only to locate pain but also to estimate its severity.
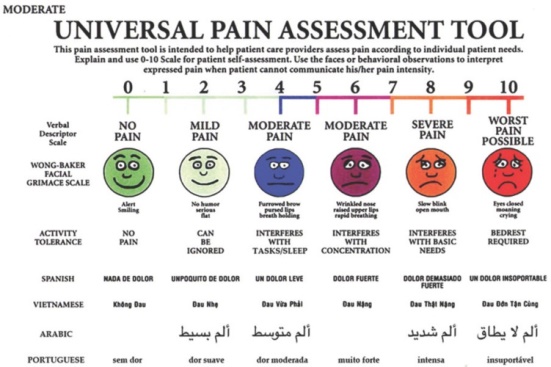
It is required to help medical personnel in choosing appropriate medication or pain relief options. While the quantity of pain might be assessed with the help of a scale, the quality of pain requires a verbal description. An example of a universal tool that combines the two dimensions of pain, including quantity and quality, was used by Dugashvili et al. (2017). It is presented in Appendix A and depicts the facial expressions representing the quantity of pain and verbal descriptions in several languages to denote the quality of pain. Thus, such a multi-linguistic tool might be used as a prototype for the development of a pain assessment method that would effectively serve patients with LEP residing in Hudson County.
Purpose
Considering the vast concerns related to the patient outcomes associated with pain assessment of the population with LEP, the development of a universal culturally relevant pain assessment tool is of vital importance to the medical institutions of Hudson County. Therefore, the purpose of this capstone project is to develop and test a simple and cost-effective tool that would enable nurses to evaluate patients’ postoperative pain decrease their anxiety related to limited English proficiency. Before the intervention, the tool should be explained to the patient by the preoperative nurse during the initial admission.
The introduction of the tool should be conducted with an interpreter or language line. The tool will be included in the patient’s chart and will be available to the postoperative nurse to assess pain during the recovery process. In such a manner, both patients and nurses will be informed about the procedure of tool application and have an opportunity to benefit from its usage.
Overall, the project attempts to develop and test the effectiveness of the universal pain assessment tool. Its goal is to compare the pain management outcomes of patients with LEP admitted to the postoperative unit who used the tool with the outcomes for those whose pain was assessed by other means. The issue under investigation is of great significance to nursing in general since it addresses the issues which medical personnel faces daily and which complicates their work with postoperative patients who do not speak English.
Also, it will benefit the organization in the face of Jersey City Medical Center and its leadership due to the potential contribution to the development of a cost-effective and simple tool capable of facilitating patient-nurse communication in populations with LEP, which prevails in Hudson County.
The Nature of the Project
The project will be conducted by utilizing qualitative methodologies. The quasi-experimental study is considered to be the best option that will enable achieving the purpose of the capstone project. Unlike other methodologies, the quasi-experimental study allows for implementing the tool in a real setting, comparing the patient outcomes for two groups of participants, including those exposed to the currently investigated pain assessment procedure and those not exposed to the intervention.
Also, the feedback from the nursing staff will allow for adequate interpretation of the results. At the first stage of the research, the tool will be developed and customized to the patients’ most commonly spoken languages, which are Spanish and Hindi. In the second stage, questionnaires will be introduced to the nurses before and after the utilization of the pain assessment tool. Comparative analysis of patients’ outcomes and comfort with reporting pain before and after the application of the tool will show how effective the pain assessment tool is.
Research Question
Based on the purpose and nature of the capstone project, the research question addresses the issue of pain assessment for culturally diverse populations who do not speak English at a sufficient level. The PICO question is formulated as follows: In the postoperative patients with limited English proficiency (P), will the utilization of the universal pain assessment tool (I), result in better pain management strategies and decreased language-related anxiety (O), as compared to patients exposed to traditional pain assessment procedures (C)?.
Summary
In summation, the proposed capstone project is necessitated by the prevalent rate of foreign-born residents in Hudson County. Due to the LEP of this population, they experience insufficient health care and anxiety as a result of inefficient nurse-patient communication at medical facilities. Pain assessment in a postoperative setting is a crucial element of proper facilitation of patients’ recovery. A simple and cost-effective universal pain assessment tool customized according to patients’ languages will provide multiple benefits. It will ensure patients’ comfort and better recovery, nurses’ timely and more effective choice of pain management strategies, and the organization’s readiness to serve the multi-cultural population.
Literature Review
Introduction
The extensive body of academic literature on the topic of pain assessment in an inter-cultural setting provides an opportunity to collect a substantial set of findings. The capstone project will be based on the currently available results of work in the field of research on the topic to draw a reliable ground for the study. Overall, the sources used as a theoretical and evidential basis provide an overview of the achievement in the field of pain assessment in culturally diverse populations.
Current Findings
The relevance of cross-cultural adaptation of health care procedures and tools gains more relevance in the professional literature due to the trends of globalization that impose intensified migration and the emergence of diverse societies. The study on the barriers to health care access that consumers from culturally and linguistically diverse backgrounds experience has examined the scope of obstacles (Harrison et al., 2020).
It has been found that the majority of non-English speaking patients struggle to access health care, find proper interpretation, and receive adequate health care due to the limited knowledge of English. To address this problem, specific studies have contributed to the investigation of the process of customizing the most crucial health care procedures to the requirements of linguistically diverse patients.
The translation and cross-cultural adaptation of pain assessment interventions have been conducted for several conditions and languages. Indeed, Mokhtarinia et al. (2018) have adapted and tested the spine functional index in the Persian language and found that the translated version provides effective results. Similarly, a verbal pain descriptor was developed specifically for Tswana-speaking patients to assess their low back pain (Yazbek, Stewart, & Bentley, 2018).
This study has demonstrated that patients are more likely to report pain, not in numbers but quality through the description. The same kind of pain was addressed by Bansal et al. (2016), who adapted the pain measuring scale to Hindi-speaking patients. The overall results indicated positive pain assessment outcomes and a reliable basis for further implementation in similar settings. Another pain assessment tool for patients with osteoarthritis has shown positive outcomes for Hispanic patients (Martin-Fernandez et al., 2017). It indicates that the adapted version is a useful tool in assessing patients’ self-perceived health conditions.
All the above-mentioned studies have translated pain assessment tools into different languages and addressed various commonly experienced pain types prevailing in multi-cultural patient populations. However, there is limited attention paid to the process of recovery in a postoperative setting, where pain management is crucial. Moreover, the majority of the analyzed studies refer to the tools that use either a vast part of verbal communication between a nurse and a patient or a broad written description of pain quality (Bansal et al., 2016; Martin-Fernandez et al., 2017). These gaps might be filled with the research that addresses the needs of postoperative patients with LEP and their pain assessment with the help of a simple tool based on minimal verbal interaction.
Conclusion
To summarize, the literature review provides a solid basis for the consecutive investigation of the cross-cultural adaptation of pain assessment tools. The identified gap in the literature accentuates the necessity to address the needs of postoperative patients whose pain management is a priority for fast recovery. The overall positive results of the currently available studies signalize that the direction of research is fruitful and important to the target population. The development and testing of a simple and cost-effective pain assessment tool will contribute to the scope of academic literature and will improve the quality of health care service provided to patients with LEP residing in Hudson County.
References
Amoah, V. M. K., Anokye, R. Boakye, D. S., Acheampong, E., Budu-Ainooson, A., Okyere, E., Kumi-Boateng, G.,… Afriyie, J. O. (2019). A qualitative assessment of perceived barriers to effective therapeutic communication among nurses and patients. BMC Nursing, 18(4), 1-8. Web.
Bansal, D., Gudala, K., Lavudiya, S., Ghai, B., & Arora, P. (2016). Translation, adaptation, and validation of Hindi version of the pain catastrophizing scale in patients with chronic low back pain for use in India. Pain Medicine, 17, 1848-1858. Web.
Christie, O. O., Oluseyi, A. O., & Olufunke, O. D. (2018). Factors associated with utilization of pain assessment tools in pain management among nurses in selected hospitals in Ekiti State. International Journal of Caring Sciences, 11(1), 163-170.
Doody, O., & Bailey, M. E. (2017). Pain and pain assessment in people with intellectual disability: Issues and challenges in practice. British Journal of Learning Disabilities, 45, 157-165. Web.
Dugashvili, G., Van den Berghe, L., Menabde, G., Janelidze, M., & Marks, L. (2017). Use of the universal pain assessment tool for evaluating pain associated with TMD in youngsters with an intellectual disability. Medicina Oral, Patologia Oral y Cirugia Bucal, 22(1), 88-94. Web.
Gudala, K., Ghai, B., & Bansal, D. (2017). Neuropathic pain assessment with the PainDETECT Questionnaire: Cross‐cultural adaptation and psychometric evaluation to Hindi. Pain Practice, 17(8), 1042-1049. Web.
Harrison, R., Walton, M., Chitkara, U., Manias, E., Chauhan, A., Latanik, M., & Leone, D. (2020). Beyond translation: Engaging with culturally and linguistically diverse consumers. Health Expectations: An International Journal of Public Participation in Health Care & Health Policy, 23, 159-168. Web.
United States Census Bureau. (2018). Hudson County, New Jersey; New Jersey; United States. Web.
Martin-Fernandez, J., Gray-Laymon, P., Molina-Siguero, A., Martinez-Martin, J., Garcia-Maroto, R., Garcia-Sanchez, I.,… Bilbao, A. (2017). Cross-cultural adaptation and validation of the Spanish version of the Oxford Hip Score in patients with hip osteoarthritis. BMC Musculoskeletal Disorders, 18(205), 1-11. Web.
Mokhtarinia, H. R., Hosseini, A., Maleki-Ghahfarokhi, A., Gabel, C. P., & Zohrabi, M. (2018). Cross-cultural adaptation, validity, and reliability of the Persian version of the Spine Functional Index. Health and Quality of Life Outcomes, 16(95), 1-9. Web.
Yazbek, M., Stewart, A.V. & Bentley, A.. (2018). A verbal descriptor incremental pain scale developed by South African Tswana-speaking patients with low back pain. South African Journal of Physiotherapy, 74(1), 1-6. Web.
Appendix A