Abstract
Objectives
This research was conducted to determine deficiencies of autonomy in patient management at the end of life hence; determine conflicts in autonomy and how they impact on nurse capacity to exercise patient advocacy and determine and identify mechanism through which nursing principles of practices could be exploited in order to provide foundation for enhancing autonomy and capacity of nurses to autonomously represent the patient.
Methods
The study used phenomenology method that was delivered through use of reflective exploratory approach. The researcher used participant observation in order to collect data on patient experiences. The action based approach was used to reflect on impacts of decisions and treatment options on the patient. The data was analyzed by using categorical data analysis that involved normalization of the observations followed by descriptive analysis of observation, reflection and emancipatory steps on actions taken.
Results
The study identified autonomy influences the capacity of nurses to deliver duty of care with regard to patient advocacy. The nurse as patient advocate has limited authority to influence patient relative’s decisions on treatment of a patient at the end of life. Power distance between nurse and physician determines capacity of a nurse to question physician authority. The patient care management at the end of life is not a function of principle of beneficence or principle of non-malfeasance. Therefore patients continue to suffer due to loss of nurse autonomy and incapacity of a nurse as a patient advocate. The nurse is not in a position to refuse treatment options that could not result to positive health outcomes on patient.
Significance
Reflection should be used to develop nursing practice and enhance the value of evidence based research. There should be policy development towards protection of nurses who demonstrate patient advocacy against treatment options that patient relatives of physician may propose. The nurse should have authority over patient best interests at the end of life care.
Introduction
Background of the study
Nursing reflection on experiences forms foundation for development of new procedures and policies for patient management (Hillard, 2006, pp.36-8). Reflection makes it possible for nurses to examine actions taken with respect to patient treatment, relate application of the action to nursing practice and develop structures that could be used to shape nursing cultural mode of actions based on nursing principles of practice, rationality of the decisions based on autonomy (Allin & Turnock, 2007a, p.16). Oncology nurses are mandated to promote health and protect patients. Autonomy application restricts capacity of nurses to deliver patient advocacy (Young & Paterson, 2007, p.48).
Patient advocacy requires patient understanding of their medical conditions in order to implement treatment options, provide education on the disease development and discharge duty of care. As patient advocates, nurses forge for consultation with physicians and improvement of communication in order to deliver equitable healthcare to patients (cf. Wopereis et al, 2010, p.245).
Nurses have duty to speak on behalf of patients and ensure appropriate end of life care is given to patients (NMC, 2004a, p.82). The nursing care should therefore alleviate patient suffering. This implies, conduct of nurse should be a function of ethical and moral consideration. Nurses should demonstrate competence in applying different nursing principles of practice (Gaines & Sanford-Ring, 2004, p.21). There should be a point where a nurse authority over a patient should exceed the patient relative’s control of patient custody. The nursing principles should provide limit where patient relatives could have control over clinical interventions of a patient. The choice of chemotherapies that are under trial should be beyond the patient relative’s rights (Cooper & Spencer-Dave, 2006, p.607).
Problem under investigation
The principle of autonomy influences level of interaction of nurses and physician and impacts on nurse capacity to patient advocacy (John & Freshwater, 2004, pp.35-9). The nurse as educator of patient and patient relatives should have capacity to refuse treatment that is being proposed on a patient. The capacity of a nurse to implement right of patient refusal of treatment lacks framework of autonomy (John, 2004, pp.24-6).
This is due to conflicts of interests that may exist amongst nurse’s wishes for patient care management at end of life, patient relative’s wishes for treatment options that nurses consider to have no clinical benefit to patient, trade off between a nurse participating in patient suffering and physician failure to consult nurses on treatment option feasibility subject to autonomy (Gustafsson & Fagerberg, 2004, pp.270-74). Patient relatives could impose treatment options against the will of the nurses who have a better understanding on the patient clinical conditions. This places nurses roles at stake due to lack of definition of autonomy and instances when nurses voice on patient concerns should be considered and implemented (Leininger & McFarland, 2002, pp.112-8).
Conflict of interest emerges in patient informed consent and capacity to refuse the treatment (Alin & Turnock, 2007b, p.43). The nurse, in principle, ought to represent the patient in clinical decisions. Decrease in nurse capacity to represent patient has resulted into precedence applications where a patient is clinically given a protected period in order to evaluate their decisions for a treatment options (ANA, 2003, pp.26-8). This provision doesn’t take into account patient clinical condition development or values and goals of timely response to clinical problems and patient suffering (Chabeli & Muller, 2004a, pp.52-7).
A patient has no capability to make reasonable clinical contribution that could provide sustainable direction in clinical practice if the patient is in vegetative state. Spirituality care should take precedence (cf. Walkerden, 2005 [cited in Keen et al, eds.]). Conflicts of interests emerges when a nurse is supposed to respect patient autonomy, respect patient relative’s right to choose clinical treatment for their patient or nurses stance to maintain authority of nursing practice (Taylor, 2006, p.18).
The nurses are mandated to protect interests of a patient based on patient’s inadequate perspectives for treatment options (ANA, 2004, p.12), immaturity of the patient (Ghale & Lillyman, 2000, pp.12-5), patient consciousness and refuse patient relative’s demands for specific treatment options. In many cases, patient’s relatives win custody if the patient’s relatives demonstrate capacity to openness to possible clinical interventions. Communication, compassion and patience have been identified to contribute into sustainable clinical solution (Cornish & Jones, 2007, pp.130-2). Failure of patience, compassion and communication to result into a consensus sought to be managed by judicial interventions, where nurse takes priority for autonomy to protect patient in the event ethical committee on patient is not conclusive (cf. John & Freshwater, 2005, p.72).
This case study reports on Faizal. The case report reflects on Faizal end of life care and influence autonomy played a role in Faizal end of life care.
Case report
Faizal was diagnosed with Acute Lymphocytic Leukaemia (ALL). He failed to respond to chemotherapy treatment. Faizal relapsed twice and was diagnosed no code. The father of Faizal demonstrated commitment to have his son undergo another cycle of chemotherapy. The father had information that there were no hopes of saving his son Faizal. After a lengthy discussion on father wishes for his son to undergo the chemotherapy, there were disagreements between the Faizal Father and the physician. The physician, agreed to provide a chemotherapy that was under trial phase. The nurses were not happy with the decision for Faizal to undergo chemotherapy. The nurses knew the chemotherapy was not going to increase chances for the survival of Faizal. The nurses had no choice but to witness as Faizal suffered more pain due to chemotherapy. Faizal died a few days later while undergoing chemotherapy.
Goals and objectives
- To determine deficiencies of autonomy in patient management at the end of life hence or otherwise determine mechanism through which deficiencies I autonomy could be managed at patient end of life care
- To determine conflicts in autonomy and how they impact on nurse capacity to exercise patient advocacy
- To determine and identify mechanism through which nursing principles of practices could be exploited in order to provide foundation for enhancing autonomy and capacity of nurses to autonomously represent the patient.
Expected outcomes of the study
The study findings will provide opportunity for integrating nursing theories and nursing practice standards into promotion of autonomy, patient advocacy and nursing education programs. The findings of the study will play a leading role in development of skills and skills that nurses could apply in day-to-day patient management. The study findings will play a vital role in improving nurse’s conceptual development and reflection on patient treatment actions and provide foundation for nurses to reflect on nursing practice and methodologies that could be integrated into nursing practice to add value to patient care management.
The study outcomes will result into formulation and adoption of nursing based systems of professional development. The study findings will therefore be instrumental in determination of direction of nursing continuity of education.
The study outcomes will help in identification of rationale of nursing reflection as opposed to consideration of reflection as a measure of surveillance in a health system on nurses or physician patient management. the findings of the study will play a leading role in adoption of evidence based research in nursing, provide basis for change of organizational settings with regard to autonomy, contribute into evolution of nursing culture with respect to duty of care and enhance patient centered approaches in patient management.
Theoretical basis of the study
This study builds on John’s model of nursing reflection (John, 1995, pp.227-32). The primary role of John’s model of reflections is to facilitate nurses to efficiently and sustainably conduct therapeutic roles and implement clinical interventions that have medical benefit to the patient (John, 1995b, pp.24-6). The John’s model involves sequence of reflections that a nurse should undergo in order to examine experiences and their foundation in enhancing and creating clinical value to patient.
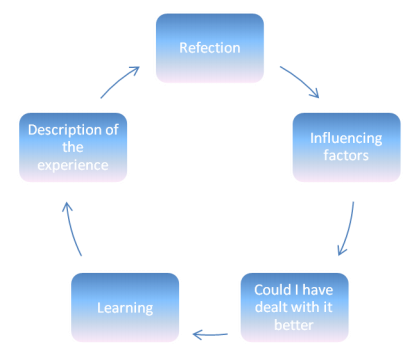
The John’s model (figure 1) involves documentation of the experience (Anderson et al, 2006, pp.183-8), reflection on rationale of the action that resulted into experience (TIP, 2006, p.23, 35-6), analysis of predisposing actions to the actions and assessment (Gaines & Sanford-Ring, 2004, p.2) and evaluation of the learning from the experience (Ghale & Lilyman, 2007, pp.65-6; 83-4). John’s model form s foundation for improving nursing learning through dynamism of reflection.
Organization of the dissertation
The rest of the dissertation is organized as follows. Chapter two reports on the literature review on reflection, application of principles of autonomy, beneficence, non-malfeasance and deficiencies of nursing principles of practice. Chapter three reports on the methodology of study, that was used to conduct the studies and Chapter four reports on results and discussion of the results that were obtained after collection of data. Chapter five reports on whether the study achieved its objectives and proposed recommendations based on study findings.
Literature review
This section reports on literature review on nurse reflection on nursing practice. It provides literature on autonomy and mechanism autonomy affects nursing principles of practice.
Oncology and paediatric nurses (Barr, 2007a, p.11; pp.16-9) spent a greater percentage of their career formulating care plans and managing children that suffer terminal illnesses that demand end of life care. Oncology and paediatric nurses form the foundation of health facility palliative care (Skinner, 2005, p.56). Thus, oncology nurses play an important role in provision of spirituality care that is required to manage patients suffering terminal illnesses (Kneafsey & Haigh, 2007, pp.834-7).
Studies on the children rights as patient have demonstrated that there exists a conflict of interest in application of children rights to refuse treatment, nurses role in educating the patient as well as nurses role as the advocate of the patient on the rights of choosing the appropriate treatment options and wishes that parents or the other members of health care fraternity may have (ANA, 2003, p.6). Therefore there is limited application of the nursing principle of patient informed consent and compliance with the nursing principle of patient autonomy (ANA, 2004, p.7).
The outcome on failure to adhere and adopt nursing practice to principle of autonomy or to act to the best interests of the patient is not in line with nurses’ duty of care. As a result, nurses and health care professionals demonstrate inadequacies of professional conduct in the mode of care that is advanced to patients that exhibit pain at their end of life (Leininger & McFarland, 2002, pp.114-6). Past studies have identified patients at the end of life receive inadequate care. The primary reason has been inadequacy of continuity of nursing education on patient management at the end of life.
Different terms have been used to define patient autonomy (Driscol & The, 2001, p.51). For instance the capacity to advocate for patient interests; the capability of a nurse to identify and prioritize the care plan management for a terminal illness patient; the ability of the paediatric nurse to act independently (Smith & Jack, 2005, pp.46-8) and under own freedom to advocate for the best treatment modality for a patient without being influenced by decisions of patient guardian, family members of members of the health facility staff to capacity to utilize nursing practice knowledge to make decisions that contribute into positive outcomes on patient care management (Clouder & Sellars, 2004, pp.265-8).
Although autonomy of patient contributes into different roles of nurses, there is existence of conflicts in decision making that affect scope of nurse to deliver sustainable patient advocacy (Moeti et al, 2004, pp.75-9). This implies, care management of a patient rests on understanding of the concept of patient autonomy as the most prioritized principle in nursing practice.
Some incidents contribute into ability of a nurse to violate autonomy principle (Hignett, 2005, p.315). This is because in practice, autonomy concept is not identified as a determinant factor to patient best interests for care (cf. Midgely, 2006, pp.339-42). As a result, autonomy is not practically applied in patient management at end of life. Different studies have identified patients suffering cardiovascular disorders (CVD) are not managed through use of autonomy principle (Foley et al, 2002, pp.184-6; p.88).
There is therefore minimal emotional support for patients at end of life care. The methods of pain interventions are not products of patient or nurse consultations. The reason that some studies cited was shortage of nurses which meant increased nurse workload impacts on capability of a nurse to advocate for patients (John, 1995b).
Autonomy as a determinant of health outcomes of a patient at the end of life should not be measured by nurse’s consultation with the physician. The nurse should have capacity to determine patients required level of autonomy that could contribute into best interests for the patient (MPBLW, 2006, pp.18-22). This implies, autonomy is a dependent variable that could vary based on patient’s case presentation. Autonomy as a nursing principle of practice should not be a function of professional status.
Autonomy doesn’t contribute into requirement for independence of nurses (Foley et al, 2002, pp.184-5). Autonomy ought to be a derivative of nurse-physician relationship that could add value to patient treatment and management. This implies autonomy ought to be relative and should be relational. It should be delivered through mutual respect and trust (Mamede & Schmidt, 2004, pp.1304-7). The poor management of autonomy has been stimulated by responsibilities vested on nursing institutions. The nursing programs don’t nurture environment for promoting healthcare professional conduct. As a result, autonomy is influenced by displayed behavior between the nurses and physician (NMC, 2006, pp.16-8).
In randomized blinded control studies, nurses failed to demonstrate credit to nursing programs role in development of nursing autonomy (Gaines & Sanford-Ring, 2004, pp.130-2). 84% of oncology nurses indicated personal and professional experiences were fundamental in nurse capacity to acquire autonomy that could contribute into responsibility and patient care accountability with regard to capacity to make decisions on behalf of the patients (cf. NMC, 2004c, pp.35-8). The observation created a scenario where nurses could be incapacitated to make decisions on behalf of their patients or to act at the capacity of patient advocates.
The nursing programs therefore require being evaluated and assessed on mechanism they deliver autonomy (NES, 2007, pp.9-12). This could help to prepare student nurses to role modeling as patient advocates through development of capacity to make independent rational patient care decisions. Nursing programs don’t expose student nurses to simulated experiences in their laboratory settings that could contribute into student nurse role playing development in preparation for their residence (Fazey et al, 2006, p.24).
The healthcare administration determines level nursing could implement the principle of autonomy (Peden-McAlpine et al, 2005, pp.496-9). Support of administration determines capacity that nurses could deliver the nursing role of patient advocacy. This implies, organizational structure provides foundation for autonomous property of the nurses (cf. Carole, 2008, pp.64-5). The hospital directorate powers influence capacity and development of structures for communicating patient concerns, consultation on patient treatment options and sustainability of nurses to provide education.
Thus, organizational structure influences nurse’s capacity to comply with principle of privacy, dignity and confidentiality (John, 2004, p.22). The authority of administration and alignment of administration to nursing principles of practice determines nurse’s capacity to clinical autonomy and capability of the nurses to build synergies and cohesiveness that is vital in sustainability of protection of patients (Jasper, 2003, pp.33-5).
The job security and provision of staff motivation determines nurse’s capacity to autonomy (John & Freshwater, 2005, p.19; p.36). Therefore the nursing work environments should provide psychological contract that nurses require to feel the health facility is committed to their cause (cf. ANA, 2004, p.7). The healthcare facility should demonstrate nurse ownership; an element that motivates nurses to be autonomous. The organizational climate that fosters nurse autonomous character should demonstrate positive nurse physician relationship (Foley et al, 2002, p.184). There should not be power distance between the physician and the nurses which could result into inability of the nurses to question care plan and care management of a patient.
Power distance and restricted communication does not provide opportunity for nurses to demonstrate control over their work. This negatively affects nurse’s capacity to deliver their roles of duty of care (Pearcey & Elliot, 2004, pp.283-5). Conformity to nursing principle of nursing has been identified as an ingredient for nurses to demonstrate autonomy and act to the best interests of the patients. Perceived level of nurse autonomy is a measure of patient advocacy and level of education that parents and patients get from the hospital (Donaldson & Carter, 2005, pp.356-7). Development of professional nursing practice environments determines capacity of nurses to engage in delivering care that conforms to principles of nursing practice (Driscoll & The, 2001, pp.99-101).
Nurse autonomy forms basis for continuity of patient supporting nursing environment (ANA, 2003, p.6). Nurses demonstrate capacity to provide nursing care that conforms to nursing principles of practice subject to availability of autonomy. Nurses play the role of patient advocacy if the nurses are free to make independent decisions on patient management and other members of staff respect their decisions (Fairley, 2005, pp.141-4).
Based on nursing practice, nurses consider autonomy as provision and recognition of nurse specialized and knowledge in nursing, identification of nurses values in advocating for patient rights and recognition of nurses to make reliable contribution to patient care (Street, 2009, p.6; pp.22-4). Therefore deficiencies in provision of nurse’s autonomy definition, contributes into reluctance of nursing to comply with nursing principles of practice. The nursing profession should be able to provide policies that increase nurse’s authority to mediate on patient behalf, address issues that affect patient safety and increase responsibilities of nurses through capacity of nurses to autonomous decision making (cf. Clouder & Sellars, 2004, pp.264-5).
The autonomy element in nursing has been negatively affected by failure to have nursing scope of practice (Somerville & Keeling, 2004, pp.43-4). The inadequacies of scope of nursing practice have resulted into failure of recognition of nurse’s specialized knowledge and expertise (Jasper, 2003, p.30). The nursing profession has been impacted negatively by failure to distinguish various roles and responsibilities of nurses (Smith & Jack, 2005, pp.42-5).
As a result, satisfaction of patient needs has been hampered by failures to provide framework for autonomy and lack of competent examination of nursing practice processes and mechanism they conform to duty of care (Skinner, 2005, pp.40-1; pp.59-62). Due to interference of different principles of nursing practice, there has been discontinuity in the flow of patient care that has negatively impacted on patient clinical outcomes. This demands critical assessment and evaluation of roles of nurse’s autonomy and mechanism it compares to patient care outcomes (Kolb et al, 2005, pp.195-9).
Patient management and care strategy development should conform to John’s model of reflection. The model of reflection has capacity to enhance nurses learning and development (Clifton et al, 2006, p.21; p.46). Through reflection on patient care and significance of patient management approaches, it would be possible o identify conflict of interests between patient autonomy, nurses roles as patient advocate and influence of parents or guardians in patient treatment options (Chabeli & Muller, 2004b, pp.38-42). John’s model of nursing reflection provides basis for nurses to visualize context of duty of care, sustainability of care and treatment options and promotion of health practice. Provision of autonomy provides a learning environment for nurses which translate into increased health promotion of the nurses (Taylor, 2006, p.124).
Reflection on nursing practice ought to contribute into health promotion of a patient through structural change on autonomy, development of health education that meets autonomy standards and promotion of interaction levels in nursing (Pearcey & Elliot, 2004, pp.283-4). Patient nurse interaction should result into better health outcomes for instance promote holism through spirituality care practices, enhance equity and patient participation in care, promote collaboration between patient parents, nurses and physician and provide necessary support from different stakeholders who have interest in health industry (Carol, 2008, pp.61-3).
The nurses could only play advocacy if empowerment is a function of care delivery. This could result into a scenario where nurses have control over decisions and actions that affect the patient that nurses care. Empowerment contributes into facilitation of nurse personal career growth and nurtures nurse’s commitment to duty of care (Bray & Nettlton, 2007; pp.849-50). Patient empowerment should form basis for nursing health promotion through accounting to nursing principles of practice and standards that could contribute into increased health care outcomes (Allin & Turnock, 2007c, pp.114-5).
Oncology nursing should be a function of holistic approaches to patient management (Bolton, 2010, pp.66-7). Oncology care should demonstrate patient’s compassionate care, patient concerns and respect for patient autonomy. Oncology nurse should represent patients that cannot express their treatment preferences based on the patient clinical conditions. Different nursing practice of principles doesn’t provide foundation for autonomy and capacity for a nurse to represent best interests of a patient (Foley et al, 2002, p.184). As a result, nurse’s attitudes in autonomy determine quality of life and quality of care at the end of life of a patient.
Nurse attitude impacts on all phases of a disease progression. It is responsibility of a nurse to provide education of disease management and sustainability of treatment option. The autonomy therefore plays an important role in determining nurse’s provision of education to patient or family members (Barr, 2007b, pp.23-5). Autonomy impacts on cancer nurses to advocate for patient treatment options based on diagnosis and cancer prognosis. Thus, failure to institute autonomy decreases capability of nurses to reflect on patient experiences, modality of care administered and sustainability of decisions on patient with regard to contribution to positive health outcomes (Baxter, 2007, pp.104-6).
Oncology nurse reflection is a derivative of metacognitive strategies (Turnock & Mulholland, 2007, p.10) that contribute into determination of patient experiences, validity and reliability of decisions made and actions that are taken towards improving health outcomes. Reflection as part of palliative care results into identification of solutions and feasibility of solutions towards resolving patient issues that impact on autonomy, consent to treatment options and alignment of the decisions or actions taken to principle of beneficence (Ghale & Lillyman, 2007, pp.12-4).
As a result, reflection on experiences conforms to experiential learning models that contribute into constructivists values that could add value to patient health outcomes. The process of reflection has been identified to involve active exploration of patient experiences in order to gain insights into new methodologies of managing patient health outcomes (Donaldson & Carter, 2005, pp.383-5). The exploration nature of reflection relies on use of exploratory theory where emergence of new practices for patient management could be proposed from patient experiences (Barr, 2007a, p.29). Patient experience exploration helps to determine patient emerging preferences for care at en of life.
Exploration of experiences provides environment for determination of barriers to provision of appropriate care at end of life and predisposing factor for instance autonomy (Allin & Turnock, 2007a, p.58). It facilitates in determination of continuity or discontinuity of care at end of life hence form basis for improving care limiting factors in healthcare facilities. In many instances, patients care at end of life has been negatively impacted by system barriers with regard to discontinuity of care due to conflict of interest between nurse role as patient advocate and wishes of patient relatives fro alternative methods of treatment (Gustafsson & Fagerberg, 2004, p.276), nurses determination that patient’s relatives treatment option doesn’t contribute into positive health outcomes and influence of structure of healthcare at the end of life.
Oncology nurses that are not able to reflect on experiences don’t have enough knowledge on pain control (Smith & Jack, 2005, p.35). This contributes into poor patient management at end of life. Inadequate nurse experiences in patient exploration, results into under-prescription, insufficient nurse assessment of patient and increased possibilities of under medicating the patient (Young & Paterson, 207, pp.141-5). Incidents of poor bonding between nurse and patient have been identified to contribute into patients under reporting of pain which affects capacity to provide appropriate analgesia. This makes nurse reflection an important element in provision of nursing practice (Wopereis et al, 2010, pp.244).
The oncology nurses play an active role in patient pain management at end of life (Moeti et al, 2004, p.73). The nurses provide pain management strategies as well as patient management of physical and psychological clinical symptoms that could aggravate patient response to medical intervention. Therefore reflection on possibility of a treatment option to have positive outcomes or not should be based on trade off between providing peaceful patient transition and elevation of patient suffering (Fairley, 2005, p.145).
Reflection of patient experiences provides opportunity for nurses to develop care structures that could contribute into improvement of patient outcomes at end of life care (Barret et al, 2006, pp.76-8). Therefore the nurses ought to utilize current knowledge and nursing principles of practice in order to develop treatment options that could effectively reduce suffering of patient at end of life. There should be institution wide support for consultation amongst nurses and physicians towards use for treatment options that meet patient’s preferences. The oncology nurses should be used as benchmark for patient preferences and values for care (Bell & Morse, 2005, p.37).
There should be development of healthcare policies and models for improving nursing practice. There should be evaluation of legal and ethical issues that impact negatively on nurse’s capacity to deliver patient care and act as a patient advocate (Caroll, 2008, p.65).
The rule that nurses should implement doctor’s orders in providing care to patients is an evidence of low profile of nurses as patient advocates (ANA, 2004, p.7). This has contributed into nurse’s low profile power relations with physicians that has resulted into poor perception of nurses care recommendations for the patients. The outcomes of compliance with physician orders have negatively impacted on nurse’s autonomy. Adoption of universal nursing theory has failed to change nurse-physician relationship in terms of proposing best treatment of patient (Clark, 2006, pp.579-81).
Power as a driver for knowledge has contributed into physician recommendation for patient treatment modalities that put patients at risk. There is need to create awareness on nurse’s roles as patient advocates and acceptance of nursing experiences and skill development as capable of providing best interests for patients (NMC, 2004b, p.52). There is need towards development of policies that could shape the ideologies that governs healthcare systems and overshadows nursing culture. This could from basis for managing conflicts of interests with regard to autonomy (John, 1995a, p.228).
Reflection of nursing practice provides foundation for change of patient care, recognition of nurse autonomy principle and enhancement of attitudes that negatively affect nursing culture (Moeti et al, 2004, pp.75-9). Nurse reflection on patient management contributes into changes of patient management approaches and development of new guidelines and policies on patient care at end of life (Carole, 2008, p.65).
The reflection of patient experiences and interplay of autonomy contributes into determination of decision making capacity of nurse’s as patient advocates vis-à-vis the physician position on treatment options and the administration role in enhancing autonomy. Reflection on patient management provides foundation for identifying the contribution of organizational structure in determining effectiveness of care and capacity of nurses to meet patient needs at end of life (Kolb et al, 2005, pp.193-6).
Reflection of patient autonomy identifies nurse’s role as patient advocates. The foundation for patient care should be based on experiences and reflection (Gaines & Sanford-Ring, 2004, pp.2-3). Different nurse needs for patients that could enhance positive health outcomes are not provided for. In many instances, resources have been identified as an underlying cause. This depends on organizational culture and scope of regulations on economic use of medical resources. Reflection adoption as a method of nursing practice contributes into standards of evidence based research (Clifton et al, 2006, p.77). It results into capability to improve nursing practice, improve on patient care and meet expectations for filling the theory of nursing practice gap.
Capability to utilize evidence based research in order to develop framework of nursing is limited by nurse workload which decreases opportunities for a nurse to engage in reflection of a patient experiences (Clouder & Sellers, 2004, p.264). Lack of resources and lack of enough time due to nurse workload decreases opportunities for conducting evidence based research on nursing practice.
Methodology of the study
Introduction
This section reports on methodology of the study that was used to conduct studies on Kelly. It reports on rationale of reflection, study design and method of data analysis and data interpretation that was used.
Method of study
The case study was delivered through qualitative approach (Gilmoour et al, 2007, pp.37). The qualitative used mixed approaches like observational research and action based research techniques I order to collect the data and carry out data analysis. Observational research was used because it depends on first hand information on an event that was observed while in progress (Foley et al, 2002, p.184). The observational research was subject to expected events and their possible outcomes.
The study design
The study was designed to use phenomenology method of research (Driscoll & The, 2001, p. 98). Phenomenology as a method of research was used in order to help in providing foundation for reflection on the patient lived experiences (Cornish & Jones, 2007, pp.130-1), nurse role in intervention for the patient rights, physician role and parents role and mechanism interaction of the players in medical intervention impact on nurses capacity to discharge her duty of care (NES, 2007, pp.112-5).
The phenomenology was used to provide lived experience of patient health, how patient was managed, interplay of different nursing principles of practice and their conflicts and how the conflicts of nursing principle of practice took control of patient care management direction. Phenomenology was adopted to provide patient experiences subject to conflicts of nursing principles of practice on autonomy in healthcare systems (Chabeli & Muller, 2004, p.52).
The nursing practice lived experiences were adopted on basis of nursing profession relations, desires and expectations of different players that affect patient right to treatment and achievements and failures that were observed in nurse’s duty of care delivery (Bray & Nettlton, 2007, pp.851-4). Phenomenology made it possible to account for strategic language that influences connection between healthcare professional identity and its impacts on conformity to nursing principle of autonomy, nurse knowledge and experience and power to patient advocacy (Smith & Jack, 2005, p.34). The study was structured to utilize narrative analysis approach in order to determine impacts of discourse as a cultural resource that impacts on autonomy, mechanism it impacts essential elements of nursing discipline and conduct on autonomy (Leininger & McFarland, 2002, p.114).
Method of data collection
The data collection involved researcher’s active participation (Bolton, 2010, pp.34-9) by living with the study respondent and observing and documenting care that was given to the patient (cf. Clifton et al, 2006, pp.30-4). The patient data, physician discourse with patient father, roles of the researcher in intervention for the patient best interests and medical intervention data on patient were taken by using participant observation approach (Clouder & Sellars, 2004, pp.264-5). The outcomes of patient management based on recommendations from physician, patient father and nurses were transcribed into verbatim into a computer as text. The verbatim transcription were coded via verbatim codification, and categorized for analysis.
Data analysis
The process of data analysis initiated with order ranking of hierarchical observations (Moeti et al, 2004, p.74) based on nursing principle of practice that was violated and determination of intervention that ought to have been implemented based on autonomy. The judgments were then normalized qualitatively through creation and development of norms and precedence criteria on autonomy (Chabeli & Muller, 2004, p.54). The validity and reliability of the judgments were examined for consistency with nursing principles of practice and deficiencies in nursing principles of practice identified.
The data analysis involved abstraction and generalization of concepts, reflection on applicability and praxis (Fairley, 2005, p.144). Reflection on the data was implemented to achieve understanding on rationale of judgments for patient treatment modalities, achieve insights on applicability of nursing principles and realization of new body of knowledge subject to deficiencies in nursing principle of practice that had contributed into development of conflicts of interests that interfered with complying with autonomy (Peden-McAlpine et al, 2003, p.497). Data analysis involved researcher’s reflection in action and reflection on action.
Data analysis was achieved through three distinct steps (Chabeli & Muller, 2004, pp.54-6). The data description step involved researchers description of different narrations and instances of nursing practice on basis of actions taken, thoughts develops due to appropriateness or inappropriateness of action taken, feelings developed subject to conformity or violation of nursing principles of autonomy and practice, circumstances and intervention implemented, and characteristics of the situations on which the incidents were observed (Somerville & Keeling, 2004, p.43).
Description step was followed by reflection step where the researcher reflected on the experiences described and then comparative analysis were implemented in order to compared researchers personal perception on correctness of the actions taken, personal beliefs that emerged, new assumptions that had been made to arrive at the action taken and new knowledge development (Clouder & Sellers, 2004, pp. 264-5). The researcher reflected on standards of nursing practice, theories of nursing practice, different situations and how they could impact on satisfying or violating nursing principles of practice and intentions that resulted into the actions taken.
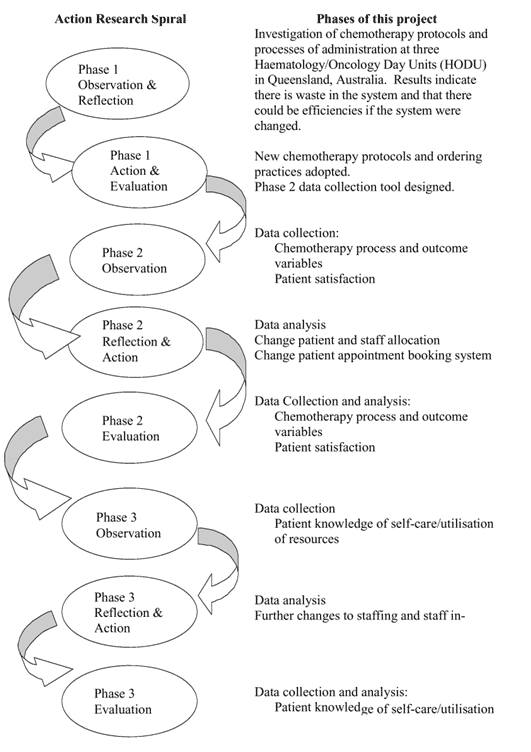
Reflective step formed basis for the action based research technique (figure 2) subject to utilization of three key elements namely scientific perspectives, ethical perspectives and aesthetic perspective of duty of care (TIP, 2006, pp.156-8). Reflective step was followed by critical step that is also termed as emanicipation step (Smith & Jack, 2005, pp.127-32) where the researcher corrected an action taken, critiqued application of a nursing principle of practice subject to its deficiencies or possibility of ineffective practices and mechanism through which the cause could be developed and assimilated into nursing practice.
Results and findings
Introduction
This section reports on the findings that were obtained after data collection. The findings demonstrate mechanism through which autonomy contributes into failure of nurses to deliver patient advocacy and how it influences outcomes of other nursing principles of practice
Failures in nursing principles
The case of Faizal ALL demonstrates failure of application of principles of nursing practice with regard to roles of the nurse as a patient advocate. The Faizal case presented lack of coordination ability of a nurse as a patient advocate through failure of physician to liaison with other nurses towards development of a treatment option for Faizal at his end of life care. There should have coordination of the physician, the Faizal Father and the nurses in implementing a treatment option that could have demonstrated best interests for the Faizal at his end of life. The case shows that Faizal as a terminal patient was not protected by nurses or physician.
Although the physician had arguments with Faizal father on possibility of another chemotherapy, the physician failed to adhere comply with nursing principles that demand independence of a nurse on treatment and management of a patient. Failure to demonstrate independence of nursing decision making in the interests of the patient demonstrated that the safety of the patient was put at risk. The nurses understood that the second chemotherapy could not have had any positive outcomes on Faizal survival. The continuity to provide another chemotherapy to Faizal shown lack of independence of nurses in instituting and implementing best interests of the patient.
The nurses and the physician failed to teach the Faizal father on ALL related concepts. This means the nurses and the physician failed to demonstrate capacity to promote the Faizal wellbeing in every situation that required intervention. The nurses ought to have spoken on behalf of Faizal hence demonstrating capacity to advocating fro patient’s right to refuse a treatment. The nurse should have refused provision of the second chemotherapy and advised the father that in principle, Faizal required care at his end of life and not a chemotherapy that was not to have positive implications on his survival.
The physician erred in proposing use of a chemotherapy that was under trial. The chemotherapy that was under trail was not medically determined its negative impacts. There was no documented safety for the chemotherapy that was under trial. The nurses should not have consented on the use of the chemotherapy that was under trial. This demonstrated negligence towards patient protection from harm. It was against nursing principle of beneficence. The nurses therefore didn’t demonstrate duty of care by protecting the patient from harm or consenting to medical treatment that nursing outcomes were not documented.
Patient advocacy was not complied with. The Faizal case demonstrated need for improvement in teaching of nursing advocacy role on patients. The traditional methods where a nurse watches a nurse as the nurse delivers positive role models in patient advocacy and mechanism of standing up for patient treatment rights seemed not sufficient in the light of Faizal ALL. The Faizal case demonstrates lack of nurses’ experiences in delivering the role of patient advocate.
The Faizal case demonstrated requirement for security of professional grounds in terms of patient advocacy. The case didn’t demonstrate nursing capacity to prove and abide by values of end of life care. Patient advocacy as a nursing principle of practice seemed to have accounted for the Faizal wellbeing. There capacity to conform to nurse’s integral duty as advocates for patients demonstrated failures in ethical practices, failures in exercising professional conduct and failure to address Faizal personal issues that could have contributed into Faizal father education on ALL, and facilitate reasonable judgment on Faizal end of life care.
The Faizal case questioned rationale for nursing practice in restoring patient’s health and mechanism through which different principles of nursing practice interact towards alleviation of patients suffering. The nurses didn’t question the physician directive. The nurses implemented the physician recommendations. The nurse’s duty of care includes carrying out procedures as ordered by the doctor. It is also nurse’s duty to collaborate with the doctors in order to deliver patient care management. The two elements of carrying out procedures as ordered by doctor, and collaborating with doctor to deliver care, conflicts with nursing principle of advocacy.
The nurse ought to have demonstrated independence by failing to implement the physician directives and seeking the physician advice on the rationale of providing Faizal chemotherapy when there were no chances for improving health outcomes. Collaboration with the physician could have provided basis through which ethics of care, duty of care and principles of nursing could have been applied in making decision on Faizal chemotherapy. The outcome of the nurse-physician collaboration could have resulted into a better framework for managing Faizal at his end of life.
Principles of nursing and administration of treatment
As a result of failing to discuss the Faizal opportunity for survival post chemotherapy, the nurses failed to address Faizal concerns for protection based on principle of beneficence and non-malfeasance. The nurse should have voiced the Faizal preferred mode of treatment. The nurses therefore failed to use the opportunity to identify weaknesses in the principles of nursing practice, duty of care and how it relates to an environment where the patient guardian or parent demonstrate wishes for use of medical intervention that cannot improve survival rate of a patient, use of chemotherapy that is under trial and position of the nurse as a patient advocate subject to independence of decision making of a nurse.
The patient, the patient family members and physician, should depend on the nurse to get information on patient’s end of life care. This implies, although a nurse takes orders on patient management from the doctor or physician, there should be reciprocity of guidelines. The nurse should be able to provide her stance with regard to patient safety, protection and advocacy. The nurse ought to demonstrate capacity to detect and address issues that could affect the patient’s safety and or shorten patient life and prevent the patient from nay clinical procedures that could result into harm to patient ethical management.
The nurse should demonstrate adherence towards maintaining patient’s safety as a priority. Independence of a nurse’s opinion on patient management should guide nurse’s capability to achieve the standards for patient’s advocacy. The nurse ought to have interceded on behalf of the patient by refusing to implement the doctor’s orders to perform chemotherapy on Faizal.
The patient right to refuse treatment
Acceptance or refusal of treatment should be the principle role of a nurse. The nurse ought to stand by her choice of providing care and interceding for the patient. The patient advocacy is part of palliative care. It helps to form and foster close patient relationship with her patients. The nurse education role should stress and clarify nurse’s advocacy and authority to protect patient. However, in practice, patients’ rights and interest are violated. Such a scenario brings into the light the moral status of the patient autonomy and the ethical element of the obligation owed to patients by nurses.
The case of Faizal demonstrated lack of nurses’ independence in making decisions on patients. The trade off might have been influenced by failure to understand the differences between being a patient advocate and standards of principle of beneficence. If beneficence gets first priority, patient advocacy is negatively affected and vice versa. The case of Faizal presented conflicts between the mechanisms through which nurses should provide beneficent obligations owed to patients. The effectiveness of managing terminal patients remains in understanding patient rights. The onus rests on capacity to use patient rights to deliver patient management.
The case of Faizal presented a conflict of interests in the nurse delivery of her roles. The nurse ought to believe in patient’s rights. The belief contributes into nurse capacity to decision making on treatment modalities. The nurse ought to accept patient right to be informed on their medical conditions. The nurse ought to accept and abide by patient wishes despite nurses possible differences of opinion. These conflicts in application of nursing care impacted on negative outcomes of Faizal management at end of life.
The Faizal case demonstrated limitation of nurses in providing advocacy for patients. Advocacy ought to form central values of nursing practice. Nurses should demonstrate capacity to put patient’s safety into their roles. The case demonstrated patient’s rights are not complied with during treatment dispensation. The reluctance of nurses to raise opposition on Faizal chemotherapy demonstrates lack of nurse’s policies that protect nurses. This puts patient’s safety at risk. There should be a policy that protects nurses from victimization when they raise issues on patient’s safety with their superiors. The nurses could not satisfactory deliver their roles as patients advocates if they are not protected. This calls for ethical and legal obligations of nursing principles of practice and mechanism they protect nurses.
Nurse Deficiencies as patient advocates
The Faizal case demonstrated failures in the support structure of a nurse as a patient advocate. The nurses visualize nursing care provides patient advocacy to expected standards. The Faizal case however demonstrated that the timing of nurse intervention could be influenced by factors beyond the control of nurse to act as an advocate. The nurse capacity to represent the patient may be limited by lack of authority and power in applying principles for instance beneficence, non-malfeasance and autonomy.
The job function of a nurse limits her application as an advocate. As a result of failures in the principles of nursing practice, the nurse was not able to protect Faizal from painful suffering, the nurse could not have promoted and forged for the patient autonomy and best interests and could not have optimized on health and abilities of the patient. The nurse failed to provide prevention of Faizal suffering and deliver peaceful end of life death. This places nursing advocacy as a theoretical basis for patient nursing care and ethics that can be varied based on prevailing circumstances. As a result, the capacity of a nurse to demonstrate commitment to patient and family members’ interference with nursing procedures and standards is minimal.
The Faizal case determined parent’s wishes have greater priority than independence of nurses in making treatment choices that suited current medical conditions of the patient. As a result, the nurse’s education on disease management to parents or patient could have limited outcomes on treatment of the patient. The Faizal case demonstrated that autonomy rests with the parents who can demonstrate what they deem fit for their patient. This puts nurses’ role as advocacy for appropriateness of the treatment as a second consideration after exhaustion of the parent or guardian wishes.
The Faizal case demonstrated existence of conflict of interest between the interests of a patient, interests of a nurse and interests of a parent. The Faizal case demonstrated the duty of a nurse to protect patient information. Protection of patient information has advantage of ensuring the nurse can implement treatment options that are to the best interests of a patient. As a consequence of privacy of communication of patient treatment rationale, the nurses ought to abide and conform to local and national laws on nursing. The patient information ought to be protected. This implies that the patient information with respect to parents or family members should get second priority.
The nurse should have first priority as a patient advocate. The capacity to act as an educator to parents or guardian threatens application of principle of confidentiality. It is duty of a nurse to provide information to parents on children treatment and response to treatment.
It is duty of a nurse to ensure she demonstrates enough kindness that can grant parents access to their child at end of life. The disadvantage arises when the privileges that nurses offer to parents as part of nursing practice turn into hindrance to delivery of best care plan for managing a patient. This puts nurse’s provision of permission to be with patient at end of life and disclosure of information on treatment of a patient at crossroads. Would the nurse abandon the best interests of the patient or allow to be misled in the process of abiding by nursing principles of practice?
The Faizal case present a scenario where educators of nurses could not present exact application of nursing principles and precedence that should be used when putting nursing principle of care into practice. The Faizal case presents deficiencies in nurse advocacy roles in training as advocates for patients. The Faizal case demonstrated physician and nurses had different opinions on Faizal chemotherapy. This demonstrates possibilities of lack of uniformity in the rationale of providing advocacy. The case further provided limitations in patient advocacy as incapable of being applied in every type of contingency management framework.
Nursing advocacy is based on learning by example that involves watching a role model deliver patient advocacy. As a result, mistakes that are made by the role model are duplicated by the student nurse in her work settings. Thus, situations could present themselves that could set bad precedence for patient advocacy. The Faizal case management and level of patient advocacy delivered demonstrated that, although nurses advocate for capacity to reduce risks and disabilities, decisions of the nurses could contribute into decrease of quality of life of a patient.
The Faizal case highlighted lack of nurse’s alertness on mode of treatment or decisions that affect treatment of patients when the patients are not able to voice their concerns. The nurses failed to give voice towards patient best interests when it was needed most. The nurse failed to respond to “what Faizal could have wanted”, “what Faizal could have preferred” and “what could be the wishes and values of Faizal?”.
Lack of inquisitive into values, preferences and wants of Faizal contributed into lack of foundation for nurses’ role as advocate on the Faizal case. Therefore the nurse’s action failed to measure to definition of patient advocacy as “act or process that supports patient cause or patient proposal”. The nurse failed to understand every encounter in the clinical environment provides opportunity for a nurse to mediate on her patient. The principle of beneficence provides that a nurse could act in the best interests of the patient without asking patients preferences and values.
Nurses role as advocate for family and its influence in nursing practice
The role of the nurse as an advocate requires guidance of the family member into current medical development of the patient. The nurse could arrange for family members to be with their patient at their point of death. This could happen in perioperative environment. The act of allowing family members to be with patient at point of death constitutes patient’s advocacy. In such instances, the nurse respect for wishes of a family member constitutes patient or family member advocacy of a nurse. The challenge that nurse’s face in respecting family wishes lay in acceptance of Faizal father wishes when they knew Faizal was not likely to positively respond.
Should role of patient and family member’s advocacy include acceptance of family member wishes on type of medical intervention to be used? This conflicts with patient’s right to refuse treatment if the patient has capacity to make informed consent. It conflicts with nurse’s right to refuse medical treatment on her patient if the medical treatment doesn’t add value to the patient management. This resulted into need to determine the principle of nursing practice or rule of nursing practice and conduct of nurse on patient medical treatment with regard to what ought to get first priority? This results into nurses challenges when they deliver their roles as advocates for patients.
The nursing duty of care is a function of team work. The nurse is supposed to consult with other nurses. The case of Faizal resulted into incapacity of nurses to consult. The Faizal case was characterized by competing priorities that impacted on nurse’s capacity to act as a patient advocate and protect and enforce principle of beneficence. As a result, the nurse was not able to put patient’s safety as a first priority. The principle of non-malfeasance and principle of beneficence affirm requirement for a nurse to put patient interests first. The Faizal case didn’t present a scenario where patient priority was considered.
The nurse conducted chemotherapy with full knowledge on the outcome. The nursing principles of practice affirm a nurse ought to put best interests for her patient regardless of possible arguments with members of staff, regardless of seniority, or failure to agree on practice issues that may compromise patient care and safety. The nurse should abide by practice standards at any instance. The Faizal case was characterized by oversight on nursing standards of practice. The Faizal chemotherapy impacts were not considered as a form of violation of principle of beneficence.
The nurses’ role and relationship with principle of privacy, dignity and confidentiality
The Faizal case management contributed into conflict of interest on the principle of confidentiality. The patient development at end of life ought to be a confidential matter. The principle of confidentiality conflicts with the principle of informed consent and education of patient and members of family on rationale and modality of the treatment to be provided and basis of carrying out the treatment.
Patient illness ought to be private information hence requirement for a patient to give consent on dissemination of the information to third parties. Discussion of the patient information to the Faizal father without considering the possible outcomes of father’s understanding of the outcomes contributed into failure to provide for patient’s dignity. The case demonstrated lack of inter-relationship in nurse functionality with regard to patient privacy, dignity and degree of confidentiality.
The need for a nurse to exercise her duty of care as an advocate for the patient subject to demonstrating independence of thought were deemed as nurses personal goals. Similar deductions could be made on Faizal father who, after being informed on survival rate of Faizal still believed his son could respond to a second chemotherapy. The principle of patient dignity and privacy should have formed basis for nurse’s independence of end of life care for Faizal. The conflict of interests between personal goals of the Faizal father and the personal goals of the nurse and physician resulted into lack of nurse’s independence in decision making.
The nurse ought to have made decisions on Faizal based on information of Faizal. This implies, the nurse ought to be guided by understanding of patient medical conditions when deciding on appropriateness of patient intervention treatment. The role of nurse support to the family and patient resulted into painful loss of the Faizal when the nurse ought to have ensured Faizal transition was peaceful and a happy moment. This implies, in nurse’s efforts to take care of the patient, the nurse should demonstrate caring about the patient. The nurses did not ensure Faizal death was peaceful. This was breach of spirituality care as a form of holistic and palliative care that oncology and pediatric nurse are supposed to provide at end of life.
Conclusion
This section reports on whether the study achieved its objectives and makes recommendations for future patient management based on autonomy.
The study achieved its objectives. The study determined that conflicts of autonomy impact negatively on the nurse capacity to represent patient interests and implement patient advocacy roles. The nurse’s autonomy could not be used as a basis for nurses to make independent decisions concerning patient end of life care. The deficiencies of autonomy in giving nurses power and authority over patient’s interests contributed into Faizal Fathers control of Faizal end of life treatment. The autonomy of patient relative to make decision on treatment options for a patient should not be given first priority although patient relatives have right to decide care and upbringing of the patient.
The nursing principle of autonomy does not provide order of priority in treatment decisions of a patient at end of life. The nurses should be in a position to voice concerns of the patient independently. The study determined nurses are in practice supposed to implement physician orders. The process of implementing physician orders should be a result of consultation between the nurse and the physician on patient bests interests at end of life.
The nurse, though is considered as a patient advocate, the Faizal case demonstrated the authority of a nurse as a patient advocate is relative and is dependent variable. As a result, the nurse acts as a patient advocate in theory. The study findings determined that the nurse should be able to refuse treatment options if the treatment options don’t contribute into patient alleviation of suffering or if the treatment options don’t increase the patient’s chances of survival.
The study findings determined that nurses should be able to provide advice and education to patients and patient relatives. The nurse should stand on their position as mediators of the patient from harm hence conformity to principle of beneficence. The nurse should prevent any treatment that may harm the patient. Failures of a nurse to take active role as a patient advocate are brought about by lack of policies that protect nurse from being accused of professional misconduct or failure to conform to ethics or abide by nursing principles of practice.
Due to autonomy of implementing physician orders, nurses are exposed to a working environment where they implement treatment options that don’t add value to patient care management at the end of life. The Faizal case determined that deficiencies of nurse to demonstrate patient advocacy on correctness of a treatment at end of life contribute into failure of patients to have a peaceful transition.
In instances when the patient is not able to make informed consent on mode of treatment option to be used, the nurse should represent the patient interests. This should include nurse’s power to refuse treatment options that don’t contribute into positive outcomes.
The nurse should jointly agree with the patient relative on the treatment options feasibility to improve health outcomes. The onus for the treatment options should be vested on the nurse due to nurse higher informed opinion on the treatment health outcomes. The nurse should not accept patient to undergo untested treatment for instance chemotherapy that are under trial due to lack of documentation of safety status and health outcomes of the untested treatment option. The autonomy does not clearly demonstrate trade off between use of treatment options whose efficacy is known and documented against use of treatment options that are not tested and are not documented on health implications.
The Faizal case helped to determine nurses don’t apply nursing principle of practice. This requires dependent on organizational settings. Regardless of organizational policies, the nurses should voice patient interests.
Recommendations
There should be development of policies that could protect the nurse from her duty to deliver roles of patient advocacy. As a result, there is need for amendments of the nursing principles of practice to ensure autonomy is prioritized. There should be a limit in which a patient relative could exercise control of patient treatment options. The nurse should have authority to determine treatment that suits patient interests without interference from physician or the patient relative. This could provide motivation of nurse to perform her patient advocacy roles.
The study recommends autonomy and beneficence should be differentiated in delivery of care. The study proposes there should be consultation between physician and the nurses on best interest of a patient. The nurse should actively participate in patient end of life care by demonstrating capacity to provide patient advocacy. Clarity of roles of patient relatives should be documented. This could ease the work of a nurse in patient relative education.
References
Allin L and Turnock C (2007a) Assessing Student Performance in Work-Based Learning. Making Practice-Based Learning Work.
Allin L and Turnock C (2007b) Reflection On and In the Workplace. Making Practice-Based Learning Work.
Allin L and Turnock C (2007c) Working with others in the workplace. Making Practice Based Learning Work.
ANA (2003) Nursing’s Social Policy Statement, Second Edition, p. 6.
ANA (2004) Nursing: Scope and Standards of Practice, p. 7.
Anderson E, Manek N and Davidson A (2006) Evaluation of a model for maximizing interprofessional education in an acute hospital. Journal of Interprofessional Care 20(2) 182-194.
Barr H (2007a) Occasional paper 8. Piloting interprofessional education: four English case studies. London: Higher Education Academy.
Barr H (2007b) Occasional paper 9. Interprofessional education in the United Kingdom 1966 to 1997. London: Higher Education Academy.
Barr H, Freeth D, Hammick M, Koppel I and Reeves S (2006) Report: The evidence base and recommendation for interprofessional education in health and social care. Journal of Interprofessional Care 20(1) 75-78.
Baxter P (2007) The CCARE model of clinical supervision: Bridging the theory-practice gap. Nurse Education in Practice, Mar, 7(2): 103-111.
Bell, S; Morse, S (2005). “Delivering sustainability therapy in sustainable development projects”. Journal of Environmental Management 75 (1): 37.
Bolton G (2010) Reflective Practice, Writing and Professional Development (3rd edition), SAGE publications, California.
Bray L and Nettlton (2007) Assessor or mentor? Role confusion in professional education. Nurse Education Today, 27(8): 848-855.
Carole Willard (2008) The nurse’s role as patient advocate: obligation or imposition? Journal of Advanced Nursing, Volume 24, Issue 1, pages 60–66.
Chabeli M, Muller M. (2004) A model to facilitate reflective thinking in clinical nursing education.Curationis. 27(4):49-62.
Chabeli M, Muller M. (2004) Reflective thinking in clinical nursing education: a concept analysis. Curationis. 27(4):37-48.
Clark P (2006) What would a theory of interprofessional education look like? Some suggestions for developing a theoretical framework for teamwork training. Journal of Interprofessional Care 20(6) 577-589.
Clifton M, Dale C and Bradshaw C (2006) The Impact and effectiveness of interprofessional education in primary care: an RCN review. London: RCN.
Clouder L, Sellars J. (2004) Reflective practice and clinical supervision: an interprofessional perspective. J Adv Nurs. 46(3):262-9.
Cooper H and Spencer-Dawe E (2006) Involving service users in interprofessional education narrowing the gap between theory and practice. Journal of Interprofessional Care 20(6) 603-617.
Cornish J and Jones A (2007) Evaluation of moving and handling training for pre-registration nurses and its application to practice. Nurse Education in Practice, 7(3): 128-134.
Donaldson J and Carter D (2005) The value of role modelling: Perceptions of undergraduate and diploma nursing (adult) students. Nurse Education in Practice, 5(6): 353-359.
Driscoll, J & The B (2001) The potential of reflective practice to develop individual orthopaedic nurse practitioners and their practice. Journal of Orthopaedic Nursing 5, 95-103.
Fairley D. (2005) Discovering the nature of advanced nursing practice in high dependency care: a critical care nurse consultant’s experience.Intensive Crit Care Nurs. 21(3):140-8.
Fazey, Ioan; Fazey, John A.; Salisbury, Janet G.; Lindenmayer, David B.; Dovers, Steve (2006). “The nature and role of experiential knowledge for environmental conservation”. Environmental Conservation 33: 1.
Foley, B J; Minick, M P Kee, and C C (2002) How nurses learn advocacy, Journal of Nursing Scholarship 34 (2), 181-186.
Gaines, M E, and Sanford-Ring, S. (2004) Alchemy: Medical mediation at its best,” Focus on Patient Safety 7 (4), 1-3.
Ghale, T. And Lillyman, S. (2000) Efefctive clinical supervision: The role of reflection. Wiltshire: UK.
Ghaye, T. and Lilyman, S. (2007) effective clinical supervision: The role of reflection. (2nd ed.) Wiltshrie: UK.
Gilmoour J, Kopeikin A and Douché (2007) Student nurses as peer mentors: Collegiality in practice. Nurse Education in Practice 7: 36-43.
Glen S (2004) Interprofessional education: the evidence base influencing policy and policy makers. Nurse Education Today 24(3) 157-159.
Gustafsson C, Fagerberg I. (2004) Reflection, the way to professional development? J Clin Nurs. 13(3):271-80.
Hignett S (2005) Measuring the effectiveness of competency-based education and training programmes in changing the manual handling behaviour of healthcare staff. Research Report 315. London: Health and Safety Executive.
Hilliard C (2006) Using structured reflection on a critical incident to develop a professional portfolio. Nursing standard 21 (2) 35-40.
Jasper, M. (2003) Beginning reflective practice. Foundations in Nursing and health Care. Nelson Thomas Ltd, Cheltenham.
John, C. and Freshwater, D. (eds) (2004) transforming nursing through reflective practice. Blackwell: Oxford.
John, C. and Freshwater, D. (EDS). (2005) transforming nursing through reflective practice. (2nd ed.) Blackwell: Oxford.
Johns, C. (2004) Becoming a reflective practitioner. Blackwell: Oxford.
Kneafsey R and Haigh C (2007) Learning safe patient handling skills: Student nurse experiences of university and practice based education. Nurse Education Today 27(8): 832-839.
Kolb, Alice Y.; Kolb, David A. (2005). “Learning Styles and Learning Spaces: Enhancing Experiential Learning in Higher Education”. Academy of Management Learning & Education 4 (2): 193–212.
Leininger, M., & McFarland, M. (2002). Transcultural nursing: Concepts, theories, research, and practice (3rd ed.). New York: McGraw-Hill. 12(3):110-26.
Making Practice-Based Learning Work (MPBLW) (2006) Mentoring: A resource for those who facilitate placement learning. Oxford Brookes University: Oxford.
Mamede, S; Schmidt, HG (2004). “The structure of reflective practice in medicine”. Medical education 38 (12): 1302–8.
Midgely K (2006) Pre-registration student nurses perception of the hospital-learning environment during clinical placements. Nurse Education Today 26(4): 338-345.
Moeti MR, van Niekerk SE, van Velden CE. (2004) Perceptions of the clinical competence of newly registered nurses in the North West province.Curationis. 27(3):72-84.
NES (2007) National Approach to Mentorship Preparation for Nurses and Midwives. Core Curriculum Framework. Edinburgh: NES.
NMC (2004a) Standards of proficiency for pre-registration midwifery education. London: Nursing & Midwifery Council.
NMC (2004b) Standards of Proficiency for Pre-registration Nursing Education. London: Nursing & Midwifery Council.
NMC (2004c) The NMC code of professional conduct: standards for conduct, performance and ethics. London: Nursing & Midwifery Council.
NMC (2006) Standards to support learning and assessment in practice: NMC standards for mentors, practice teachers and teachers. London: NMC.
Pearcey P and Elliot B (2004) Student impressions of clinical nursing. Nurse Education Today 24(5): 382-387.
Peden-McAlpine C, Tomlinson PS, Forneris SG, Genck G, Meiers SJ. (2005) Evaluation of a reflective practice intervention to enhance family care.J Adv Nurs. 49(5):494-501.
Skinner K (2005) Continuing professional development work for the Social Services workforce in Scotland. Dundee: Scottish Institute for Excellence in Social Work Education.
Smith A, Jack K. (2005) Reflective practice: a meaningful task for students. Nurs Stand. 19(26):33-7.
Somerville D, Keeling J. (2004) A practical approach to promote reflective practice within nursing. Nurs Times. 100(12):42-5.
Street, A. (2009) From image to action: reflection in nursing practice. DEakin University: Geelong.
Taylor B. J. (2006) Reflective Practice A guide for Nurses and Midwives 2nd Ed Berkshire: Open University Press.
Theory Into Practice (TIP) (2006) Explorations in Learning & Instruction: The Theory Into Practice Database. Greg Kearsley.
Turnock C and Mulholland J (2007) Learning in the Workplace: A toolkit for placement tutors, supervisors, mentors and facilitators. Chichester: Kingsham Press.
Walkerden, G. (2005) Felt knowing: a foundation for Local Government Practice. In Keen, M., Brown, V. & Dyball, R. (Eds.) Social Learning in Environmental Management. London, Earthscan
Wopereis, Iwan; Sloep, Peter; Poortman, Sybilla (2010). “Weblogs as instruments for reflection on action in teacher education”. Interactive Learning Environments 18: 245.
Young L and Paterson B (2007) Teaching Nursing: Developing a Student-Centered Learning Environment. Philidelphia: Lippincott, Williams & Wilkins.