Introduction
Since the 1980s, multiple interventions have been developed to treat the symptoms of posttraumatic stress disorder and Acute Stress Disorder (ASD) (Vanyo, Sorge, Chen, & Lakoff, 2017). Some of the most common ones include crisis interventions and critical incident stress management (CISM) (Hararay, 2012). Generically, these interventions are referred as components of the “debriefing” process, which is meant to address the immediate psychological effects of trauma among health workers (Halpern, Gurevich, Schwartz, & Brazeau, 2009). The CISM method is the most popular technique for treating the psychological effects of trauma because it provides support to victims through group contact (Macnab et al., 1999).
Its goal is to help people address the negative impact of stress before it has a long-lasting psychological effect on mental health and, by extension, the quality of healthcare services. The current debate on intervention use in PTSD management has been focused on understanding the merits of employing PTSD management interventions on the general application vis-à-vis the cautious application of the same methods on unique groups of people likely to suffer the greatest effects (Halpern et al., 2009; Macnab, Russell, Reverend, & Gagnon, 1999).
Most interventions developed to manage PTSD symptoms among EMH personnel are generalised, regardless of the unique work environment they are in. In other words, there have been minimal attempts made to identify unique working conditions and coping requirements for this group of workers. Furthermore, different interventions have unique characteristics and components that affect their efficacy in the treatment of PTSD symptoms among EMH workers (Halpern et al., 2009; Hararay, 2012).
Differences in the categorisation and application of interventions have further worsened the problem. Consequently, there is a challenge in the identification of appropriate interventions for the management of PTSD symptoms among EMH workers. The issue is further complicated by the existence of a wide variation of interventions for treating PTSD symptoms.
Apart from the time taken to implement the aforementioned interventions, they also demand a lot of commitment from healthcare administrators to address distressing aspects of the work experiences of EMH personnel (Halpern et al., 2009; Macnab et al., 1999). The impetus for identifying the right interventions to manage PTSD symptoms among EMH workers is rooted in the need to improve their cost-effectiveness and service planning outcomes (Vanyo et al., 2017).
The interventions are also meant to confront the emotional cost of PTSD among EMH workers. This systematic review builds on the above-mentioned views by providing a focused analysis of interventions aimed at reducing the effects of PTSD in the provision of emergency medical services. Its findings will be useful in developing or improving interventions that reduce the effects of PTSD and enhance the quality of services offered in emergency medical services. The following research aim and objectives guided this review:
Aim
This systematic review aims to identify literature relating to interventions for reducing ASD and posttraumatic stress disorder among emergency medical service personnel. The analysis will help to identify effective interventions that are suited for different groups of people and conditions.
Objectives
This review aims to identify interventions that could be used to treat PTSD among emergency care workers. The following objectives guided the investigation:
- What interventions have been demonstrated to be effective in treating PTSS (ASD and/or PTSD) among EMS workers?
- Is there a relationship between the symptoms and effectiveness/outcomes of the intervention? And does the duration of the symptoms affect the intervention outcomes?
- What external factors influence the effectiveness of PTSS interventions?
Methods
Inclusion and Exclusion Criteria
The inclusion and exclusion criteria used in this study involved a description of different parameters for removing or including studies for the review. Indeed, the guidelines for including or excluding studies for review were based on population, interventions and outcomes. These parameters are further discussed below.
Population
The target population for this review included EMS personnel of any age. Notably, research studies that included employees who worked as front line staff in the EMS or ambulatory services were given priority for selection. Comparatively, studies that used paramedics, or interns, as key study populations, were excluded from the investigation. Moreover, investigations that used “other” groups of emergency first respondents, such as fire-fighters and policemen, were excluded from the study. However, an exception was made to include studies that sought the views of fire-fighter paramedics because these professionals form a significant part of the early response medical team in most jurisdictions. Lastly, an exception was made to include studies that focused on a general overview of emergency responders’ views, provided they recognised EMH personnel as a distinct group of medical staff.
Interventions
Emphasis was made to include studies that highlighted interventions to minimise PTSD symptoms. Most of the research articles that met this inclusion criterion were clinical interventions. Clinical incident stress debriefings also formed a significant percentage of such journals, as was the case with those that shared a link with clinical stress debriefing processes. To create a reliable list of articles for review, those that contained ambiguities regarding the treatment of PTSD symptoms were identified and the authors contacted for clarification. Similarly, documents that involved the prevention of PTSD symptoms were also included in the investigation.
Outcomes
The desired clinical outcome for the articles reviewed in this document was the reduction of PTSD symptoms among healthcare workers. This goal is verifiable by conducting a self-administered questionnaire or by collecting data through observation because these were the main methodologies adopted by the authors of the studies sampled. Similarly, the outcomes (level of PTSD symptom minimisation) were measured using the Post Traumatic Symptom Scale and the Clinician-Administered Posttraumatic Stress Disorder Scale. A desired secondary outcome of the intervention would be a reduction in the duration of time for PTSD symptoms to manifest.
Types of Studies Included
This review included an investigation of all empirical studies that focused on the reduction of PTSD symptoms among healthcare workers. The search strategy yielded both published and unpublished data. The source materials used human subjects and were published in English. They were obtained from the following databases: Ovid PsycINFO, Ovid MEDLINE, Ovid EMBASE, EBSCOhost CINAHL, Web of Science and Google Scholar.
There was no limitation on the date of publication for the journals sampled. However, the reference lists attached to them were investigated for further analysis and verification of data. The keywords used to gather the research materials included: paramedic’, ‘emergency medical services’, ‘EMS’, ‘ambulance’, ‘emergency medical technician’, ‘EMT’, ‘prehospital’, ‘pre-hospital’, ‘acute stress’, ‘critical incident stress’, ‘posttraumatic stress’, ‘post-traumatic stress’, ‘post-traumatic stress’, ‘PTSS’ and ‘PTSD’. Full copies of materials that met the above-mentioned search strategy were obtained.
Data Extraction
The data used for this review were extracted from the research materials obtained through the processes described above. The pieces of information obtained were further subjected to a more rigorous analytical process, which checked for the reliability and validity of data. The articles selected were also reviewed for duplication at this point of analysis. Those that remained were further screened to assess whether they met the inclusion criteria described above. Those that failed to meet the threshold for review were excluded from the analysis and a reason provided. Following this data extraction strategy, the final list of materials that were included in this review was developed through a consultative process that acknowledged the researcher and supervisors’ inputs.
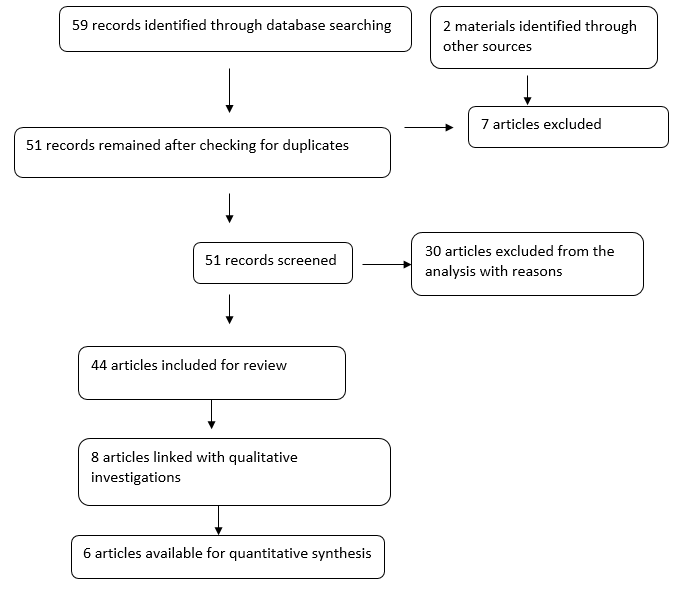
For quality assessment purposes, the data obtained in the review were assessed using the Critical Appraisal Skills Programme (CASP). Particularly, the technique was used to review the methodological quality of the studies sampled. Lastly, from the elaborate data analysis techniques adopted, different types of outcomes were expected from this analysis. To systematically analyse linked data, information was organised using the thematic data analysis method. The findings were developed using a combination of the inductive and deductive approaches. A meta-analysis was also done where appropriate. Figure 1 below outlines PRISMA.
PRISMA
Risk of Bias in Individual Studies
One of the main areas of bias for this systemic review is the data search process. This step was undertaken by the researcher alone; meaning that the processes could be subjected to prejudice. However, the data extraction stage was important in affirming the validity and reliability of the information obtained. Since this limitation was identified before starting the review process, emphasis was made to describe the search strategy in detail to enable other researchers to conduct a similar investigation.
The inclusion of English-based studies in this review also portends another limitation for this systemic analysis of PTSD interventions because associated studies that have investigated this research phenomenon were omitted from the review based on language limitations. The confinement of the search strategy to a few credible databases was also another limitation of the study because other sources of data could similarly contain relevant articles.
Results
The results obtained from this systematic review were categorised according to themes. Each one of them represented a specific intervention discussed by the authors sampled. Broadly, the interventions that emerged from the analysis were developed to improve coping strategies for stress among emergency care personnel. Six themes emerged from the review. They include critical incident stress evaluation, narrative therapy, downtime, early psychological interventions, e-Mental health approach and exposure-based cognitive behavioural therapy. The themes are further discussed in the sections below.
Critical Incident Stress Intervention
The critical incident stress debriefing (CISD) was highlighted as one of the most effective interventions for managing the stress and symptoms of PTSD. The doctoral dissertation by Hararay (2012) particularly highlighted its efficacy in the treatment of PTSD symptoms among emergency care workers in a district hospital. The findings were based on an empirical investigation involving five emergency care workers who suffered the adverse effects of trauma. The study highlighted the need to use seven guidelines for CISD training, which included an introduction, fact phase, thought phase, feeling phase, reaction phase, strategy phase and re-entry phase (Hararay, 2012).
The study confirmed that the CISD framework was an effective way of treating PTSD symptoms. However, the need for a more comprehensive review of the effects of cultural factors on the experiences of emergency personnel was recommended. The CISD was also mentioned by Hararay (2012) who said that it did not have a significant impact on the severity of PTSD symptoms but had a stronger effect on the efficacy of stress management strategies before the occurrence of trauma.
The article authored by Halpern et al. (2009) also evaluated the effects of critical incident stress intervention on the ability of 60 emergency medical technicians to cope with the adverse effects of PTSD. The authors established that there was a positive correlation between early exposure to stress and coping ability. The critical incident stress intervention was also proposed by Macnab, Sun and Lowe (2003) who used a three-level assessment of factors to understand the commencement of intervention strategies in PTSD management. Their study was closely linked with that of Macnab et al. (1999) that was published four years earlier. The empirical investigation gathered data from nurses, physicians and paramedics. These participants were the first responders to a crash site that had five fatalities (Macnab et al., 1999).
Using the Mitchell Model of emotional awareness, the researchers sought to find out the effects of critical incident stress interventions on the minimisation of PTSD symptoms across a two-year study. It was established that requests for critical incident stress interventions were lower than expected; meaning that ambulatory medical personnel chose other methods of coping with stress (Macnab et al., 1999). This study highlighted the possibility of there being too much emphasis on PTSD among emergency care personnel, while the need for such assistance is negligible. Its findings contradict what the other articles reviewed in this document showed because it suggests that the need for drastic interventions is overstated.
Narrative Therapy
A narrative therapy model was also identified as one of the most effective ways of treating PTSD symptoms. This intervention works in a binary manner where a subject is allowed to talk about past experiences and a therapist links them with positive future expectations of life. The technique was highlighted in the article authored by Palgi and Ben-Ezra (2010), which documented the treatment’s success in relieving PTSD symptoms for a soldier who worked in the Israeli army. The participant had experienced a traumatic event where he had to carry body parts of a dead terrorist across a dangerous border crossing point (Palgi & Ben-Ezra, 2010).
Consequently, he started manifesting symptoms of acute depressive disorder and a mild case of PTSD. Irregular sleep patterns, disassociation with current events and nightmares were some of the depressive symptoms manifested by the patient (Palgi & Ben-Ezra 2010). The narrative therapy method was successfully employed to manage the condition.
Broadly, the narrative therapy method does not use the past as the focus of therapy because neurotic links are established between its associated events and the future. The narrative therapy technique is closely linked with the identification and description of emotions method explained by Halpern, Maunder, Schwartz and Gurevich (2012). The researchers sampled the views of 190 paramedics who were exposed to traumatic events in the emergency care setting.
Their findings revealed that the ability to describe emotions was correlated with people’s coping mechanisms for trauma. Therefore, professionals who were able to correctly describe or convey their feelings were better equipped to cope with PTSD symptoms. Test results also showed that the inability to describe emotions was not associated with a reduction in PTSD symptoms (Halpern et al., 2012). Furthermore, the inability to correctly identify emotions was linked with a high level of negative symptoms for the target population. Broadly, this study revealed a link between a person’s ability to express their emotions and their perceived ability to cope with stress (Halpern et al., 2012).
Downtime
The need for rest after a traumatic event was also highlighted as an effective intervention for treating PTSD. Notably, the article by Halpern, Maunder, Schwartz and Gurevich (2014) highlighted this factor by identifying the need for workplace-based interventions to reduce the incidence of posttraumatic stress events on emergency care workers. The study sampled the views of 201 emergency medical practitioners and physicians who gave their views using a questionnaire (Halpern et al., 2014).
The respondents demonstrated that downtime was linked to low levels of depression and burnout symptoms. In fact out of a population of 75% of the personnel who took part in the study, 59% of them reported experiencing better symptom management for PTSD (Halpern et al., 2014). This outcome was associated with reduced levels of stress, burnouts and emotional upheavals. Nonetheless, low levels of depression were regarded as the most common outcomes for the intervention. Overall, it was established that critical incidents followed different pathways of neurologic processing and there was a need to identify one that suited the specific dynamics of the affected emergency personnel.
The above-mentioned view closely relates to the need for a cultural understanding of PTSD symptoms, which was highlighted by Macnab et al. (1999). The use of downtime to alleviate symptoms of PTSD was also mentioned by Vanyo et al. (2017) who interviewed 60 medical practitioners that reported having experienced a reduced intensity of PTSD symptoms by taking some time off work. Based on an ethnographic investigation of the views of emergency medical personnel regarding the alleviation of PTSD symptoms, the researchers also suggested that most emergency healthcare workers needed emotional support at work (Vanyo et al. 2017).
Therefore, interventions that addressed this need were recommended. The need for education regarding the effects of PTSD and its effects on workplace performance was also mentioned as another area of improvement in the study authored by Vanyo et al. (2017). However, it was reported that organisational cultures which stigmatised those who suffer emotional vulnerability posed the biggest barrier to accessing effective interventions.
Early Psychological Interventions
Early psychological interventions also emerged as another technique for managing the effects of PTSD. It works by identifying people who are at high risk of PTSD and providing them with the necessary support and tools needed to manage the effects of trauma. This technique has been linked with an increase in emotional stability among emergency personnel who have experienced the effects of PTSD.
The technique has also been regarded as one of the most effective methods for improving the effectiveness of long-lasting prognosis in PTSS management. These insights were highlighted in the article authored by Cunha, Soares-Oliveira and Pereira (2009), which investigated the efficacy of early psychological interventions in the treatment of PTSD symptoms among medical care workers. The editorial investigation also affirmed the need to expose workers to adverse events so that they develop better coping mechanisms.
Exposure-based Cognitive Behavioural Therapy
The article by Bryant et al. (2019) exemplified the efficacy of exposure-based cognitive behavioural therapy for medical personnel working in the emergency department. One hundred participants participated in the study and were randomised to five active treatment methods for PTSD using the exposure-based cognitive behavioural therapy. The interventions included educational seminars, skill-building sessions and simulated “imagined exposures” to improve coping methods (Bryant et al. 2019). The respondents’ reactions to the interventions were assessed during the baseline period and the analysis was done post-treatment and after six months.
The exposure-based cognitive behavioural therapy works by subjecting victims of PTSD to short or long-term imaginative exposures to trauma. The purpose is to reduce its effects on a patient by exposing him or her to its impact, albeit in small quantities. The same approach can be compared with the efficacy of vaccination where a small amount of the disease-causing factor is injected, or orally administered, into a person’s body and immunity is developed. This intervention was identified to cause marginal reductions in PTSD symptoms (Bryant et al. 2019). The outcomes were identified after reviewing the severity of PTSD for maladaptive behaviour and depressive symptoms using the Clinician-Administered PTSD Scale.
The pre-traumatic vaccination intervention was also examined as another method for treating people with PTSD symptoms (Essar, Palgi, Saar, & Ben-Ezra, 2010). However, it was explored as a pre-exposure intervention because of its reliability in managing symptoms before they occur.
Unlike other interventions proposed in this study, the exposure-based cognitive behavioural therapy was administered before the occurrence of the traumatic event. The goal of the intervention is to equip medical personnel with skills for coping with the effects of trauma. Therefore, even when exposed to it, they are better able to adjust to its effects compared to people who have not experienced any level of pre-exposure. This intervention was linked to low levels of disassociation between traumatised victims and the incident that caused the trauma in the first place. Therefore, victims were more aware of the effects of trauma on their lives compared to those who ignored them. The intervention was also associated with a lower level of mistakes and errors among medical personnel and an improved likelihood of leading a normal life (Essar et al., 2010).
Lastly, the use of drugs to treat the symptoms of PTSD also emerged in the investigation through discussions conducted by Murray, Wallace and Nielssen (2017). In their article, they focused on Rivastigmine (RVST) as a reliable drug for the minimisation of PTSD symptoms. The right dose for treating these symptoms was identified to be 12 mg orally or 13.3 mg transdermally for an adult (Murray et al., 2017).
e-Mental Health Approach
The use of online-based emotional support techniques also emerged from the review through an examination of the study authored by Ketelaar, Nieuwenhuijsen, Bolier, Smeets and Sluiter (2014), which used the pretest-posttest study design to evaluate the impact of e-Mental health on a group of 128 nurses working in an emergency care department in Netherlands. Self-help emergency medical health services were provided on this platform to this group of nurses who reported marginal levels of PTSD symptom reduction. Furthermore, significant improvements in work functions were observed and a diminished incidence of fatigue reported.
Based on the marginal reduction in stress-related symptoms observed in the studies, the researchers emphasised the need for improving virtual methods of providing emotional support to PTSD victims. The resilience of healthcare staff in coping with the negative effects of PTSD also emerged as another key area of discussion for some of the articles reviewed.
For example, the article by Ke et al. (2017) showed that women were more likely to demand interventions for managing PTSD symptoms compared to men because they suffered a disproportionately high psychological impact of adverse events compared to their male counterparts. The investigation was conducted in Taiwan and it explored the resilience of healthcare workers who took part in an emergency evacuation process for earthquake victims. Nonetheless, the resilience of healthcare staff was established after early intervention was introduced (Ke et al., 2017).
Discussion
Most of the studies sampled in this systemic review used the qualitative methodology because the alleviation of PTSD symptoms is largely subjective. Indeed, different groups of health workers may report varied emotional effects of exposure to a traumatic event. Nonetheless, the interventions described above aim to manage PTSD symptoms before, during and after they happen. For example, exposure-based cognitive behavioural therapy is designed to equip health workers with the tools needed to manage adverse events.
However, for most of the interventions analysed in this review, there was little evidence to support a high level of efficacy for the prevention of PTSD symptoms. However, there was enough data to support conclusions about six treatment methods, which have been described above: critical incident stress evaluation, narrative therapy, downtime, early psychological interventions, e-Mental health approach and exposure-based cognitive behavioural therapy.
It is important to emphasise three broad observations that emerged from the review. The first one is that the interventions mentioned do not necessarily reduce the incidence or severity of PTSD symptoms among emergency health workers. Secondly, from a meta-analysis of six research trials included in this study, it can be established that critical incident stress intervention is more effective in reducing PTSD symptoms compared to support-based therapies. Besides, collaborative care emerged as one of the most effective interventions for managing PTSD symptoms among EMH workers compared to individual-based therapies.
This finding emphasises the need to establish open channels of communication and support for emergency medical service workers that may be suffering from psychological problems because of PTSD. Another observation that emerged from the review related to gender differences because no significant variations in PTSD symptoms were observed in studies that had male and female respondents.
Anecdotal data regarding the role of a person’s history of depression in reducing the effects of PTSD was inconclusive. For example, it was difficult to understand the effects of timing, intensity of adverse events and drug dosages on the management of PTSD symptoms. Similarly, the evidence needed to determine whether specific interventions were appropriate for different types of trauma victims was also inconclusive.
Although the interventions mentioned in this review emerged from reliable and credible empirical research, the authors sampled made little effort to understand the efficacy of their interventions beyond their targeted participants. The use of drugs to treat PTSD symptoms was also rarely discussed in the literature studied, except for Rivastigmine drug, which has a broader use on patients beyond PTSD management. Therefore, this area of research lacks adequate scientific rigour to identify drugs that could be administered effectively to affected persons or improve their efficacy in the management of PTSD symptoms. Nonetheless, the broader context of this review suggests the potential for healthcare personnel to self-administer drugs to cope with the symptoms of PTSD. This stress management strategy may obscure some of the findings presented in the journals sampled because some of the respondents may not be forthcoming to disclose all pieces of information that may be self incriminating.
Broadly, it could be deduced that most of the interventions proposed for treating emergency care workers mentioned in this study aim to identify, understand or change the thinking patterns of personnel who suffer from PTSD. For example, the narrative therapy method emerges from this school of thought because it strives to link past experiences with positive future references. The cognitive behavioural therapy method is also modelled on the same basis of reasoning because it targets people’s thinking patterns for better stress management.
Exposure therapy also shares the same characteristics, except that it is focused on pre-empting the occurrence of PTSD by preparing health personnel to manage possible adverse experiences they may encounter at work. The pieces of evidence gathered in this study affirm that it has been positively used to reduce fear and anxiety among patients (Halpern et al., 2009; Macnab et al., 1999). Indeed, by being exposed to terrifying experiences, people become less sensitive to harm and can cope with their effects better than those who did not get the same exposure.
Summary
This review highlights a list of interventions for managing PTSD symptoms among emergency service workers. The multiplicity of journals and articles that discuss this research issue across varied sectors of the healthcare practice show that the topic is multidisciplinary. Based on this idea, most of the authors who have investigated the research topic do so from a western perspective. Indeed, most of the research articles originated from either the United States (US) or the United Kingdom (UK). However, there were a few exceptions where the analysis was based on selected Asian countries, such as Taiwan, but such reviews are scanty. Nonetheless, the selection of research materials was informed by the limitation of the search strategy to include only English-based studies.
Overall, the management of PTSD symptoms among emergency care workers is a practical issue and this is why the studies sampled in this analysis were based on case studies and empirical investigations. However, it is important to recognise limitations in applying the findings because some of them are unique to the demographics targeted. Lastly, in the course of undertaking this systematic review, a list of possibly interesting research questions emerged from the investigation. However, the time allocation for completing this assessment was pre-established and consequently, it was difficult to explore all new and emerging lines of research.
The information presented in this document could provide the impetus for undertaking future research on PTSD management. It is possible to do so because researchers can use similar platforms to address some of the challenges highlighted in this paper. For example, they should be able to replicate this work, partially or in full. However, the process should be done after acknowledging the limitations highlighted in this study. For example, the review of only English-based studies means that there is potential for reviewing more studies published in other languages. Lastly, there is room to expand the use of meta-analyses and systemic review findings in medical research because they are rarely utilised in PTSD research.
References
Bryant, R. A., Kenny, L., Rawson, N., Cahill, C., Joscelyne, A., Garber, B.,… Tockar, J. (2019). Efficacy of exposure-based cognitive behaviour therapy for post-traumatic stress disorder in emergency service personnel: A randomised clinical trial. Psychological Medicine, 49(9), 1565-1573.
Cunha, S., Soares-Oliveira, M., & Pereira, N. (2009). Early psychological intervention in prehospital emergency care systems. Journal of Emergency Medicine, 36(4), 404-6.
Essar, N., Palgi, Y., Saar, R., & Ben-Ezra, M. (2010). Pre-traumatic vaccination intervention: can dissociative symptoms be reduced? Prehospital and Disaster Medicine, 25(3), 278-84.
Halpern, J., Gurevich, M., Schwartz, B., & Brazeau, P. (2009). Interventions for critical incident stress in emergency medical services: A qualitative study. Stress and Health, 25(1), 139-149.
Halpern, J., Maunder, R. G., Schwartz, B., & Gurevich, M. (2012). Identifying, describing and expressing emotions after critical incidents in paramedics. Journal of Traumatic Stress, 25(1), 111-4.
Halpern, J., Maunder, R. G., Schwartz, B., & Gurevich, M. (2014). Downtime after critical incidents in emergency medical technicians/paramedics. BioMedical Research International, 2014(1), 1-7.
Hararay, S. (2012). CISD and crisis intervention: A qualitative study. Pleasant Hill, CA: John F. Kennedy University.
Ke, Y. T., Chen, H. C., Lin, C. H., Kuo, W. F., Peng, A. C., Hsu, C. C.,… Huang, C. (2017). Posttraumatic psychiatric disorders and resilience in healthcare providers following a disastrous earthquake: An interventional study in Taiwan. Biomed Research International, 2(7), 1-10.
Ketelaar, S. M., Nieuwenhuijsen, K., Bolier, L., Smeets, O., & Sluiter, J. K. (2014). Improving work functioning and mental health of health care employees using an e-mental health approach to workers’ health surveillance: Pretest posttest study. Safety and Health at Work, 5 (2014), 216-221.
Macnab, A., Russell, J. A., Reverend, J. P., & Gagnon, F. (1999). Critical incident stress intervention after loss of an air ambulance: Two-year follow up. Prehospital Disaster Medicine, 14(1), 8-12.
Macnab, A., Sun, C., & Lowe, J. (2003). Randomized, controlled trial of three levels of critical incident stress intervention. Prehospital and Disaster Medicine, 18(4), 367-71.
Murray, A., Wallace, D., & Nielssen, O. (2017). Rivastigmine for treatment resistant post traumatic stress disorder. The Australian and New Zealand Journal of Psychiatry, 51(9), 946-947.
Palgi, Y., & Ben-Ezra, M. (2010). Back to the future: Narrative treatment for post-traumatic, acute stress disorder in the case of paramedic Mr. G. Pragmatic Case Studies in Psychotherapy, 6(1), 1-26.
Vanyo, L., Sorge, R, Chen, A, & Lakoff, D. (2017). Posttraumatic stress disorder in emergency medicine residents. Annals of Emergency Medicine, 70(6), 898-903.