Problem Identification
While working as a skilled nurse at the Arizona Center for Specialized Treatment, I noted that the greatest risk in post-operation surgery is a decrease in mobility of the patient who is in the process of recovery. As a result of the reduced mobility, patients are exposed to the risk of frequent falls since they are confined in unfamiliar environments. Besides, the post-surgery recovery facility has varying medication regimens and treatments. In addition, some patients may feel that they are strong enough to ambulate. Thus, falls are more likely to occur and increase health care costs.
As opined by Dykes, Carroll, Hurley, Benoit, and Middleton (2011), “although there is a sense of urgency in hospitals to prevent falls to ‘do no harm and because Medicare will not reimburse hospitalization costs due to falling related injuries, patient falls remain a serious problem” (Dykes, Carroll, Hurley, Benoit, and Middleton 2011, par. 7) at health care facilities. As observed at the Arizona facility, it is necessary to introduce rules and changes within the facility to minimize frequent falls.
Desirable changes
Even though the Arizona facility has implemented numerous interventions to prevent injuries from falls, little effort has been carried out in terms of implementation. The current intervention mechanism has loopholes that implementers may take advantage of. Therefore, there is a need to introduce the aspects of patient contract, bed alarms, and hourly rounding within the intervention mechanism. The contract will be signed by the patient stating that he/she agrees not to transfer, ambulate, or go to the restroom without calling for assistance. This contract will be signed once the nurse feels that the patient is moderately independent. Whenever the contract is breached by the patient, a bed alarm, which is attached to the patient’s mattress/wheelchair, will automatically alert the staff if the patient attempts to get up without calling for assistance.
Aligning change to the organization
As opined by Marquis and Huston (2012), “planning is critically important to and precedes all other management functions. Without adequate planning, the management process fails since organizational needs and objectives cannot be met” (Marquis and Huston, 2012, p. 32). Therefore, it is important to align the proposed change to avoid frequent falls at the Arizona facility. For the proposed change to be successful, it is important to create clear and accurate documentation to communicate the proposal within the facility’s mission of quality services within the best interest of the patients. The procedure should be aligned to the mission of organizational learning through constant and continuous training about the requirements in the proposed change (McCarthy Adedokun, and Fairchild, 2014). Thus, the beds should be fitted with alarms.
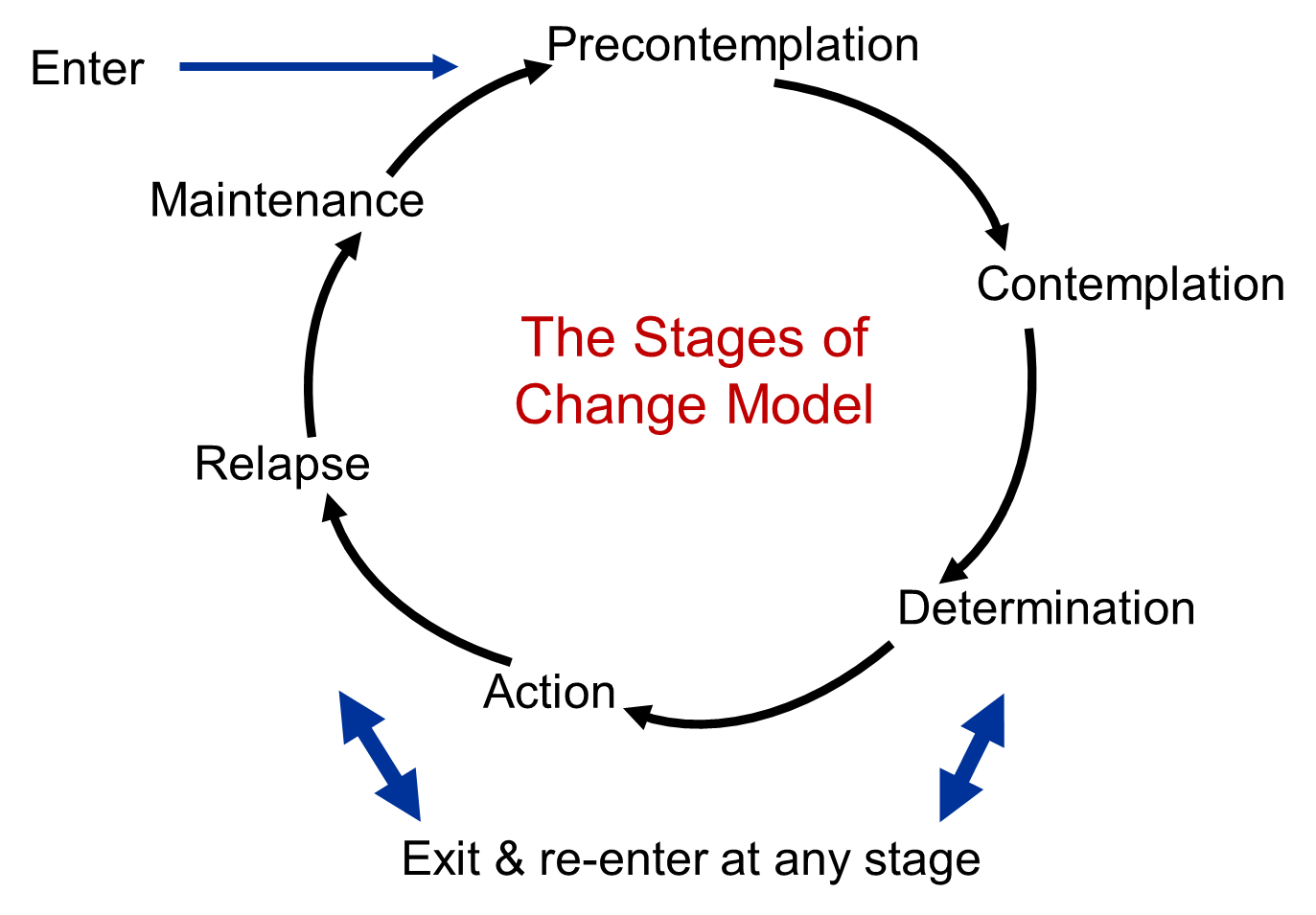
Change model and rationale
Frequent falls pose a great risk for nursing facilities as they reflect on the effectiveness of nursing care in a health facility. Therefore, the proposed change will create a safe nurse practicing environment to promote good and quality care for desirable patient outcomes. The proposed change is meant to prevent injury from falls. When a patient falls, their healthcare stay can be lengthened, causing the facility to incur additional costs because most insurance companies do not cover injuries that occur at a health care facility.
Steps in implementing the change
As indicated in the Lewin change theory, the steps in implementing the proposal to avoid and minimize frequent falls will involve research, documentation and training, implementation, and evaluation. Under the research, the change agent will carry out explicit analysis of best practices in other hospitals in order to create a flexible and sustainable change platform (Weick and Quinn, 2009).
The second stage will involve documentation and training. Under this step, the change agent will create legal contracts and other documentation to make the proposed change part of the treatment guideline in the post-surgery recovery environment. The stage is also characterized by creating a flexible training program for the nurses, who will be the main change implementers. The implementation stage will involve the actual process of testing and practicing the proposed change (Marquis and Huston, 2012). The last stage will involve evaluation of the effectiveness of the proposed change, in terms of reviewing the number of falls after implementation against the same number before implementation (Weick and Quinn, 2009). This is presented in the change model below.
Personal contribution towards managing the change
My roles include investigation to make sure all procedures are in place to prevent falls and patient education. Besides, I will have to speak with the assigned staff to have documents and progress notes completed (Marquis and Huston, 2012).
Skills necessary in facilitating change
The main skills required to implement the proposed change include project management skills, nursing evaluation skills, and intrinsic communication skills since the proposed change involves proactive participation and self-evaluation (Marquis and Huston, 2012). The success of the proposed change management plan will depend on the acceptance and the progress monitoring system. With the support of the shareholders, the proposed change aimed to minimize and avoid frequent falls within the post-surgery recovery environment will be implemented successfully (Bustin, 2004).
References
Bustin, G. (2004). Take charge: How leaders profit from change. Irving, Texas: Tapestry Press.
Dykes, P. C., Carroll, D. L., Hurley, A. C., Benoit, A., Middleton, B. (2011). Why do patients in acute care hospitals fall? Can falls be prevented? Web.
Marquis, B. L., & Huston, C. J. (2012). Leadership roles and management functions in nursing (7th ed.). Philadelphia, PA: Wolters Kluwer.
McCarthy, R., Adedokun, C. W., Fairchild, R. M. (2014). Preventing falls in the elderly long term care facilities. Web.
Weick, K. & Quinn, R. (2009). Organizational change and development. Annual Review Psychology, 50(2), 361-386.