Problem Statement
Budget cuts and decreased resources affected Sarah’s RN’s job at the hospital where she worked. Nurses, who comprise most healthcare workers, are particularly vulnerable to cost-cutting measures. Economic downturns can disrupt the nursing labor market, resulting in long-term shortages of qualified nurses. Nurse burnout and fatigue can be caused by various causes, including long working hours, rotational shifts, a heavy workload, and the emotional exhaustion of providing care and support for critically ill patients. Internationally, this is a significant issue for caregivers, whether they work in an Intensive Care Unit or an outpatient setting (Irani et al., 2018). Primarily, nurses should take care of themselves as emotionally and physically worn-out caregivers experience burnout and fatigue. No matter how many times a day a nurse fails to finish that final medical note, their emotional load grows heavier.
National Context
- Nursing burnout and exhaustion have been connected to a national quality indicator from the Joint Commission on Accreditation in Healthcare Organizations (JCAHO). This indicator points to healthcare organizations’ adherence to quality care standards that lead to their success.
- A nurse-sensitive quality indicator is linked to the problem of nurse burnout and fatigue. The availability of sufficient nursing staff is one of the key structural factors. Budget cuts at the hospital reduced resources and lessened personnel, increasing Sarah RN’s daily patient load from four to seven.
Background Information concerning the Problem
Nurses in emergency departments are more likely than other caregivers to experience burnout. Among the top concerns for improving the quality and safety in healthcare organizations is fatigue. In today’s healthcare system, nurses are the frontline caregivers who shoulder many jobs and obligations at a great personal expense (Dall’Ora et al., 2020). Having to balance multiple priorities in stressful situations might lead to feelings of exhaustion. Attributable to these stressors, healthcare professionals may not care for others properly.
Summary of Evidence-Based Article
Burnout results from a long-term misalignment between an individual and their work environment, an aspect of the job that should be addressed. When looking at how theories of burnout and other variables are linked, Dall’Ora et al. (2020) wanted to present a complete account that explores the correlations between nursing burnout and other variables and how this pertains to ideas of fatigue. MEDLINE, CINAHL, and PsycINFO were scoured for research that evaluated the relationship between nursing staff burnout and work-related factors, as well as quantitative primary empirical investigations. The researchers found ninety-one studies, the bulk of which were cross-sectional (n = 87). Among the factors, they found to be associated with burnout were a lack of control over one’s work environment, a lack of freedom to make decisions, a negative work environment, and a low level of social support.
Burnout has been linked to employee turnover, sick days, and overall health; however, only sickness absence and general fitness were associated with burnout. Insufficient nurse staffing, 12-hour shifts, time constraint, exhaustive job demands, poor variation in tasks, role conflict and decreased autonomy, negative nurse-physician interaction, and inadequate manager/leader support were all predictors of exhaustion in the medical literature. Because of burnout, the researchers discovered a decrease in job performance and a decline in the quality of treatment, a reduction in patient safety, adverse events, and an increase in patient dissatisfaction (Dall’Ora et al., 2020). These occurrences reveal that undesirable employment features, such as heavy workload, inadequate staffing, lengthy hours, and minimal control, are associated with nursing burnout. The consequences for caregivers and patients are appalling and should be resolved amicably to maintain nurses’ quality of care and work-life balance.
The Use of Information
The group used the information on nursing burnout and fatigue to enhance understanding of the problem and its effects on nurses and the quality of care. High job expectations and position uncertainty were among the most important psychological variables affecting the onset of exhaustion. However, healthcare workers reported higher degrees of fatigue than other working groups due to occupational burnout syndrome. Stress at work can lead to a condition known as burnout syndrome, which is a mental health condition (Irani et al., 2018). An individual’s ability to meet the demands of their employment is a symptom of this condition. Emotional weariness, depersonalization, and a reduction in self-esteem are all symptoms of occupational burnout. Overworked and overtired nurses face a host of problems, including a lack of knowledge about workplace regulations, a lack of managerial interest in their performance, a lack of courage, and a general dissatisfaction with their jobs. As a result, nurses forfeit their humane viewpoint on patient treatment and feel a sense of personal accomplishment diminished.
When healthcare provider experiences burnout, they may become emotionally depleted, distanced from patients, and less productive at work. These characteristics lower the likelihood of providing engaged and competent treatment to their patients. However, nurses suffering from burnout may be unable or unwilling to provide high-quality treatment because they work in poor quality of care. When nurses are dissatisfied with their working conditions, they are more likely to experience burnout, leading to a decrease in patient outcomes (Dall’Ora et al., 2020). Several adverse effects for patients and nurses have been related to nursing practice environments that lack support from the frontline and top management, low levels of human and other resources, and insufficient supplies for performance improvement and training programs. Inadequate staffing levels and unsatisfactory working conditions are closely linked to poor health outcomes and nurse burnout.
Decision-Making Model Diagram
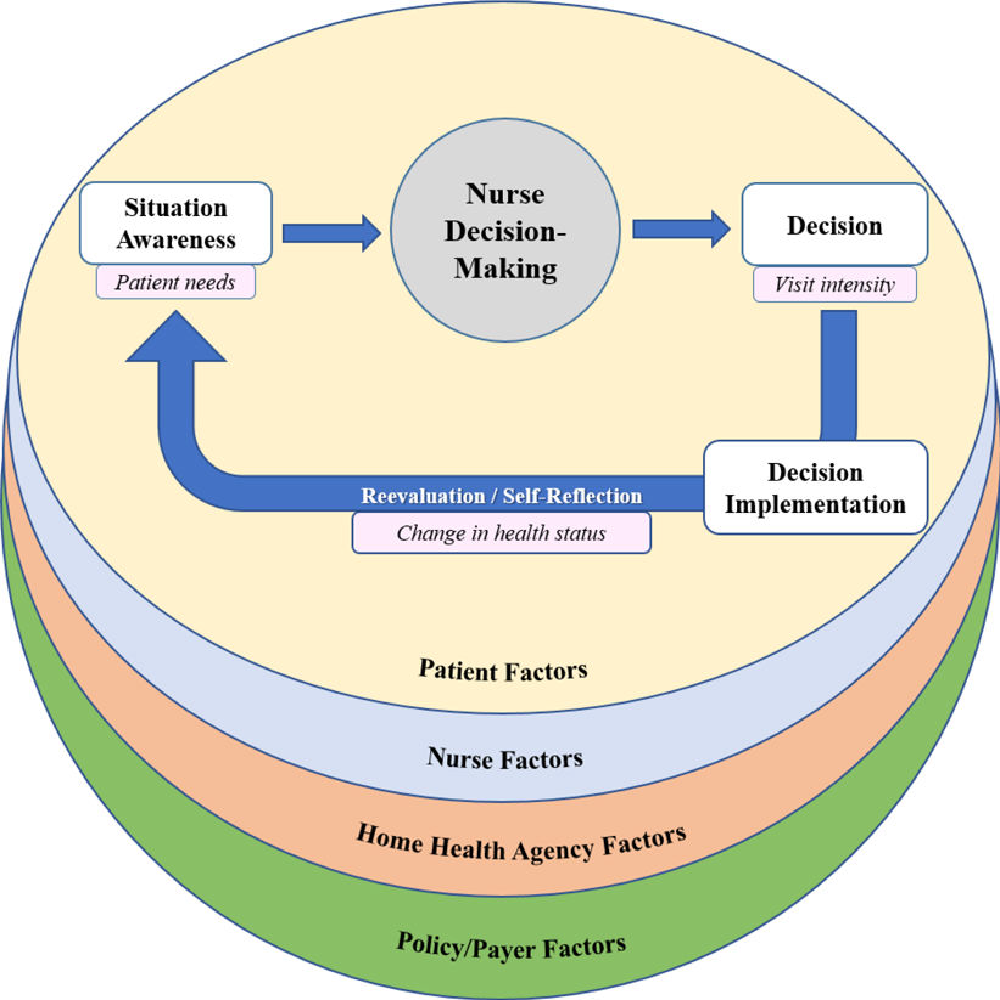
Knowing the patients and their families is critical to making the best clinical judgments. People’s values and professional expertise are essential considerations in decision-making, as are their previous encounters with similar situations. This allows for a more thorough assessment and comparison of available options. Managerial and peer support in a home health agency directly impact how nurses participate in decision-making and healthcare provision, which in turn influences effective policies (policy elements) and consequently affects care delivery.
Evidence-Based Practice Change
Efforts to reduce nurse burnout should include training healthcare leaders to detect and treat the problem and increasing nurse-to-patient ratios. Nurse leaders should detect, manage, and avoid burnout among their staff (Irani et al., 2018). They should be taught to recognize the indicators of disengaged employee or suffering burnout, such as a growing percentage of call-outs, withdrawal from interactions, and becoming upset with minor inconveniences during their training sessions. Early detection of indicators of burnout allows leaders to intervene and support their employees, preventing burnout from becoming a major problem.
Burnout is inversely proportional to the nurse-to-patient ratio. Emotional weariness is twice as familiar among nurses in healthcare facilities with 10:1 patient-to-nurse ratios compared to institutions with 5:1 balances. Burnout increases by 23% for every extra patient exceeding four that a nurse is assigned to care for (Irani et al., 2018). A higher staffing level may be required to reduce nurse-to-patient ratios. However, other issues can countered the cost, such as increased nurse turnover, patient dissatisfaction, and readmission levels.
Potential/Anticipated Outcomes
Nursing burnout may be exacerbated by close patient contact and complex practice environments, hurting organizational performance and quality of care. Notwithstanding the cultural, financial, and social shifts in healthcare systems, nurses worldwide face similar challenges. With the current nursing shortage and nurse burnout, providing safe and high-quality care can be challenging (Irani et al., 2018). Maintaining or improving the quality of care can be achieved through the development and testing of interventions to reduce nurses’ burnout and fatigue.
Researchers should investigate utilizing multidimensional scales and measurements to capture more characteristics of nursing care quality in the future, even though global assessments of the quality of care are convenient now. In addition, researchers depend on the quality-of-care reports provided by nurses, which have all the inherent biases and limitations. Instead of relying primarily on nurses’ reports for quality representation in future studies, it will be necessary to obtain patient outcomes data from multiple sources, such as discharge abstracts. However, it may be argued that a nurse-rated standard of care is better operationalized at the unit or hospital level than at the specific nursing level. A different approach for future research could be to use multilevel models to measure the quality of care at the unit or hospital level. Next, researchers should investigate if burnout directly affects patient care, for example, by causing errors or reducing the excellence of care provided.
References
Dall’Ora, C., Ball, J., Reinius, M., & Griffiths, P. (2020). Burnout in nursing: A theoretical review. Human Resources for Health, 18(1), 1-17.
Irani, E., Hirschman, K. B., Cacchione, P. Z., & Bowles, K. H. (2018). Home health nurse decision-making regarding visit intensity planning for newly admitted patients: A qualitative descriptive study. Home Health Care Services Quarterly, 37(3), 211-231.