Abstract
Sustainable management of medical waste is one of the major concerns that the Ministry of Health of Viet Nam and hospitals are trying to deal with. Most medical wastes are unique and cannot be disposed of in the same manner as normal wastes. They are infectious and can also cause serious physical injuries if they are not properly disposed of.
The paper looks at the current strategies used by public hospitals in Viet Nam to manage medical wastes. It discusses the strategies used at the local level (public hospitals) to ensure that medical wastes do not pose any significant threat to the public. Issues such as waste segregation at the hospitals and different ways of disposing of different types of wastes are explored.
The study also looks at the level of awareness among doctors and nurses on sustainable management of medical wastes, based on the assertion made in the literature that one of the only ways of achieving success in sustainable medical waste efforts is to ensure that all doctor and nurses are involved and are empowered to dispose of medical wastes responsibly. The study finally looks at what can be done to promote sustainable medical waste management in Viet Nam. It provides several recommendations that could be implemented at the hospital level and at the national level to enhance sustainable waste management.
Introduction
Background
The definition of sustainable development as “meeting the needs of the present without compromising the ability of future generations to meet their needs” was first put forth by Brundtland (1987) in the report ‘Our Common Future’. The report introduced the three fundamental components of sustainability as environment, economy and society and the need to balance the three of them in decision making, whilst also emphasising both intra-generational and inter-generational justice.
More recently, work around the planetary boundaries (Steffen et al. 2015) has reinforced the idea of environmental limits to growth, whilst the work of Raworth (2012) on “doughnut economics” has sought to reintegrate the importance of a ‘social floor’ to complement the concept of the ‘environmental ceiling’, aiming to generate both a “safe and just operating space for humanity.”
The pursuit of sustainable development is intimately connected to health issues. Much of the discussion has focused on the relationship between environmental pollution and public health. Early in the 1990s, Agenda 21 of the United Nations Conference on Environment and Development in Rio de Janeiro (UNCED 1992) defined reducing health risks from environmental pollution and hazards as one of the top concerns of the global community.
The Sustainable Development Commission (2010) emphasized the importance of “a focus on the environmental determinants of health and health inequalities, especially the effects of climate change”. More recently, health and well-being are perceived as integral to the achievement of Sustainable Development Goals launched in 2015, with Goal 3 explicitly aiming: to ensure healthy lives and promote the well-being for all at all ages.
There are multiple dimensions to the relationship between sustainable development and (public) health (Abdula, Qdais, & Rabi 2008). Besides the link between health and environmental quality, health care infrastructure itself has environmental impacts (Wilburn 2007). One could research carbon footprint, energy consumption, or water consumption of health care facilities, to name but a few areas (Abd El-Salam 2010).
This thesis focuses on one specific aspect: the current practices in the management of medical waste versus the required sustainable waste management paradigm. According to Pruss, Giroult, and Rushbrook (1999), poor medical waste management is linked with threats to the environment and human health.
Proper segregation, collection, storage treatment and disposal are important steps that take place at hospitals and under the scope of influence of health care workers (DARA 2010). Therefore, the daily practices of health care workers’ are important contributions to sustainable medical waste management and indeed to the sustainable development of a country’s health care system in general.
Much of the existing literature focuses on the medical waste management practices in the context of the developed world with a smaller number of articles exploring what sustainable medical waste management looks like in a developing country context (Ananth, Prashanthini, & Visvanathan 2010). This dissertation uses Viet Nam as the research context, based on a case study of the two major public hospitals, to identify the key actions for moving towards more sustainable medical waste management practice in the health care sector.
The purpose of this introductory chapter is to make the case for examining sustainable medical waste management in the Vietnamese health care context, with a specific focus on the role of healthcare workers, especially doctors and nurses.
Definition of Terms
Medical waste and classification
The terms ‘clinical waste’, ‘medical waste’, ‘hospital waste’ and ‘health care waste’ are often used interchangeably in both academic studies and a policy/regulatory context.
Clinical waste is defined broadly by Controlled Waste Regulations (2012) as “any waste which consists wholly or partly of human or animal, drugs or other pharmaceutical products, swabs or dressings, syringes, needles or other sharp instruments; and any other waste arising from medical, nursing, dental, veterinary, pharmaceutical or similar practice, investigation, treatment, care, teaching or research, or the collection of blood for transfusion, being waste which may cause infection to any person coming into contact with it”.
Therefore, clinical waste can be divided into three broad groups of materials: a) any healthcare waste which poses a risk of infection; b) certain healthcare wastes which pose a chemical hazard; c) medicines and medicinally-contaminated waste containing a pharmaceutically-active agent (Dutta & Das 2010).
The World Health Organization (WHO) (2014) defined ‘health care waste’ as all waste generated within health-care facilities, research centres and laboratories related to medical procedures. Between 75% and 90% of the waste produced by health-care facilities is non-hazardous or general health-care waste, and only 10% to 25% of health-care waste has a hazard that requires careful management (AQI 2015).
The distinct categories of health-care waste are sharps, infectious waste, pathological waste, pharmaceutical (including cytotoxic) waste, hazardous chemical waste, radioactive waste and non-hazardous general waste (EPA 2009). Infectious waste can be further classified as wastes contaminated with blood or other body fluids, cultures and stocks, and waste from isolation wards. Hazardous chemical waste includes halogenated and non-halogenated solvents, disinfectants, toxic metals such as mercury, and other organic and inorganic chemicals.”
Directive 43 of the Ministry of Health of Viet Nam (2007) defines ‘medical waste’ as ‘materials in solid, liquid or gaseous form, discharged from medical establishments, including hazardous medical wastes and ordinary/general medical wastes’.
Hazardous waste is waste that contains “elements hazardous to human health and environment such as contagiousness, intoxication, radiation, flammability, explosiveness, corrosiveness or other hazardous characters if these wastes are not safely destroyed”. This is the definition that will be used in this study. Medical wastes are classified into 5 groups: a) infectious wastes; b) hazardous chemical wastes; c) radioactive wastes; d) pressure container; e) general (ordinary) wastes.
Management of medical waste
The process of medical waste management in hospitals includes several interrelated steps: segregation, collection, storage, transportation, treatment and disposal (Pruss, Giroult, & Rushbrook,1999).
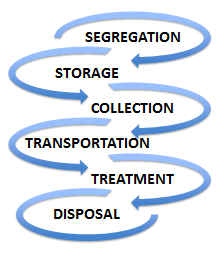
In these identified steps, segregation (to separate the waste into designated categories) is considered the most important step. Segregating potentially infectious material from clean waste at the point of generation may reduce both volume and cost (General Statistics Office of Viet Nam 2015). Improper segregation will lead to implications for public and environment health. Furthermore, infectious and hazardous wastes are subjected to special treatment (incineration, autoclave), which is very expensive before disposal. Autoclave, also known as steam sterilization, has been used for a long time in the medical sector.
Reduce, Reuse and Recycle
The 3Rs principle of reducing, recycling and recovery – also known as the ‘waste hierarchy’ – has been widely adopted since its articulation in 1995 (GFDRR 2011). The basic premise is that of reducing the amount of waste generated whenever and wherever possible. If a reduction is not practical, consideration should be given to re-use. Recovery is the final option if neither reduction nor reuse is practical (Jiang 2006). Currently, 3Rs has been accepted as Reduce, Reuse and Recycle.
Statement of the Problem
Viet Nam has experienced a dramatic increase in the amount of medical waste generated over the last 20 years, especially hazardous waste, due to the rise of complicated diseases in a growing population (International Conference on the Development of Biomedical Engineering 2015). When it comes to surveying Vietnamese medical waste collection, recycling, treatment and disposal, performance varies according to geography and type of healthcare facility.
Geographically, cities and urban centres with high populations tend to generate more wastes than rural and sparsely populated locations (Lye 2010). In terms of healthcare facilities, large referral hospitals tend to generate more medical wastes than small clinics, due to both handling more patients and also engaging in complex medical procedures that produce more wastes.
In terms of waste collection, according to the Ministry of Health of Viet Nam, in 2006, only 50 per cent of hospitals met the Ministry’s requirements around waste collection and segregation (Hoang 2009). According to a project by the Ministry of Health and the WHO (World Health Organization) in 2009 (MONRE 2011), it is estimated that more than 25% of medical waste can be recycled.
Most recycling activities, however, take place outside hospitals and under the management of contracted waste management companies. In 2003, a study by Cheremisinoff (2003) showed that only 5% of these wastes are recycled. The study attributes responsibility to various stakeholders, especially the government, for failing to come up with initiatives for recycling medical wastes.
In terms of waste treatment, current medical waste treatment facilities are not equipped with advanced technologies due to the limited state budget allocated. Whilst there is 71 per cent of public hospitals at the central level with wastewater treatment systems compared with 85 per cent in private hospitals, only 46 per cent have such facilities at the provincial level and 30 per cent at district level (Hoang 2009).
There is no single treatment or disposal method used for the various types of medical waste in Viet Nam (Kagonji & Manyele 2011). Common methods are incineration, landfilling, burning, autoclaving and chemical treatment (WHO 2014). Traditional waste treatment by incineration is still widely used for infectious medical waste. In Hanoi and Ho Chi Minh cities, hospitals have signed contracts with the third-party companies and medical waste is treated at centralized facilities using the incineration method (Hassan et al. 2008).
In other cities and provinces, hospitals are still using their incinerators. It is reported that the majority of hospital incinerators lack an air treatment system and the outdoor operating system also leads to environmental pollution (Hoang 2009). The Vietnamese Ministry of Natural Resources and the Environment (MONRE 2011) reported that only 50 per cent of the total incinerators in key cities are operating well, and as low as 20 per cent in other provinces.
Such issues have caused the Vietnamese MONRE to conclude that only 68 per cent of hazardous medical waste is properly treated, which presents a significant challenge for the goal of environment protection (MONRE 2011; p.92).
Furthermore, despite the efforts of the Government towards sustainable management of medical waste, multiple cases of poor handling, inappropriate treatment and disposal, and even waste being left completely untreated are still reported (Hutchins & White 2008). In 2015, a private hospital in Viet Nam was fined for illegally dumping 63 tons of untreated medical waste (Thanhnien NEWS 2015).
Recently, the largest and most prestigious public hospital in Viet Nam was blamed for wrong recycling activities of the hazardous waste, against the current regulations on medical waste management (Vietnamnet 2016). The Ministry of Health has come up with a legal and regulatory framework that guides how individual hospitals, both public and private, should manage their medical wastes.
Bolay, Hostettler, and Hazboun (2014), based on the study they conducted in Switzerland, say that the policies require hospitals to classify and segregate their wastes based on their impacts on the environment and ability to recycle them.
Bdour and Hadadin (2007), in their study conducted in Jordan, argue that policies also outline how hazardous medical wastes should be destroyed sustainably without posing any threat to the environment, people, plants, and animals. It is important to note that besides these government regulations, individual hospitals have their own internal medical waste management policies. However, their policies must conform to the policies set by the Ministry of Health.
Purpose of the Study
As the Literature Review will go on to explore, sustainable medical waste management involves, not only employing proper segregation, collection, transportation and disposal but also implementing the 3Rs of Reduce, Reuse and Recycle (Nihon 1999).
In a healthcare context, implementing ‘3Rs’ strategies needs to involve both the leadership provided by those in management positions and commitment to sustainable medical waste management amongst health care workers, especially doctors and nurses (Jiang 2006). This thesis argues that lack of such leadership and commitment could lead to increasing the amount of medical waste, non-compliant treatment, and therefore threats to the environment and public health.
Research Objectives and Questions
The following are the objectives of this study.
- To come up with effective sustainable waste management policies and practices that can be applied in Vietnamese hospitals
- To increase awareness among the stakeholders in the healthcare sector – specifically healthcare workers – on how to manage medical wastes using the 3Rs strategy.
- To achieve the above research objectives, the following questions were proposed to collect the relevant data.
What are the current strategies used by the healthcare institutions in Viet Nam in managing medical wastes?
- What is the level of awareness among the stakeholders – specifically healthcare workers – on sustainable management of medical wastes?
- What are the barriers to implementing 3Rs strategies and what can be done to promote sustainable medical waste management in Viet Nam?
Study Area
This research focused on two key public hospitals in two of the largest cities in Viet Nam based on population: one in Hanoi (in the North) and another in HoChiMinh city (in the South). Hanoi is the Vietnamese capital with a population of 7,096 million and HoChiMinh city has a population of 7,982 million, with the total population of the country as 90,700 million (General Statistics Office of Viet Nam 2015).

Significance of the Study
The recommendations from the study will be shared with those hospitals involved in the study, and the Ministry of Health of Viet Nam. It is hoped that the findings will enable the hospitals to address any identified gaps in daily practice in terms of implementing medical waste management policy. It is also hoped that, through examining the factors influencing the successful deployment of 3Rs strategy in other countries, this might be applied to the Vietnamese context to inform medical waste management, to contribute to the sustainable development of the country.
Literature Review
Sustainable medical waste management is an issue that has attracted the attention of many scholars and environmentalists who have conducted extensive research to find out the best approaches that can be used to manage different types of waste. The concept of sustainable medical waste management is becoming increasingly important in modern society.
As such, it has become necessary to develop better ways of managing these wastes (Blenkharn 2006). According to Sattler and Hall (2008), medical wastes are the most dangerous waste substances and if not disposed of properly, they may pose serious environmental problems. In Viet Nam, just like in many other countries around the world, medical wastes have increased significantly over the past three decades and managing these wastes is becoming an issue (Pariatamby & Tanaka 2013).
Substances such as syringe needles that were re-used after sterilization two decades ago are currently not re-usable because of fear of transfer of diseases such as Human Immunodeficiency Virus (HIV) (Birpinar, Bilgili, Erdogan 2009). The number of people seeking medical attention has also increased significantly due to the emergence of various lifestyle diseases (Ketlogetswe 2004). These are some of the reasons that have made it necessary for researchers to give serious attention to this topic.
As Visvanathan (2006) notes, for every research project, it is important to generate information that will enrich the existing bodies of knowledge. To ensure that the researcher does not duplicate the existing published information, the study first focused on a review of the literature before identifying key research questions and collecting the primary data. The review is important to understand what other scholars have found out in this topic and therefore identify potential research gaps that need further study.
Medical Waste Generation – A Geographical Overview
The health care industry is one of the largest producers of waste due to diagnostic, experimental activities and therapeutic methods (Diaz et al. 2008). As institutions that operate throughout the year, hospitals produce considerably large quantities of waste. The characteristics of medical waste are generally similar in all countries, but the amounts generated are different. This difference depends on variations in regulations and economic status between countries (Pruss, Giroult, &Rushbrook1999; Sakaguchi 2001).
Even within a country, generation of medical waste differs by geography, hospital level, and the departments in each hospital. It also depends on the types of health care service, the amount of disposable or reusable medical devices, and the regulations and policies governing medical waste management (Cesaro & Belgiorno 2015). For example, in a Vietnamese survey conducted in 24 hospitals, the intensive care unit, obstetric and surgical departments generated the largest amount of waste because of the nature of activities undertaken (Hoang 2009). The figure shown below is a comparison of medical waste generation from a global perspective.
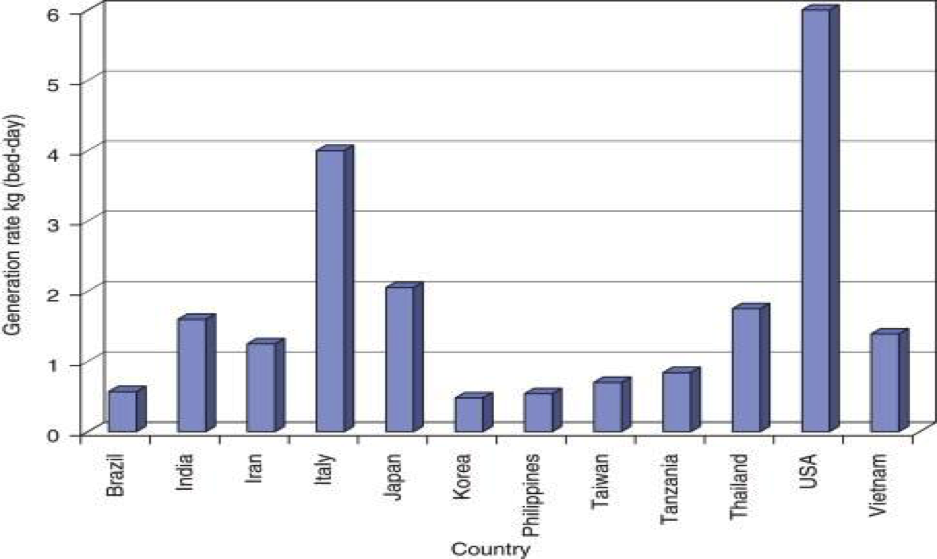
The information in the graph above shows that the developed countries produce the largest amount of medical wastes. The United States produces the highest amount of medical wastes in the world. As Sakaguchi (2001) notes, most Americans get regular medical check-up even in cases where they do not have a specific medical problem. Japan and Italy also produce significant amounts of medical wastes (Mbongwe, Mmereki, & Magashula 2008). China and India, because of the massive size of their population, also have a considerable amount of medical waste that need sustainable management.
The graph below provides further details in exploring medical waste generation in a section of Asian countries.
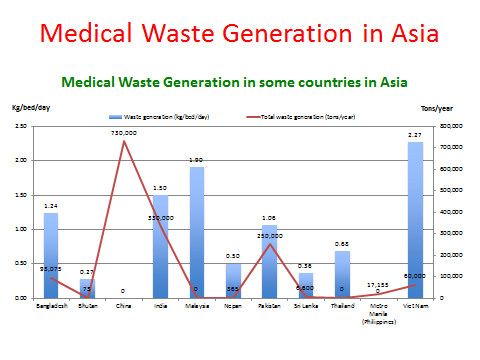
The graph above shows that different countries produce different amounts of medical wastes based on their population size and other demographic factors. According to Visvanathan (2006), across Asia, Viet Nam had the highest amount of waste generation (2.27kg/bed/day).
In 2011, Jang noted that Viet Nam is still one of the countries with a high generation rate of medical waste (higher than the Philippines, Taiwan, Korea, and Tanzania). This is attributed to several factors, including a growing population, increasing number of patients, changing lifestyle, and the increase of using disposal medical devices and access to medication, aligned with the growth of health care facilities annually (MONRE 2011; Mbongwe et al. 2008).
According to Sakaguchi (2001), in the late twentieth century, the government of Viet Nam focused on improving the healthcare system in the country. The increasing level of education in the country has also improved awareness about various diseases that has encouraged many people to take advantage of medical procedures to prevent these diseases. According to Le (2014), life expectancy in the country has improved significantly.
The Vietnamese Context
According to the Ministry of Health of Viet Nam, in October 2007, there were 1,087 hospitals with 140,000 beds in Viet Nam (1,023 public hospitals and 64 private hospitals) (Hoang 2009). In 2012, there were 1,250 hospitals (1,095 public hospitals and 155 private hospitals) (Ministry of Health 2013). The most recent figure from the Viet Nam Health and Environment Management Agency is 1411 hospitals nationwide (VIHEMA 2015a).
It is estimated that the daily amount of medical waste generated from Vietnamese hospitals alone is 450 tons of solid waste in 2015, comprising approximately 47 tons of hazardous solid waste (VIHEMA 2015b). It costs more than 500 billion Viet Nam dong (25 million USD)/year) to treat that waste and hospitals have to bear this cost without a separate fund allocated from the state budget.
The medical service fee charged does not cover the fee either (Mejia & Sattler 2009). This is a major challenge for the health care system in Viet Nam. Another issue is the number of patients served daily. It is obvious that a high number of patients served per day will lead to a higher amount of medical waste generated (Manyele & Lyasenga 2010). The World Bank estimates that it needs 500 million USD to develop the appropriate medical waste treatment system infrastructure (VIHEMA 2015b). The table below shows the amount of medical waste generated in Vietnamese hospitals.
Table 1: The amount of medical waste generated in Viet Nam (MONRE 2011)
Risks Associated with Medical Waste
Public injury and infection
Bokhoree et al. (2014) indicate that whilst the amount of medical waste can be quite small versus the amount of total waste generated in a community, it poses more serious risks to human health in direct and indirect ways. Individuals like medical staff, patients, workers in waste disposal facilities and the general public are at risk of being injured or infected if exposed to infectious/hazardous waste, largely because physical injuries caused by discarded sharps may directly contribute to the transmission of microbial infectious agents.
According to the Pruss, Giroult, and Rushbrook (1999), human immunodeficiency virus (HIV), and hepatitis viruses B and C can be transmitted via healthcare waste. The WHO (2002) estimates that over the past ten years, there have been over 20 million infections of Hepatitis B, C and HIV globally associated with reuse of syringes and needles in the absence of sterilization. Additionally, the sale of recovered drugs also poses a risk to public health (WHO 2002).
Salkin (2004) confirms that health care waste contains hazardous components which pose physical, chemical, radiological and/or microbiological risks to occupational and public health, and needs to be treated properly before disposal. Furthermore, amongst the health care waste, hospital waste (10-25%) has a higher potential for injury, infection and environmental pollution, and when mixed with other waste sources, it can lead to the entire bulk of the waste becoming infectious (Bryman & Bell 2011).
Mato and Kassenga (1997) indicate that diarrhoea, leptospirosis, typhoid and cholera can be transmitted through untreated medical waste. The Viet Nam Health and Environment Management Agency and the Ministry of Health (VIHEMA 2015c) have pointed out that the number of broken thermometers (estimated by the UNDP) is 447,588 units /year. This leads to the release of 550kg of mercury/year to the environment (Moreira & Gunther 2013). The mercury poisoning following high-dose exposures leads to neurotoxicity.
Soil and groundwater contamination
There are also several indirect risks posed to the environment when dumping medical waste in uncontrolled areas. Studies have shown that the major effects of medical waste on the environment are water and air pollution (Hoang, 2009). This includes the contamination of soils, especially if the waste is non-biodegradable (Shah & Ranghieri 2012). Wastes that dissolve in water can contaminate groundwater, rendering such waters unfit for human and animal use (Hoang 2009). Foster (1996) argues that the real environmental impact is groundwater contamination, which affects drinking water supply.
Emissions from incineration
The two primary ways of treating medical waste are disposed to landfill (not applying to infectious medical waste) and incineration. Incineration, also known as thermal treatment, is defined by Le (2014, p. 56) as “a waste treatment process that involves the combustion of organic substances contained in waste materials.” The method is mainly used in treating combustible wastes that may pose a serious hazard if not properly disposed of (WHO 2014).
A proportion of medical waste is general waste and is incinerated together with the other wastes in the incinerators. Johnke (2000) confirms that the generation of climate-relevant emissions from the incineration of municipal waste is CO2 (carbon dioxide), N2O (nitrous oxide), NOx (oxides of nitrogen), NH3 (ammonia) and organic carbon. Abor (2007) points out that incineration of medical waste, in a South African context, has been associated with many health problems such as disruptive body hormones, the immune and reproductive systems, and cancer.
Dioxin – one of the most toxic substances if is inhaled or digested – can cause cancer through genetic change (EPA, 1997). Le (2014) indicated that incinerators which are used for burning industrial and medical wastes are responsible for dioxin emissions in Viet Nam. The EPA (1997) pointed out approximately 87% of mercury emissions come from combustion sources and if not managed properly may leak into the environment, a problem that is common in the developing countries such as Viet Nam (Carpenter & Hoppszallern 2010).
Given the above potential environmental and health impacts, it is clear that managing medical waste sustainably will reduce the number of pollutants that directly impact on climate change and public health in Viet Nam.
Medical Waste Management Policies and Regulations
Environmental protection became a legal obligation for the health care sector in general, and hospitals in particular (Richardson et al. 2012). Laws, policies, regulations and guidelines have been developed at international, national and hospital levels to establish a legal framework to protect human and environmental health against the risks from medical waste (Van 2015).
One of the common guidelines is colour-coded bins and bags to ensure correct segregation to prevent infection and injuries within and outside hospitals (Chaerul, Tanakab & Shekdarb 2007). The guidelines also provide information about medical waste substances that can be destroyed through incineration and those that require alternative waste management methods. The table below shows the legal documents underpinning medical waste management in Viet Nam.
Table 2: List of medical waste management policies and regulations (Viet Nam Laws)
Table 3: List of government programs on medical waste management (VIHEMA 2015a, p. 45)
It is worth noting that having policies and guidance in place is only part of the picture. Mato and Kassenga (1997) noted that even though a national standard for segregation (to ensure effective treatment) of hospital waste is in place, it is not applied adequately throughout the country. The issue is not a lack of legislation and policies but a lack of commitment to their implementation. The factors influencing this implementation of waste regulations and policies are explored further in the following sections.
Enablers/Drivers for Sustainable Practices in Medical Waste Management
This literature review explored the existing research around the enablers for sustainable medical waste management in a hospital context. Many authors when studying medical waste management have sought to identify the factors enabling the embedding of the 3Rs of Reduce, Reuse, and Recycle in hospital policy and practice around medical waste management (Cheng et al. 2009).
There are, of course, many different dimensions to this topic (Coker 2009). The available waste collection infrastructure, the capital available for investing in treatment infrastructure, and the particular medical products available to the procurement teams are all examples of material issues that will affect medical waste management (Strohschen 2009). This review focuses on the literature that specifically relates to the role of health care workers, and seeks to summarise the key themes emerging, as a basis for testing their application in a Vietnamese context.
Training and education at all levels
Chaerul et al. (2007) observed hospital waste management practices in Indonesia and pointed out that various issues (safety, public health, environmental conservation) are rarely considered by hospital management. The authors gave the example where infectious waste is mixed with municipal solid waste and disposed of in the landfill sites without any treatment before disposal.
Mato and Kassenga (1997) and Askarian, Vakili, and Kabir (2004) in their studies in Iran and Tanzania respectively identified that low awareness regarding the importance and benefit of sustainable hospital waste management was due to a range of actors, including staff unwillingness to participate, lack of motivation, limited training and education. Manyele and Lyasenga (2010) also pointed out the other factors contributed to such poor medical waste management is the involvement of individuals who lack medical knowledge when it comes to medical waste management.
Lee (2002) concluded that to increase recycling of wastes, education of workers and managers, and efforts of the entire hospital staff should be pursued. Tudor et al. (2008) confirmed that sustainable waste management programs should be targeted towards specific departments and involve staff throughout the entire process. There appeared to be a lack of consistency between the national guidance and local practices because the involved stakeholders are not taken through regular training, for example, the definitions of what constitutes clinical waste.
This leads to a situation where people develop their definition and sometimes create confusion when it comes to waste segregation. It shows how important training is and it relates to staff motivation. Richardson et al. (2012) suggested regular training for the nurses, doctors, janitors, and other medical staff who handle wastes in one way or the other. Regular training is meant to ensure that they understand the emerging trends in waste management (Strohschen 2009). The training can help staff have a better understanding of how to segregate clinical wastes.
Engagement and rewards
In the organisations where Richardson et al. (2012) conducted their study trying to understand the behaviour of non-staff stakeholders at a hospital regarding waste management, it was found out that effective and efficient waste segregation was rewarded. This was a good way to keep staff motivated to embrace the good practice, especially as existing staff could be shadowed by new ones and the good habits would be picked up (Kojima & Michida 2013).
Another suggestion emerging from the literature was that institutions could develop policies where each department is rated based on how effective they manage wastes and the department that comes at the top is given some form of reward as a sign that their commitment towards maintaining a clean medical environment is appreciated (Controlled Waste Regulations 2012). This can be done monthly. It was a good way to keep staff motivated to practice well. The approach will promote good practice in medical waste management.
Staff capacity
A study by Nichols et al. (2013) noted that a key factor affecting the ability of health care workers to carry out sustainable medical waste management was a heavy workload, leaving insufficient time “to do something massively different.” (p. 41). Manyele and Lyasenga (2010) argue that effective medical waste management is affected by the number of workers in health facilities.
In Viet Nam, according to the Joint Annual Health Review (2014), the number of health workers reached 7.5 doctors per 10,000 populations, although these are unequally distributed across regions and specialities. In Hanoi and Ho Chi Minh City, it could be 14 doctors per 10,000 population compared with 4-5 in far provinces (Joint Annual Health Review 2014). This imbalance can lead to the migration of patients to public hospitals in Hanoi and Ho Chi Minh City, which then leads to further overloading for the health workers there.
Working environment and infrastructure
Nichols et al. (2013) also noted that a key factor affecting the ability of health care workers to carry out sustainable medical waste management was the lack of space for recycling. When the environment lacks the right equipment such as waste segregation bins and medical waste incineration systems among others, then it may not be easy to manage wastes in an effective manner (Ozbek & Sanin 2004).
These two scholars argue that the management should always be supportive to the junior employees to create an environment where they can positively engage to find solutions to problems affecting their operations. Richardson (2012, p.16) argues that “individuals will change behaviour when it is easy for them to do so.” It means that the working environment should facilitate easy management as well as the removal of waste (Delving 2006). If not, the people who recycle at home may find it difficult to recycle at work.
Green champions
In their study in a county in the south-west of England, Nichols et al. (2013) found that participants identified the importance of understanding sustainability and waste management issues and this information being disseminated by ‘Green Champions’, driven by both environmental and financial points of view (Strohschen 2009).
Green Champions should include sufficient seniority to be respected and provide advice rather than disciplinary actions such as penalizing poor practice. As Kojima and Michida (2013) say, the aim should be to motivate the stakeholders, not through fear, but through a desire to have a sustainable environment that is appropriate for both the staff and patients.
The important role of nurses
Several studies point out the importance of nursing staff in promoting sustainable waste management. Harris et al. (2009) emphasised the important roles that nurses can play to make the hospital an environmentally sustainable setting. Nurses account for the largest number amongst the healthcare professionals in the health care sector and have the best opportunities to promote green initiatives (Nichols et al. 2013).
In daily work, nurses are interacting with the top hospital leaders and other stakeholders like patients, family and friends of the patients, and suppliers, providing them with opportunities to use the nursing process in education and policy efforts to promote going green (Dinkins & Sorrell 2007). Nurses can conduct orientation training for new staff regarding medical waste management and educate the patients. McDermott-Levy (2011) argues that nurses should become members of a hospital green team and influence product selection and appropriate product disposal.
Embedding in legislation, policy and practice
Nichols et al. (2013) concluded that legislation and regulation provide a driver and incentive for positive and sustainable changes in the management of medical waste. Studies have discussed the use of policy and practice interventions that can reduce the volume of wastes in the hospital.
A study by Almuneef and Memish (2003) conducted in Saudi Arabia has shown that a well-formulated waste management plan (written policy, mandatory in-service education, continuous waste audit and cooperation of all staffs) caused a 58% reduction in the amount of infectious waste incinerated which lead to more than 50% cost saving in fuel, labour, and spare parts.
In Richardson’s (2012) study, the participants shared their ideas of change, including ways to improve legislation, procurement, and interaction in terms of best practices. In terms of legislation, the legislators (Government, health care managers) should listen to the frontline staff to enhance receiving right feedbacks aimed at changing legislation (Clover 2009). This helps to ensure that the guidance on recycling of waste is taken into account at the clinical level.
The government of Viet Nam, through the Ministry of Health, Parliament, and other institutions, has developed policies and regulations that should be followed by various stakeholders in the healthcare sector to ensure that there is effective disposal of medical wastes.
According to Coker (2009), there should always be consistency between national guidance and local practices. A study by Richardson et al. (2012) focused on understanding current practices across public and private institutions managing healthcare waste in the U.K., found out that there appeared to be a lack of consistency between the national guidance and local practices because the involved stakeholders are not properly empowered.
Research Gaps
The literature reviewed provided a rich insight into the research topic, in particular identifying a range of potential drivers and enablers in embedding sustainable waste management in a medical context. Many of these studies, however, were conducted in a developed country context. Literature that specifically addresses sustainable medical waste management in Viet Nam are limited and disjointed (Le 2014). As such, further investigation is necessary for this area. Many of the studies above address the policies, plans, training, role-modelling and incentives and infrastructure that may encourage sustainable waste practice (Newswire 2016).
This study will aim, first of all, to examine the applicability of these strategies and practices in a Vietnamese context. Secondly, having identified various enablers and drivers, the research by Nichols et al. (2013) also suggests the need for further investigation about barriers to behavioural change.
This study will look at these barriers and how they might be overcome to foster an environment that is supportive of sustainable medical waste management at various levels. As McDermott-Levy (2011) notes, understanding the nature of change when introducing new policies is very important. In the analysis, the researcher will look at these changes that need to be put into consideration when coming up with new medical waste management.
Research Method
The methodology of this study was determined by the study aim. This chapter describes how the research was conducted including research design, subjects, data collection, limitations and ethical considerations.
Setting up the Study
The author initially contacted the Vice Director of the Viet Nam Health Environment Management Agency (VIHEMA), which is a unit within the Ministry of Health, to get his advice on which public hospitals performed well in medical waste management based on his expertise and supporting data. Following his consultation, the author selected two public hospitals with appropriate access for data collection. These were the ‘National Hospital of Tropical Diseases’ in Hanoi and ‘Thong Nhat hospital’ in Ho Chi Minh City. Both hospitals are under the management of the Ministry of Health.
The National Hospital of Tropical Diseases was developed from the infectious disease department of Bach Mai hospital which was established in1911. As such, it has inherited the Bach Mai’s waste treatment and disposal system. The hospital has 300 beds and 21 departments including 8 clinical departments and 7 subclinical departments. As of Nov 2014, there were 80 doctors and 203 nurses, amongst a total of 363 health care workers. The treatment methods for hazardous solid medical waste are the autoclave (steam sterilization) and micro-wave (sterilization process that is based on the microwave technology). The hospital is unusual in that it does not make use of an incinerator.
Thong Nhat hospital was established in1975. The hospital has 1,000 beds and 43 departments including 24 clinical departments and 10 subclinical departments. As of Nov 2014, there were 262 doctors and 565 nurses, amongst a total of 1,209 health care workers. Whilst it is responsible for collecting waste, the hospital does not treat hazardous waste inside the hospital. The third-party company collects it and is responsible for that treatment.
Research Design
The research design adopted was an exploratory investigation based on a qualitative approach. In the handbook of qualitative research, Denzin and Lincoln (2005, p.3) describe qualitative research as involving “an interpretive naturalistic approach to the world. This means that qualitative researchers study things in their natural settings, attempting to make sense of or interpret phenomena in terms of the meanings people bring to them.”
The qualitative approach was applied following a constructionist ontology and interpretivist epistemology. This recognises that the healthcare workers participating in the study would be constructing their own ‘reality’ of the situation based on their knowledge of the subject and their perception of what they had been doing towards sustainable medical waste management (Bell 2001). It also recognises that the researcher’s role is to interpret through those social constructions (Calabrese 2006).
Qualitative research is a research strategy that usually emphasizes words rather than quantification in the collection and analysis of data (Bryman & Bell 2011, p.386). In this research study, the qualitative approach consisted of twenty interviews with health care workers – doctors and nurses at different management levels – who were involved in medical waste management as a daily practice in two public hospitals in the two largest cities (Hanoi and Ho Chi Minh City) in Viet Nam.
The selection of these two hospitals is explained in section 3.1. The participants were interviewed to establish their current knowledge and awareness of the 3Rs approach to sustainable medical waste management, and the enablers and barriers to practice.
The data collection took place in two weeks of January 2016.The semi-structured interviews had a list of questions to be covered in venues agreed by the participants. An ‘interview guide’ (Goddard 2001) was used, which allows consistency of questioning in interviews whilst providing some freedom to build a better rapport with interviewees (Bouma 2000). Open-ended questions were used to enable the participants to justify their responses (Dunleavy 2003). The participants were briefed that the interviews would be coded to ensure anonymity, to encourage them to speak candidly. They all signed up to this process. Participants were identified in the analysis by a special number and hospital name (Gupta 2002).
Key question themes that were covered include the following:
- What are the current strategies used by the healthcare institutions in Viet Nam in managing medical wastes?
- What is the level of awareness among the stakeholders on sustainable management of medical wastes?
- What are the barriers that currently exist in seeking to implement 3Rs strategies?
- What can be done to promote sustainable medical waste management in Viet Nam?
The interviews ranged from 20 minutes to 45 minutes. All the interviews were digitally audio-recorded and transcribed. Following the completion of all interviews, the author undertook a process of coding common themes in a spreadsheet, identifying categories from the data, and summarising key themes, using an inductive approach (Brause 2000). The findings were then analysed in light of the original literature review, and effort was made to understand and interpret the behaviour of healthcare workers regarding how they understand the importance of medical waste management, how they prioritise actions, what barriers they perceive, and how it is mobilised within hospitals.
Sampling
The initial meeting in each hospital was with the Heads of the Nursing Department, during which the objectives of the study were explained. They were then requested to provide a list of doctors and nurses across the various hospital departments. The sampling strategy used in this research was a judgment-based sample approach based on the research question (Hakim 2000).
A snowballing approach was also used, identifying additional interviewees through recommendations from other interview respondents (Hinkel 2011). In both hospitals, hospital staff across different departments were approached, including both doctors and nurses in internal infectious and infection control departments, environmental specialists, and representatives from the management board (the Director or Vice Director of each hospital).
Twenty interviews were felt to represent a saturation point in the collection of data. Saturation is defined as “the point at which no new relevant information is forthcoming, even if more people are interviewed” (Galvin 2015, p.3) to ensure collected data was sufficient for analysis. Hospital documents (hospital guidelines and reports related to hospital waste management) were also analysed.
In this study, the sample included only two different groups of people who were interviewed. The first group of people were the doctors and the second group of people were nurses at the two hospitals that were identified. For the analysis, the researcher used TN to denote participants from the first hospital and ND to denote participants from the second hospital. The table below is a detailed identification of these participants based on their positions at the different hospitals.
Table 4: Sampled participants (developed by the author)
The classification system helped the researcher identify the participants in the study (Cramer 2003), whilst preserving the anonymity of the respondents. According to Andrzej and Buchaman (2007), it is ethical to conceal the identity of the respondents, especially if others can have access to the report. There are cases where people may be victimised because of their views which may contradict that of the majority (Creswell 2009).
In some studies, those in management positions have issued punitive measures if it is perceived that an employee has issued confidential information or maligned the image of the organisation. Protecting the identity of the respondents makes it almost impossible for them to be individually victimized (Anderson 2004). The codes also make it easy to classify the respondents and the responses based on the class in which the respondents fall. This way, it becomes easy to identify the pattern of response based on the area of expertise and experience of the respondent.
Limitations
According to Badenhorst (2007), when conducting a research project, several limitations may be encountered based on several factors that playoff in the course of planning, data collection, analysis, and presentation. It is important to highlight these limitations and where possible, state how they were dealt with in the study to promote the validity and reliability of the report.
In this study, the researcher encountered the following limitations.
Sampling
When sampling the respondents, the researcher was at liberty to choose the participants for this study. This posed a potential challenge inherent in selecting a given group of respondents over others (Hoyle 2002). In particular, I gave more focus to the nurses over other respondents because of the personal belief that they are more responsible for medical waste management in healthcare institutions. I made an effort to eliminate or minimise the effect of personal biasness when selecting the samples by trying to pick the respondents in each of the two strata.
Personal position and its effect on interviewees
It was noted that my position as a Director at a pharmaceutical company could have influenced the response received from some of the respondents (Denzin & Lincoln 2011). Some of those interviewed requested to know my position before answering the questions. Most were satisfied with the assurance that their identity would remain anonymous, hence they appeared to answer the questions freely without seeming to attribute any importance to my personal views.
For one or two respondents, however, even after being assured of anonymity, there was a fear that they might be reported to the authorities. There was also the risk that such respondents provided answers to ‘please’ rather than sharing their honest views. It is important to note though that this problem was not common among all the respondents. Only a few of the respondents exhibited this behaviour.
Collecting data from only two hospitals
According to Barzun (2004), the problem of medical waste management varies from one institution to another and from one geographical setting to the other. There are cases where the problem is with the infrastructure, while in other cases the main problem is with the stakeholders involved.
The factors affecting private hospitals in terms of medical waste management may also be different from what is affecting public hospitals. In this research project, only two public hospitals were selected and consequently could not represent the entire population. Nonetheless, the study elicited insights for the chosen two contexts, which can then be tested for their applicability in other geographies or privately-owned institutions.
Primarily focusing on practitioners’ behaviour
Poor medical waste management is a problem that is caused by infrastructural, financial, and behavioural forces. When an institution lacks proper infrastructure to manage medical waste, then it may be impossible to safely and effectively dispose of these wastes. Financial considerations are also significant, in determining purchasing decisions, use of suppliers, and capital investment in equipment and infrastructure. There is the need to ensure that bills are paid and proper tools are purchased or replaced from time to time to enhance the efficiency of the system (Earl 2009).
In this paper, these two important factors were acknowledged as context, but the primary focus was placed on practitioners’ attitudes and behaviour towards medical waste management. Moreover, the research focused on healthcare workers, rather than the role of other functions within the hospital context, for example, procurement. The findings, therefore, should be examined in this light and would do well to consider other research looking at other dimensions of the system.
Relying on peoples’ reporting
This study largely relied on people’s reporting of their behaviour to understand the forces affecting the effective management of medical wastes. As Barthe (2010) says, sometimes people may deliberately hide the truth from a researcher for personal or organisational reasons. This is particularly common when interviewing people in managerial positions.
There is often the feeling that they are responsible for mistakes or shortcomings at the firm. To protect themselves, they might be tempted to cheat or provide half-truths. It may have been more appropriate for the researcher to observe the behaviour and attitude of the stakeholders in the sampled institutions without their knowledge. However, the amount of time available for the study could not permit the researcher to make such observations. The study had to rely on their reporting, assuming that their statement would be a fair reflection of their attitude and personal behaviour towards the issue under investigation.
Ethical considerations
The research study required the approval of the Viet Nam Health Environment Management Administration (VIHEMA), the Ministry of Health, and the hospitals’ Management Boards to research public hospitals. No patients were involved in the research.
The research was informed, designed and conducted in adherence to current principles applying for research involving human subjects, such as the right to withdraw and confidentiality, including demonstration of respect for all participants (Nurse and Midwifery Council 2008). A consent form was obtained, for each participant and, as explained earlier, all interview responses were coded for anonymity.
Findings and Analysis
The previous chapter has given a detailed analysis of the method that was used in collecting and analysing data. In this chapter, the focus will be on the analysis of the data and presentation of the findings. The study was designed to explore the level of knowledge and awareness of health care workers (doctors and nurses) about the 3Rs strategy in sustainable medical waste management, and to identify key drivers/enablers for implementing a 3Rs strategy in medical waste management in Vietnamese public hospitals, including quick wins and long-term objectives, and analysis of barriers.
The chapter outlines the findings from the qualitative interviews. These have been illustrated where appropriate by relevant quotes. As explained in the above chapter, the participants included 14 nurses and 6 doctors in different positions in the two hospitals. In the first part of the interview, the participants shared their view on current situation and factors influencing the good practices at their hospitals in terms of medical waste management. It is important to note that consideration of barriers is explored as part of exploring the enablers for change, because of the overlap in themes emerging.
Current situation
Based on the findings of this study, it is evident that in both hospitals where the primary data were collected, doctors and nurses are aware of improper medical waste management and its impact on humans and environment health. The awareness regarding this impact determines the attitude and practices in medical waste management among these medical staff. It is also evident that, the participants are satisfied with their organisation’s performance in medical waste management and understand the factors influencing good practices.
However, they showed their concerns about medical students, patients and their caregiver’s incorrect practice in medical waste disposal. As will be shown in this chapter, these participants felt that sustainable medical waste management needs attention of other relevant stakeholders, not just the medical staff alone. The respondents noted that irresponsible practices among the non-medical staff who visit hospitals regularly made the process of managing wastes more complex.
The respondents argued that recycling of some of the medical wastes may be one of the ways of enhancing sustainable waste management. To achieve success, these respondents emphasized on the need to embrace training and education for the medical staff, effective leadership among the administrators, proper supervisions at work, having adequate and modern medical waste management facilities in hospitals, and proper regulatory procedures. They also mentioned the need to promote knowledge about 3Rs principle among the medical staff.
Factors affecting good practices in medical waste management
Effective management of medical wastes is affected by a number of factors as was revealed in this study. The following are the factors that were identified.
Leadership
All the respondents were unanimous about the relevance of leadership in effective management of medical wastes. They noted that leaders play a critical role in defining how wastes are managed within a healthcare facility. The director of the hospital is the person accountable for medical waste management within the hospital as defined by the Ministry of Health.
A number of participants confirmed that they are reminded regularly by their director about the need to pay attention and strictly adhere to the set guidelines when it comes to waste management. They also noted that the head of department and head of nurses often talk about waste management during hospital meetings and department meetings. In Thong Nhat Hospital, the director was praised as a leader who understands the need to have proper waste management system within his institution.
The interview results from the two hospitals show that it is very critical to engage all the stakeholders when trying to implement 3Rs strategy. The response shows that the support from management board is essential to encourage the implementation of medical waste management in hospitals.
“The support of the management board is the foundation to build the background and to give the right orientation for developing all specialties from clinical to para-clinical and step by step standardise all activities and procedures” (ND2).
This claim was also supported by another participant who stated the following:
“The management board must pay attention and prioritise the need for a ‘clean and hygienic’ hospital environment.” (TN2).
The participants also emphasised the need to ensure that all other healthcare workers are included in the entire process of strategy development and implementation. Those in management and non-management positions ought to work very closely to ensure that the desired success is achieved (TN2).
Training and education
The respondents unanimously confirmed that in order to reinforce the importance of the effective and efficient medical waste management, each hospital regularly conducts training and refresher training to promote awareness on health, safety, and environmental issues. Knowledge about handling and segregation of medical waste was noted to be very important during training processes.
The repeated training helps healthcare workers improve their knowledge of the risks caused by improper waste handling and segregation. This task is under the scope of the Infectious Control department in both hospitals. Hospital guidelines on medical waste management are summarised, printed, and posted on the wall in all departments of both hospitals.
Organising regular training on medical waste classification is a key action needed to achieve the required levels of best practice in hospitals. The analysis revealed that the targets for training should not be confined to hospital staffs that engage daily on medical waste management, but should be expanded to cover all the relevant categories such as caregivers and medical students.
“The hospital has a continuous education program organised by the Infection Control Department. There is a Patient Committee that involves 1 – 2 patients of every specialty. Nurses will communicate with patients and their caregivers about the regulations right from the beginning” (TN3).
The statements from these respondents indicate that regular training is a very important enabler of this strategy. It empowers the stakeholders and makes them be aware of the environmental forces within their workplace. “The training should be repeated yearly in order to instil the habit” (TN9).
The response shows that it is important to ensure that the training is as detailed as possible to make the relevant stakeholders to understand what is expected of them. One respondent gave the following recommendation.
“It is important to build capacity for nurses to ensure good practices and avoid repeated practices which lead to increasing the amount of waste” (TN4).
It is the responsibility of the management to build capacity and to promote best practices based on the industry standards. Nurses need regularly training to sharpen their skills and enable them understand emerging forces that affect their work.
“Apprentice, caregivers, and visitors do not know what constitutes medical waste and its classification. Knowledge of medical waste management was also lacking” (TN5).
“There are many cases of in-correct disposal of medical waste into the wrong recycle bin, especially by caregivers due to lack of knowledge” (TN10).
“There are many cases of in-correct disposal of medical waste into the wrong recycle bin, especially by caregivers due to lack of knowledge” (TN10).
It is, therefore, important to come up with proper guideline for training these caregivers on strategies they should use in managing medical wastes. The limited knowledge of patients, caregivers, and medical students on what constitutes ‘medical waste’ is a major barrier for hospitals in reducing medical wastes. They tend to confuse normal waste and medical waste due to their limited of knowledge.
Supervision
The respondents confirmed that both the hospitals in which they work implement a regular supervision scheme, including ad-hoc and periodically checking for segregation of medical wastes. Across all departments, nurses are responsible for correct segregation of wastes into the bins. The head of nursing is also responsible for cross-checking between departments.
Their names and signatures appear on the bags when they are transported to the infectious department. When mistakes in segregation step are identified, the written minutes are recorded and shared in the hospital meetings to improve their performance and give warning to the other departments. Moreover, ad-hoc and regular supervision from the Ministry of Health and Department of Environment also takes place, which prepares the hospital for strict implementation.
The interviews conducted indicated that the role of regular follow up and back checks is critical to ensure there is compliance. Being compliant with the national standards is the first step towards ensuring that these hospitals embrace sustainable practices in waste management. Hospitals recognised the importance of supervision by an empowered team for periodical back checking. This is shown in the response shown below.
“The Infection Control Department has monthly supervision and random checking without notice. There back checks within specialties, performed by nurses. The checks are often conducted without prior notice in order to test the efficiency of the system to give regular feedback” (ND5).
“Thanks to training and regular checking, the knowledge of hospital employees about waste management has improved. Many hospitals are now applying ISO standards and do make regular notes when they discover a mistake” (ND6).
It became apparent that through regular supervision, it is possible to identify areas of weakness during the implementation process and to come up with measures to remedy such weaknesses.
Regulations and guidelines
One of the nurses stated that the strict regulations put in place by the Ministry of Health and clear guidelines from the hospitals governs the health care workers’ attitude and behaviour in medical waste management (ND3). These regulations are often updated regularly based on the changing trends. The interviewees confirmed that proper segregation and collection has now become a habit and is embedded in doctors and nurses’ practices (ND3).
There is neither a fine nor a reward scheme put in place so far in either hospital. In the National Hospital of Tropical Diseases, a written warning is mentioned in the hospital guidelines but not implemented yet. A verbal warning is common in both hospitals for the purpose of improving the attitude towards effective medical waste management.
All activities of hospitals on medical waste management are based on the current legal framework with decisions and guidelines of the Ministry of Health. Besides the MOH guidelines, the respondents stated that each hospital should also develop internal standard of practices (SOPs) for implementation based on each hospital’s unique situation. The following responses were obtained from the directors at the two institutions
“Regulations and guidelines of MOH and Hospitals are available and clear for action” (TN10).
“The specific hospital regulations are built up based on the Ministry of Health guidelines with direction for clear implementation” (ND7).
Their responses show that regulations and well-formulated plans can also act as enablers when implementing the strategy. They help the stakeholders to understand what is expected of them. These policies are ambitious and if implemented appropriately, they can truly bring about sustainable waste management not only at organisational level but also nationally. They can help deal with the problem of managing medical waste in Viet Nam.
Hospitals facilities
Across both hospitals, all interviewees stated that they believed their hospital was adequately equipped for segregation, collection and storage of medical wastes, with the exception of water waste treatment systems. Most of the respondents (18 out of the 20 participants) did not know about their hospital’s water waste treatment situation. It was only those working in the Infection Control Department who understood this issue.
The reason given among those working in Thong Nhat Hospital was that the hospital has a special way of doing this, which it has done for the 40 years that it has been operational. It was recognised that there is a need to invest in a new waste water treatment system which costs about $15 million, requiring state budget allocation and under consideration by the Ministry of Health. For the National Hospital of Tropical Diseases, as mentioned earlier in chapter 3, the hospital is using the same waste water treatment system with Bach Mai Hospital, which has a history of over 100 years and the participants working here refused to comment about this matter. Most of the bins are not properly labelled, which means that sorting becomes a major issue. These infrastructural challenges may have serious impact in sustainable medical waste management at organisational level.
Role of nurses
When analysing the interview results, the critical role of nurses at all levels was a repeated theme regarding good practices in medical waste management. Heads of nursing are the ones who motivate the hospital management and committee to initiate change management programs. They are responsible for the smooth running of the hospital in general and medical waste management in particular. They are also responsible for supervising the segregation and collection at the point of waste generation within the department.
They are members of Hospital Infectious Control Committee. The duty of the committee in both hospitals is to propose the revision of hospital guidelines in alignment with the Ministry of Health regulations. The committee is also expected to propose solutions to solve issues identified in daily practice, organise training, oversee communication programs, and undertake scientific study regarding control of infectious wastes in general and medical waste management in particular (MOH 2009).
Heads of nurses are responsible for training and educating new staff and medical students before they can come to work in the hospital. One respondent said, “At National Hospital of Tropical Diseases, all the new nurses and other staffs are taken through training before they can be assigned official duties,” (Van 2015, p. 12).
Analysis of the interview responses indicates that nurses are understood as the ones who should engage doctors, medical students, patients and their caregivers to ensure proper segregation and collection of waste. Before the waste is transported to the hospital’s storage area, in both institutions, they are responsible for checking to ensure proper segregation and identifying any mistakes.
Nurses are responsible for instructing patients and their caregivers on proper segregation of waste and following up their daily treatment until the treatment is completed. Given that nurses often have limited time to attend to patients, sometimes it may not be easy to ensure that these caregivers follow the instructions given.
In the hospitals, nurses participate in the Infection Control Committee of hospitals and are assigned to check and supervise the implementation of medical waste management in healthcare centres.
“In hospitals, the head nurse is responsible for checking if the guidelines are effectively followed” (TN1).
“The Infection Control department periodically checks the waste classification with what has been deposited. Nurse department also participates in the checking. The Head Nurse is responsible for checking at the Department” (TN4).
It was noted that nurses actually have many difficulties in the role of supervising the performance of medical waste management. Local nurses often find themselves faced with heavy workload compared to other regional countries, and it impacts on the effectiveness of their daily work of medical waste management.
“Release workload for nurses: currently, a nurse takes care of 3 – 4 patients. The expectation is one nurse taking care of 1 – 2 patients” (TN7).
Together with the workload, some interviewees suggested that the mind set of physicians is also a challenge for nurses in the management and control of medical waste in hospitals, specifically around issues of respect: “Physicians should coordinate with nurses. In developed countries, physicians respect nurses” (TN5), with the implication that this was not the case in the Vietnamese context.
A further example given was around the attitude towards the use of specific medical materials:
“Injections will increase contagious medical waste. It is necessary to reduce injections and replace it with oral drugs. We also need to change the mindset of physicians to reduce injections because they sometime prefer injections. Reducing injections also helps release workload of nurses” (TN5).
Awareness and Implementation of the 3Rs
It was noted that most of respondents understand and support the need to have effective medical waste management systems. Through sharing during the interviews, it seems there are many challenges in implementing the concept in the current condition of Viet Nam public hospital. People understand that reducing medical waste will help protect the environment. The plan is available in hospitals but the feasibility is still a question in the condition of overstretched hospitals.
All of hospital management board know and want to apply 3Rs concepts in the hospitals for both cost saving and environmental protection but the deployment in the hospitals is not enough and it may have the synchronised actions in the whole society. The consciousness on 3Rs should be well promoted in the society, instead of waiting for people to be hospitalised to be informed on how to manage medical wastes. Reducing medical waste is very important in enhancing management of medical waste.
“All hospitals, not only in Viet Nam but also the world, would like to apply 3Rs but it is still a challenging to implement. Contagious waste will become normal waste after treatment and can be recycled. However, not everyone has the same understanding especially people in the society and environmental officers. Reducing and recycling will help hospitals reduce costs. However, hospitals do not have the permission to perform it themselves (It will be performed by professional third parties following the current regulations)” (ND4).
As noted in the above response, sometimes regulations may limit the capacity of individual hospitals to perform certain functions when it comes to management of medical wastes. In most of the cases, the major issue is often the feeling that these hospitals may not follow the right procedure in managing some medical waste which poses serious threat to the environment.
“The plan to reduce medical waste is available but it is still on paper” (TN2).
“Reducing solid medical waste is impossible because it depends on the number of patients, except shortening the treatment time for in-patients. It is very difficult to save water since it is required for the purpose of cleansing” (ND3).
Currently, hospitals have limited application of the concept by reuse of water bottles and glasses, and it is the most popular practice in the hospitals currently. It is important to promote knowledge on the issues of reuse based on the 3Rs strategy. The respondents gave suggestions on how to implement this strategy. One of the respondents stated.
“To reduce medical waste, the plan is available but the implementation is not as easy as anticipated i.e. we cannot reduce plastic bags although it is accepted as a necessary action. Hospitals cannot immediately reduce medical wastes and the current focus is to just focus on how to better manage them” (TN1).
“Hospital can reuse plastic and glasses bottles only” (TN3).
“Glass materials can be reused, but it will need water and manpower to wash, and electricity to dry to sterilise” (TN8).
In the second part of the interviews, the participants were asked about what they understood by the term reduce, re-use, and recycle. Amongst 20 interviewees, there were only 3 persons- who belong to the Infection Control Department- who understanding this strategy as a way to minimise the impact on both financial benefit and human/environmental health. 12 people knew the term recycle because of recycling activities.
However, all of them doubted the feasibility of the deployment. For ‘reduce’, they said that they cannot reduce the number of patients but admitted that reducing of injection products and reducing the days of in-patient treatment by controlling cross-infection can reduce the amount of medical waste. For ‘reuse’, they argued that high demand of disposable medical devices which are safer than reused ones is creating the challenge for reusing.
The participants identified the barriers such as water, electricity, chemicals, time, and human resource needed for cleaning and disinfection in order to reuse those devices. They also noted that most of hospitals have inadequate staffing in terms of health care workers. The shortage puts a lot of pressure on the existing nurses, making it difficult for them to undertake some of the time consuming recycling processes. For ‘recycle’, most of recycling activities take place outside the hospital and out of the hospital’s control because of the existing policies.
That is the reason the cost benefit is not measured. The hospital only promotes the strategy to save water, electricity, and reduce cost of buying chemicals and other materials. These are consumables that these hospitals have full responsibility on. This could be a key area for supervision and control by a designated MOH team to significantly improve this area. The official data from both hospitals shows that one nurse has to serve 3-4 patients (1/3-4) whilst the ideal ratio should be 1/1 as is the case in the developed countries. This rate is even higher in the Intensive Care Unit department (1/4-5).
Healthcare Practices
In light of the challenges identified above regarding implementing the 3Rs, the responses obtained from the participants strongly indicated that specific healthcare practices embraced by workers can be enablers of implementing a 3Rs strategy. Some practices can hinder the implementation while others can enhance it. Policies and plans may be in place, but the reality is still far from the ideal because of some of the practices embedded within the hospitals studied.
Some interviewees identified specific healthcare practices, which could be reviewed to enhance sustainable waste management:
- Length of stay: “Reducing solid medical waste is sometimes not practical because it depends on the number of patients. The only option is to reduce their treatment duration in hospital” (ND3). The respondents also noted that it may not be easy to reduce the amount of water used in cleaning unless the days of patients’ visit can be reduced.
- Prescriptions: “Reducing medical waste by ‘accurate’ prescriptions being generated and avoiding injections will help reduce medical wastes” (TN4) and “using paper wrap for drugs instead of nylon wrap” (TN3).
- Treatment options: “Intravenous drug usage increases the amount of waste. It is needed to change doctors’ perception to increase oral drug usage. It also helps reduce workload for nurses” (TN5).
Nurses also ought to be careful when handling gloves because in most of the cases it may not be possible to recycle them, especially when handling different patients.
- Efficiency in routine procedures: “Improving the skill of nurses and avoiding repetitive operation are also solutions to reduce medical wastes” (TN4) and “[Reducing] in-patient time by using effective and efficient treatment” (ND2).
- Infection control: “Better management of hospital infections and controlling medical waste will help reduce cross-infection in hospital and shorten the duration of treatment of patients” (ND2).
- Certain technologies and procedures: Under the current practice and technologies used in cleaning medical equipment and facilities, specific volumes of water must be used. “It is very difficult to reduce waste water since there is a minimum volume for cleaning” (ND3).
The respondents also noted that procurement is another important issue as part of medical practices. The management is expected to have a procurement system that ensures that all drugs and any other medical consumables are delivered at the right time, in the right amount, and the right state to eliminate unnecessary wastages. Through effective procurement, the amount of medical wastes can be significantly reduced.
One respondent commented that it was important “to plan well for purchasing drugs aimed at reducing cases of rampant expired drugs /chemicals” and “to have compensation scheme related to procurement” (TN11), whilst another suggested that “effective procurement practices will help to save cost of treatment as well as the volume of medical waste” (ND2).
The responses suggests that a time has come when stakeholders across both hospitals have to critically review the current practices with a view of being more dynamic and more focused on finding sustainable solutions to the current problem of managing medical wastes.
Summary
This chapter has provided an overview of the key themes emerging from the primary data collected from the respondents. Some of the findings support the information that was gathered during the review of literatures, whilst some findings highlight particular insights about the Vietnamese context on how medical wastes should be properly managed. Both primary and secondary sources are in agreement with the fact that it is important for healthcare organisations and the government to have effective ways of managing medical wastes.
Effective medical waste management requires a concerted effort from a number of stakeholders as shown in the above analysis. Nurses, doctors, hospital directors, caregivers, and patients all have a role to play in managing medical wastes. They must work very closely to ensure that policies and regulations regarding waste management is hospitals are followed effectively.
A number of drivers of effective waste management have been identified. Leadership, training and education, supervision, and regulations have been identified as very important drivers of effective medical waste management. Leadership helps in offering guidance and motivation when it comes to medical waste management. Training and education equips the hospital staff with the necessary skills they need in effective management of medical wastes.
Regulations outline what is expected of the staff when it comes to medical waste management. Other drivers include involvement of all stakeholders having proper regulations, and clearly outlining the role of nurses in medical waste managementThe government, medical staff, management of healthcare institutions, the patients, and the visitors all have their roles clearly defined in promoting effective medical waste management.
Conclusion and Recommendations
This study has clearly shown how important sustainable medical waste management is in Viet Nam. This study aimed to come up with effective sustainable waste management policies and practices that can be applied in Vietnamese hospitals. It was also important for the study to help increase awareness among the stakeholders in the healthcare sector on how to manage medical wastes using the 3Rs strategy. The study also focused on the barriers to effective medical waste management. In this chapter, conclusions and appropriate recommendations are given in the context of the findings of the study.
At a national level, the Ministry of Health in Viet Nam has clear guidelines in place for helping healthcare workers understand the relevance of medical waste management. The study reveals that the two hospitals studied are not fully compliant with national medical waste management policies that would help minimize risks to the environment and public health.
However, sustainable waste management arguably involves more than compliance with existing regulations, as existing regulations do not currently fully embrace the principles of 3Rs and the actions necessary for them to be implemented. Whilst healthcare workers are aware of these principles, there is evidence to suggest that they do not know exactly what they need to do to put them into practice.
Recommendations
Based on the findings from the above analysis, the following recommendations are suggested for promoting sustainable medical waste management. The recommendations, if followed properly, may help address some of the challenges that healthcare workers currently face in their efforts to manage medical wastes effectively. The recommendations target both health institutions (specifically the two hospitals examined) as well as the Ministry of Health.
For hospitals – promoting sustainable behaviour
A specific action plan aiming at reducing the waste and potential recycles (3Rs) should be in place. Potential 3Rs practices should be applied, such as:
- Proper procurement of products/devices that do not contain PVC plastic because of the challenges associated with managing plastic waste.
- Educate all health care workers, students, patients and their caregivers in regards to the urgent need to minimize the waste by strict segregation. These stakeholders should have proper knowledge on how to manage medical waste
- Developing proper infrastructure for sustainable medical waste management may also be critically important in these organisation
There is a need to find the actual cost of medical waste management in each hospital. It is also needed to have urgent studies in regards to the benefits of implementing 3Rs initiatives versus current activities. It will ease for behaviour change. In the analysis, the lack of cost-benefit analysis was identified as one of the barriers that limit the proper implementation of 3Rs initiatives. Most of these hospitals are yet to analyse the costs of implementing these strategies against the benefit they bring.
For the Ministry of Health: improve legislation, guidelines and policies
The ministry of health has to address several issues to ensure that there is the effective management of medical wastes within the country. The current regulations may need to be revised and set clear 3Rs strategy and guidance for hospitals in how to implement it successfully.
The study also found that sometimes the set policies by the ministry are not in tandem with the reality of the ground. The ministry should try and ensure that it consults the relevant stakeholders as much as possible every time it is planning on developing new policies. This way, the views of doctors and nurses will be taken into consideration. Doctors and nurses play a key role in the management of medical waste management amongst health care workers in hospitals because they have to segregate the waste before storing it in the correct bins at the point of generation, are facing daily the waste in healthcare service. Based on the information collected from the review of literature, the Ministry of Health in Viet Nam should encourage the industry to work with the government agencies together to develop standards for products and biodegradable materials used.
Recommendations for further study
This study is a source of information on medical waste management in Viet Nam. However, the result may not be applied to other hospitals. Thus, there is a need to do related research in more public hospitals in different geographies, and privately owned hospitals. Furthermore, it is needed to conduct further studies because there are issues that were not captured because of time constraints, such as water waste. Nonetheless, this study demonstrates the value of accessing the perspectives and ideas of healthcare workers, as an important step towards implementing sustainable waste management.
Bibliography
Abd El-Salam, M (2010) ‘Hospital waste management in El Beheira Governorate Egypt’, Journal of Environmental Management, vol. 91, no. 6, pp: 618-629.
Abdula, F, Qdais, A & Rabi, A 2008, ‘Site investigation on medical waste management practices in northern Jordan’ Journal of Waste Management’, vol. 28, no. 2, pp: 450-458
Abor, P 2007, ‘Medical Waste Management Practices in a Southern African Hospital’, J. Appl. Sci. Environ. Manage, vol. 1, no. 3, pp. 91–96.
Almuneef, M & Memish, Z 2003, ‘Effective medical waste management: It can be done’, American Journal of Infection Control, vol. 31, no. 3, pp. 188-192.
Ananth, A, Prashanthini, V & Visvanathan, C 2010 ‘Healthcare waste management in Asia’ Journal of Waste Management, vol. 30, no. pp. 145-161.
Anderson, P 2004, Research Methods in Human Resource Management, Chattered Institute of Personnel Management, London.
Andrzej, A & Buchaman, A 2007, Organizational Behavior, Prentice Hall, London.
AQI 2015, Air Pollution in the World: Real-time Air Quality Index(AQI).
Askarian, M, Vakili, M & Kabir 2004, ‘Results of hospital waste in private hospitals in Far Provinces, Iran’, Waste Management, vol. 24, no. 6, pp. 347–352.
Badenhorst, C 2007, Research writing: breaking barriers, Van Schaik Publishers, Pretoria.
Bak, N 2004, Completing your thesis: a practical guide, Van Schaik, Pretoria.
Barthe, G 2010, Verification, Model Checking, and Abstract Interpretation, Springer, New York.
Barzun, J 2004, The modern researcher, Wadsworth, Belmont.
Bdour, A & Hadadin, N 2007, Assessment of medical wastes management practice: A case study of the northern part of Jordan.
Bell, P 2001, Evaluating, doing and writing research in psychology: a step-by-step guide for students, Sage, London.
Birpinar, M, Bilgili, S, Erdoğan, T 2009, ‘Medical waste management in Turkey: A case study of Istanbul.’ Journal of Waste Management, vol. 29, no. 4, pp: 445-448.
Blenkharn J 2006, ‘Standards of clinical waste management in UK hospitals’ Journal of Hospital Infection, vol. 62, no. 2, pp. 300–303.
Bokhoree, C, Beeharry, Y, Makoondlall-Chadee, T, Doobah, T & Soomary, N 2014, ‘Assessment of Environmental and Health Risks Associated with the Management of Medical Waste in Mauritius’, APCBEE Procedia, vol. 9, no. 3, pp. 36-41.
Bolay, J, Hostettler, S & Hazboun, E 2014, Technologies for sustainable development: A way to reduce poverty, Cengage, New York.
Bouma, G 2000, The research process, Oxford University Press, Oxford.
Brause, R 2000, Writing Your Doctoral Dissertation: Invisible Rules for Success, Falmer Press, London.
Brundtland G.H., (1987), Report of the World Commission on Environment and Development: Our Common Future. p.16
Bryman, A & Bell E 2011, Business Research Method, Oxford University Press, Oxford.
Calabrese, R 2006, The elements of an effective dissertation and thesis: a step by step guide to getting it right the first time, Rowman & Littlefield, Lanham.
Carpenter, D & Hoppszallern S 2010, Green + Greener: Hospitals embrace environmentally sustainable practices, through laggards remain.
Cesaro, A & Belgiorno, V 2015, Medical waste generation and management in different sized facilities.
Chaerul M, Tanakab, M & Shekdarb, A 2007, A system dynamics approach for hospital waste management.
Cheng, Y, Sung, C, Yang, Y, Lo, H, Chung, T & Li C.,(2009)’Medical waste production at hospitals and associated factors.’ Waste Management, vol. 29, no. 1, pp 440-444.
Cheremisinoff, N 2003, Handbook of solid waste management and waste minimization technologies, Butterworth-Heinemann, Amsterdam.
Clarke J 2008, Clinical waste in developing countries.
Clover P 2009, ‘Safe management of healthcare waste guide’, London: Royal College of Nursing, vol. 33, no. 5, pp. 44-67.
Coker, A, Sangodoyin, A, Sridhar, M, Booth, C, Olomolaiye, P & Hammond F 2009, ‘Medical waste management in Ibadan, Nigeria: obstacles and prospects’. Journal of Waste Management, vol. 29, no. 3, pp: 804-811.
Controlled Waste Regulations 2012, Environmental Protection, England and Wales, 2016
COP21 Paris 2015, Sustainable Innovation Forum.
Cramer, D 2003, Advanced quantitative data analysis, Open University Press, Maidenhead.
Creswell, J 2009, Research design: qualitative, quantitative, and mixed methods approaches Sage, Thousand Oaks.
DARA 2010, Climate Vulnerability Monitor 2010.
Delving, A 2006, Research methods: planning, conducting and presenting research, Wadsworth, Belmont.
Denzin, N & Lincoln Y 2011, The SAGE Handbook of Qualitative Research, Sage Publication Inc, New York.
Diaz, L, Eggerth, L, Enkhtsetseg, S & Savage, G 2008, ‘The characteristics of Healthcare waste’, Waste Management, vol. 28, no. 7, pp. 1219-1226.
Dinkins, C & Sorrell, J 2007, Ethics: The Expanding Circle of Environmental Ethics.
Dunleavy, P 2003, Authoring a PhD: how to plan, draft, write and finish a doctoral thesis or dissertation, Macmillan, New York.
Dutta, S & Das, A 2010, ‘Analytical perspective on waste management for environmental remediation’, Trends in Analytical Chemistry, vol. 29, no. 7, pp. 636-643.
Earl, B 2009, The practice of social research, Wadsworth, Belmont.
EPA 1997, Mercury Study Report to Congress.
EPA 2009, Economic Impacts of Revised MACT Standards for Hospital/Medical/Infectious Waste Incinerators.
Foster, D 1996, Groundwater Resources Beneath Rapidly Urbanising Cities – Implications and Priorities for Water Supply Management.
Galvin, R 2015, How many interviews are enough? Do qualitative interviews in building energy consumption research produce reliable knowledge?
General Statistics Office of Viet Nam 2015, Population and Employment.
GFDRR 2011, Vulnerability: Risk reduction and adaptation to Climate Change Viet Nam.
Goddard, W 2001, Research methodology: an introduction, Juta, Lansdowne.
Gupta, P 2002, Statistical Methods, Sultan Chand & Sons, New Delhi.
Hakim, C 2000, Research Design: Successful Designs for Social and Economic Research, Routledge, London.
Harris, N, Pisa, L, Talioaga, S, & Vezeau, T 2009, Hospitals Going Green: A Holistic View of the Issue and the Critical Role of the Nurse Leader.
Hassan, M, Ahmed, A, Rahman, A & Biswas, T 2008, Pattern of medical waste management: existing scenario in Dhaka City, Bangladesh.
Hinkel, E 2011, Handbook of Research in Second Language Teaching and Learning, Volume II, Routledge, New York.
Hoang, T 2009, Study on status and factors related to medical waste management in General Central hospital in Thai Nguyen province, Thai Nguyen University of Medicine and Pharmacy, Bangkok.
Hoffman, E 2001, Postgraduate research guidelines, Triangle Technikon, Vanderbijlpark.
Hoyle, R 2002, Research methods in social relations, Wadsworth, Fort Worth.
Hutchins, D & White, S 2008, Coming round to recycling.
International Conference on the Development of Biomedical Engineering, 2015, 5th International Conference on Biomedical Engineering in Viet Nam, McMillan, London.
International Conference on the Development of Biomedical Engineering 2015.
Jiang, S 2006, The practical implementation of the 3R’s of sustainable waste management in the Norfolk and Norwich university hospital.
Johnke, B 2000, Emissions from Waste Incineration.
Joint Annual Health Review 2014, Strengthening prevention and control of non-communication diseases.
Kagonji, S & Manyele, S 2011, Analysis of measured medical waste generation rate in Tanzania District hospitals using statistical methods.
Ketlogetswe, C 2004, Improved combustion process in medical waste incinerators for rural.
Kojima, M & Michida, E 2013, International trade in recyclable and hazardous waste in Asia, Edward Elgar, Cheltenham.
Kudoma, B 2013, An Evaluation of Clinical Waste Management in Garobone city Council Healthcare Facilities, University of South Africa, Cape Town.
Le, K 2014, Dioxin Contamination in Viet Nam: Emissions from industries and levels in the environment.
Lee, B 2002, Analysis of the recycling potential of medical plastic wastes.
Lye, L 2010, Sustainability matters: Environmental management in Asia, World Scientific, Singapore.
Manyele, S & Lyasenga, T 2010, Factor affecting medical waste management in low-level health facilities in Tanzania.
Mato, R & Kassenga, M. 1997, Critical review of industrial and medical waste practices in Dar es Salaam city.
Mbongwe, B, Mmereki, T & Magashula, A 2008, ‘Healthcare waste management: Current practices in selected healthcare facilities’, Waste Management, vol. 8, no. 1, pp. 226-233
McDermott-Levy R 2011, The nurse’s role on green teams: an environmental health opportunity.
Mejia, E & Sattler, B 2009, Starting a Health Care System Green Team.
Ministry of Health 2007, Directive No 43/2007/QD-BYT.
Ministry of Health 2013, Health Statistic Yearbook 2012, McMillan, Hanoi.
MONRE 2011, The report on national environment – solid waste.
Moreira, A & Gunther W 2013, ‘Assessment of medical waste management and a primary health care centre in Sao Paulo, Brazil’, Journal of Waste Management, vol. 33, no. 6, pp. 162-167.
Newswire, P 2016, Doctors, Dentists and Nurses-Most trusted professionals to give advices, according to Harris Poll U.S. Adults.
Nguyen, T 2005, Solid Waste Management in Viet Nam.
Nichols, A, Grose, J, Bennallick, M & Richardson, J 2013, ‘Sustainable healthcare waste management: a qualitative investigation of its feasibility within a county in the south west of England,’ Journal of Infection Prevention, vol. 14, no. 2, pp. 60.
Nihon, K 1999, The State of the environment in Asia, Institute of Southeast Asian Studies, Singapore.
Nurse and Midwifery Council 2008, The Code: Professional standards of practice and behavior for nurses and midwives.
Ozbek, M & Sanin, F 2004, A study of the dental solid waste produced in a school of dentistry in Turkey.
Pariatamby, A & Tanaka, M 2013, Municipal solid waste management in Asia and the Pacific Islands: Challenges and strategic solutions, McGrow Hill, New Delhi.
Pham, A & Eggleston, B 2015, Diabetes Prevalence and Risk Factors Amongst Vietnamese Adults: Finding from Community-Based Screening Programs.
Pruss, A, Giroult, E & Rushbrook, P 1999, Safe Management of Wastes from Health-Care Activities.
Public Health Association of HoChiMinh City 2014, Annual Conference against cancer in HCMC.
Raworth, K. 2012, A safe and just space for humanity. Can we live within the doughnut?, Oxfam Discussion Papers.
Richardson, J, Burton, R, Sewell, R, Spreckelsen, T & Montgomery, P 2012,
Docosahexaenoic Acid for Reading, Cognition and Behaviour in Children Aged 7–9 Years: A Randomized, Controlled Trial.
Sakaguchi, K 2001, ‘Hospital Waste Management in Japan and Viet Nam’, Japan Society of Waste Management Experts, vol. 37, no.1, pp. 2-3.
Salkin, F 2004, Review of health impacts from microbial hazards in health care wastes.
Sattler, B & Hall, K 2008, Healthy Choices: Transforming Our Hospitals into Environmentally Healthy and Safe Places.
Shah, F & Ranghieri, F 2012, A workbook on planning for urban resilience in the face of disasters: Adapting experiences from Viet Nam’s cities to other cities, World Bank Washington.
Steffen, W 2013, The Great Acceleration: Towards Sustainability or Collapse? University of Cambridge, Unpublished.
Strohschen, G 2009, Handbook of blended shore education: Adult program development and delivery, Springer, New York.
Sustainable Development Commission 2010, Sustainable development: The key to tackling health inequalities. p.9
ThanhnienNEWS 2015, Vietnam hospital fined for dumping 63 tons of untreated medical waste.
Tudor T.L. et.al., 2008, Realising resource efficiency in the management of healthcare waste from the Cornwall National Health Service (NHS) in the UK.
UNCED, 1992, United Nations Conference on Environment and Development Rio de Janerio, Brazil, 3 to 14 June 1992: Agenda 21. p41
Van, S 2015, A Different Face of War: Memories of a Medical Service Corps Officer in Viet Nam, Wiley, Hoboken. Viet Nam Laws.
Vietnamnet 2016, Bach Mai hospital recycling medical waste.
VIHEMA 2015a, Workshop on the draft of Guidance on medical waste management for health care facilities generating less of medical waste.
VIHEMA 2015b, Medical Waste Management is still a burden to hospitals.
VIHEMA 2015c, The harm of mercury and its sources in the medical area.
Visvanathan, C 2006, Medical waste management issue in Asia.
WHO 2002, Injection Safety.
WHO 2014, Safe management of wastes from health-care activities.
Wilburn, S 2007, Overview and Summary: Environmental Health: Important Choices for a Greener World.