Introduction
Diabetes is a highly prevalent and costly chronic disease affecting millions of people. It requires ongoing clinical and self-management. For this reason, the education of patients on self-management practices is an integral part of the disease intervention. While traditionally, clinicians instructed their patients about various health and disorder-related issues during face-to-face meetings, nowadays, education can be administered via distinct telehealth technologies. Considering that over time telehealth has proved to be efficient and cost-effective and was associated with greater patient satisfaction in multiple studies focused on its use in the monitoring of chronic diseases, it may become useful in diabetes self-management education (DSME) as well.
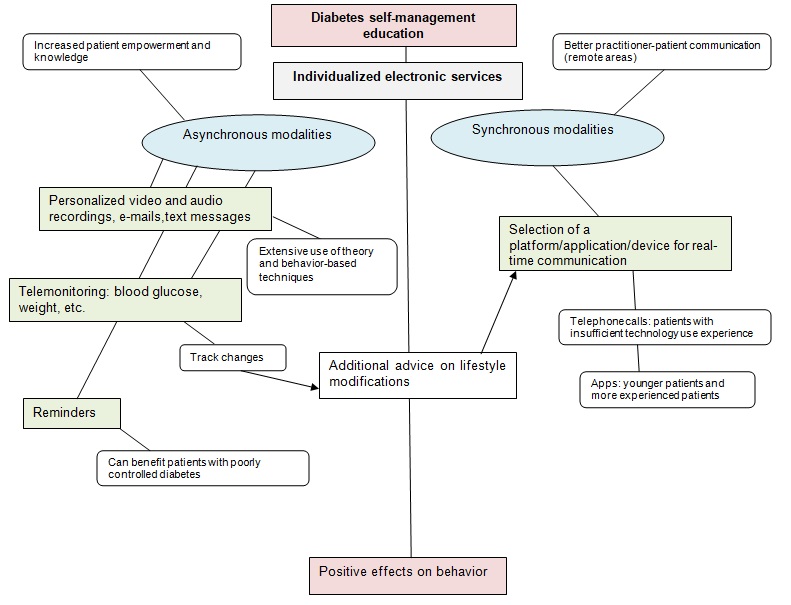
In the given paper, a study on the telehealth technology use in DSME, written by Fitzner, Heckinger, Tulas, Specker, and McKoy (2014), will be reviewed in Précis. In the following section, a mind map designed based on the findings of the study will be discussed. The mind map outlining some possible ways and methods of telehealth implementation for addressing the selected issue will be presented in the appendix.
Précis
In their study, Fitzner et al. (2014) evaluated the total sample of 25 systematic literature reviews and meta-analyses, as well as 22 additional studies on diabetes and related interventions and technologies. The researchers aimed to identify if the use of telemedicine in DSME is associated with cost-effectiveness, better access to services, improved clinical outcomes, and individual behaviors. The findings obtained by Fitzner et al. (2014) indicate that telehealth can be regarded as effective for the improvement of the health of patients with diabetes, yet it remains uncertain if remotely provided education for patients of different age is associated with consistent effects in improved clinical, behavioral, and economic results. The literature analysis conducted Fitzner et al. (2014) is important because it outlines the major strengths and weaknesses of telehealth in DSME and helps identify barriers to its effective use and, in this way, can assist in designing better strategies for the technology use, i.e., individualization of electronic service offerings, real-time vs. self-paced interventions, its combination with offline face-to-face communication, etc.
Mind Map Discussion
Fitzner et al. (2014) emphasize that to increase the efficacy and cost-effectiveness of telemedicine, individual factors of patients must be considered. These factors may include health risk factors, previous technology experience, age, overall accessibility to both face-to-face and online services, etc. It is also important to consider that the use of technology might not be cost-effective or efficient in all cases and among all patients with diabetes, e.g., individuals with advanced stages of the disease. Thus, to address all the factors well, a healthcare practitioner should utilize a multimodal approach and select the best education technology and method based on patients’ capabilities, needs, and interests.
According to Toh, Pawlovich, and Grzybowski (2016), telehealth modalities can be either synchronous or asynchronous. As it is shown in the appendix to the paper, the former ones may include real-time online, phone, video, and audio communication. The latter ones include audio and video recordings, images, e-mails, etc. − all the sources to which a patient may refer anytime. It is possible to say that asynchronous modalities are associated with greater patient empowerment as they imply an extensive use of theory, which usually results in greater behavioral improvement according to Fitzner et al. (2014). At the same time, synchronous modalities help develop better relationships with a patient. Thus, their use is especially important when patients live in remote areas and do not have an opportunity to establish trustful relationships with their health providers offline. It is worth noticing that when a communication medium is familiar to a patient, he or she may be “more willing to divulge sensitive information than they would in a face-to-face encounter” (Toh et al., 2016, p. 962).
By combining different modalities, practitioners will be able to provide necessary adherence and psychological support, remotely monitor self-management results, and give feedback (Hanlon et al., 2017). Although the selected methods of communication and education may slightly differ for every patient, healthcare providers must design a standard communication, monitoring, and feedback loop, which would be applicable to every case. For instance, the following loop is suggested in the mind map: telemonitoring − track changes − additional advice on lifestyle modifications through a selected synchronous modality. Through the systematization of the education process, it will be possible to achieve higher work efficiency and minimize the risk of excess workload.
Conclusion
Fitzner et al. (2014) suggested that telehealth technologies, including such mobile technologies as text messaging and applications, have the potential to offer tremendous utility. It can lead to better short-term clinical and behavioral outcomes in patients. However, individual factors must be considered to implement technology more efficiently. Thus, the strategy suggested in the paper implies a multimodal approach to telehealth diabetes education because it presumably allows healthcare providers to meet the individual needs of patients and address specific factors and barriers to clinical intervention more effectively.
It is expected that telehealth will be utilized more widely in the future. Based on this, it is possible to conclude that as an adjunct to the conventional face-to-face patient meetings and education sessions, telehealth can be an increasingly effective tool, especially when a patient lives in a remote area. If a practitioner can select a modality adequately, education by using the given technology may result in better patient outcomes and satisfaction.
Appendix
Mind Map
References
Fitzner, K. K., Heckinger, E., Tulas, K. M., Specker, J., & McKoy, J. (2014). Telehealth technologies: Changing the way we deliver efficacious and cost-effective diabetes self- management education. Journal of Health Care for the Poor and Underserved, 25(4), 1853-1897.
Hanlon, P., Daines, L., Campbell, C., McKinstry, B., Weller, D., & Pinnock, H. (2017). Telehealth interventions to support self-management of long-term conditions: A systematic metareview of diabetes, heart failure, asthma, chronic obstructive pulmonary disease, and cancer. Journal of Medical Internet Research, 19(5), 1.
Toh, N., Pawlovich, J., & Grzybowski, S. (2016). Telehealth and patient-doctor relationships in rural and remote communities. Canadian Family Physician, 62(12), 961–963.