Abstract
The National Health Service was established in 1948 with the primary goal of providing a universal healthcare to all the residents of the United Kingdom. The government was committed to finding a solution to the problem of rising cost of medication at a time when the country was reeling from the effects of the Second World War.
The NHS has achieved its mandate over the years because it has remained dynamic. Under the joint management of government and the market, the NHS has undergone significant evolution and reforms as it seeks to offer residents of the country quality healthcare services. The institution now spends more money on research and training of its workforce. NHS was significantly affected by the Brexit. The fate of doctors, nurses, and clinical officers who are not citizens of the country is still unclear.
The institution also benefited from medical research and other sponsorships from European organisations. These benefits may be lost as the country seeks to define its political, economic, and social future as a non-member to the EU. As the country was still in the process of dealing with Brexit, the COVID-19 pandemic struck.
It happened at the worst time for NHS because the management was still restructuring to ensure that it could deal with the negative effect of leaving the European Union. The government has increased its expenditure on NHS to support research, protect frontline workers in the healthcare sector, and to improve facilities to accommodate more patients and the demand continues to increase.
Introduction
Background Statement
The National Health Service, popularly known as the NHS, is a public healthcare system in the United Kingdom. It was launched in 1948 after years of intense lobbying in an effort to have a system that would make healthcare affordable to every resident of the kingdom. For several decades prior to the Second World War, the political class and stakeholders in the healthcare sector had struggled to develop a healthcare system that would address concerns of all citizens, but there was no consensus (Ryder et al., 2020).
When a new administration took over immediately after the war, the need for a universal healthcare became more evident for the political class. The prime minister tasked Aneurin Bevan to develop a people-sensitive healthcare system for all residents of the United Kingdom. The country was still recovering from the events of the war, and healthcare was one of the basic needs for everyone (Ryder et al., 2018).
He helped in creation of NHS with the principle goal of providing universal healthcare for all residents of the country irrespective of their financial capacity. The fundamental principle of the NHS was to have universal coverage for everyone, maintain a cost-effective healthcare system, and manage costly specialised services in a way that do not burden the general population.
The NHS is one of the most effective models of healthcare systems in the world that many countries have used as the benchmark to improve individual systems. However, Gorsky (2008) notes that it also has some major weaknesses those different administrations have tried to address. Chantelle et al. (2017) explains that the system has been viewed as being regard, over-centralised, and lacking in incentives for improvement and innovation.
Different administrations have tried to introduce reforms meant to improve its service delivery without over-burdening tax payers in the country. In most of the cases, introducing such reforms has been challenging because of extreme political differences. In this paper, the researcher seeks to investigate how the NHS has evolved and reformed under the joint management of the government and the market, as well as the impact of Brexit and the current COVID-19 pandemic.
Rationale for the Study
The NHS has continued to play a critical role in enhancing the provision of healthcare services in the country for all. There has been a need to make changes to this organisation to improve its efficiency in provision of health services. This study will help to evaluate how NHS has evolved, over the years under the joint management of the government and the market.
It will investigate forces that have contributed to such changes. The study will also analyse the impact that the Brexit and COVID-19 has had in promoting these reforms. Through the study, it will be possible to determine whether these reforms have helped to positively transform service delivery at NHS.
Research Questions
The healthcare sector has played a crucial role in managing the COVID-19 pandemic in the country. This study will help in understanding how reforms have helped in making the NHS effective in managing such emergencies and general healthcare needs. The following are the research questions that guided this investigation:
- How has the NHS evolved and reformed under the joint management of the government and the market?
- What is the impact of Brexit (economic, social, and political factors) on the reforms and performance of NHS?
- What is the impact of COVID-19 (such an emergency) on the reforms and performance of NHS?
- How can the management model of NHS influence the medical systems of other countries?
Literature Review
The previous chapter has provided detailed background information about the topic under investigation. In this chapter, the focus is to review existing literature about the issue. It is necessary to review what other scholars have found out about how the National Health Service has evolved and reformed under the joint management of the government and the market. This chapter looks at the process that led to the establishment of the NHS, success that it has experienced over the years, challenges that it has faced, and reforms that it has gone through since its establishment.
The Establishment of NHS and Its Mandate
The United Kingdom, like many other European Nations, was massively affected by the events of the Second World War. According to Walker, Hanna and Raisborough (2020), prior to the war, the political class failed to agree on the best model for universal healthcare. However, the devastation of the war demonstrated the need to have a universal healthcare that could meet needs of all residents of the United Kingdom.
The country’s economy was significantly affected, and many people were struggling to meet their basic needs (Phillips et al., 2019). The government felt the need to provide for its soldiers and the general population who were affected in different ways during the war. When the Labour Part, under the leadership of Clement Attlee won the 1945 elections, one of the promises that it set out to accomplish was to provide universal healthcare for all the residents of the country (Guest et al., 2017). The system that existed then was unfavourable to the unemployed.
When Aneurin Bevan was appointed to be the Minister of Health, one of his primary assignments was to develop a healthcare system that would cover everyone in the country. He came up with the concept of National Health Service that was adopted in England and Wales in 1946, Scotland in 1947, and Northern Ireland in 1947 (Hers, 2017).
At the time of its launch, it had three primary principles: to meet everyone’s need, be free at the point of delivery, and based not on the ability to pay but clinical needs (Sanderson, Allen and Osipovic, 2017). It meant that residents of the United Kingdom could walk into any healthcare facility and get medical assistance without being demanded to pay for it.
The government understood the fact that healthcare is a basic need and that it would be immoral to deny a person such services because of their limited financial capacity. According to Clarke and Youngstein (2017), these principles were deeply rooted in the British culture and the majority was proud of a system that enabled everyone to have access to medical services.
When NHS was first introduced to the country, Aneurin Bevan emphasised the need to ensure that it would be accessible to everyone residing in the United Kingdom irrespective of their nationality. As the Minister of Health, he argued that screening patients who need such services on the basis of their nationality would create discord as some British citizens who are unable to prove their citizenry would be denied services when they need them the most.
During the launch, he said, “unwise as well as mean to withhold the free service from the visitor to Britain. How do we distinguish a visitor from anybody else? Are British citizens to carry means of identification everywhere to prove that they are not visitors?” (Regmiab and Mudyarabikwa, 2020, p. 280). It is important to note that some reforms have been introduced in the recent past to screen patients to determine their eligibility. The screening became necessary become of the increasing burden on the country’s healthcare system because of the increasing cases of illegal immigration in the country.
Success of the NHS
The National Health Service has played a critical role in making medical services universally available to all residents of the United Kingdom. According to Worthington et al. (2017), since its establishment, it has made a massive impact on lives of many people, especially in the low income families who may not afford the high cost of health services. One of the biggest successes of NHS is its ability to have a system that provides comprehensive health insurance (excluding dental and optical care) to the citizens without burdening citizens.
Prior to its development, one of the biggest challenges that hindered the creation of such a medical cover was the concern that it would burden taxpayers. However, it has been proven that NHS does not burden the ministry of health financially. Checks and balances have been put in place to ensure that services are offered in an affordable way.
NHS has been essential in protecting people from facing financial burden when ill. According to Addicott (2016), since its introduction, healthcare services in the country have been relatively cheaper than in other European nations. In fact, the model has been borrowed by other countries in Europe and North America because of its effectiveness.
Watson (2017) explains that the productivity of the NHS has been going up over the years and from January 2018 to January 2019; it registered a 3% growth across in terms of its productivity. The institution has continued to provide quality healthcare to its targeted population over the past seven decades despite the numerous economic, social, and political challenges that it has been facing.
The success of the NHS is partly attributed to its continued commitment to recruiting highly qualified staff and ensuring that they go through training regularly. Currently, it is considered the largest employer in the United Kingdom, and the fifth-largest in the world. The large workforce is meant to ensure that residents of the country can have access to the services they need without delay, including those who are in need of emergency services (Thacoor, Bosch and Akhavani, 2019).
The team includes doctors, nurses, clinical officers, and other non-medical staff that work as a unit to ensure that quality service is delivered to those who are in need.
The outbreak of the COVID-19 in the United Kingdom in the early 2020 has demonstrated the unique capacity of NHS to deliver quality services to residents of the United Kingdom. When the pandemic struck, the country, just like many other nations around the world, was not prepared to deal with the problem. The team at NHS lacked proper information about the disease, but it soon became apparent that it was a highly contagious and dangerous disease (Wong et al., 2018).
Doctors, nurses, clinical officers, and all the other staff members have continued to put their lives at risk to fight this pandemic for over the last seven months. Many of them have sacrificed their lives and those of their loved ones just to ensure that the rest of the population is safe. The country has lost many people to this disease, but the team has done an excellent job in protecting many more from a problem that many lacked information about.
Challenges that NHS Has Faced and Reforms Following the Joint Management of the Government and the Market
The National Health Services has demonstrated its commitment to the provision of quality healthcare to all residents of the United Kingdom. However, the institutions have faced numerous challenges as it seeks to provide its services to the people. Some of these challenges have made it impossible to introduce some of the reforms meant to improve its service delivery. Pimpin et al. (2018) explain that the initial model of NHS that was introduced in the country was very effective.
However, just like other models in various other sectors, changes in the environment make it necessary to introduce changes and reforms at various stages of implementation. Some of these challenges have made it difficult for the institution to deliver its mandate to the people and to make necessary reforms.
The NHS has been facing the problem of political interference ever since it was created. Soon after it was launched, the Labour government that was responsible for its creation was replaced by the Conservative government under the leadership of Winston Churchill. It immediately introduced prescription charges, which was a major controversy at the time (Pillai, Navas and Walker, 2018). When the new regulation was introduced, a section of the society did not see a proper justification for it.
Many stakeholders felt that it was a deliberate attempt by the current administration to dilute the major achievement that the previous government had made. Kerr et al. (2019) explain that since then, many other changes have been introduced by the political class, including strict screening procedure to determine one’s eligibility, something that goes against the initial spirit of NHS. Some policies have been introduced by the politicians to attract voters without taking into consideration their viability and ability to address pressing needs.
The institution has also faced financial challenges worth discussing. According to Lombaerts et al. (2020), 98.8% of the revenue that this institution uses to facilitate its operations comes from the government. The remaining 1.2% is generated from the small amounts of fees that it charges its patients.
It means that whenever there is a delay in government funding, the operations of the institution can be paralysed. When it was launched in 1948, it had a budget of £437 million, but that amount has increased to £ 122.5 billion in 2017 (Stokes et al. 2018). The government’s expenditure on health at that time was 11.2% of the GDP, but that has since increased to 29.7% in 2017 (Williams and Dickinson, 2016). The statistics show that government’s expenditure on healthcare services, as a percentage of its GDP, is increasing considerable.
Stakeholders have been struggling to find ways of maintaining a universal healthcare for all in the country, but in a way that do not overburden taxpayers. One of the main concerns is that the cost of care has been on the rise consistently, which is putting pressure on the NHS. According to Robotham et al. (2016), introducing more charges is not an option that the institution can consider because it would go against its principles. As such, it is necessary to find alternative ways of addressing the problem.
Some stakeholders have blamed the institution for lacking proper incentives to motivate individual hospitals to improve their performance. In an effort to reduce the waiting time for patients, especially those that need medical emergencies, some healthcare centres have introduced unique strategies to cut improve their efficiency in service delivery (Khan et al., 2017).
Others have invested in research and hiring highly qualified staff to ensure that they deliver the best services to their clients. The problem that they face is that once their reputation is known to public, they start experiencing an influx of patients. Many people would opt to visit such institutions because they are guaranteed speedy quality services. The NHS lacks mechanism that can enable it to monitor changes in demand at different institutions that would warrant an increase in their budget. Such institutions will continue receiving the same amount of money as before.
In some few cases, the budget may be increased, but not in a way that reflects the demand. As the trend continues, the facilities and staff at such institutions will be overwhelmed (Osipovič et al., 2020). Quality of services delivered will go down and the reputation will be eroded. The lack of a proper mechanism of incentivising individual institutions for excellent performance is partly responsible for the increase in waiting time at the institution.
Although the institution is managed at the national level, there is need to have a local approach. The management requires a system that would enable it to understand the demand at individual institutions and how to manage it in a way that does not strain healthcare facilities.
The joint management of government and the market has promoted various reforms at the institution. System automation was one of the new changes that were introduced under these reforms. The desire to improve efficiency forced stakeholders to introduce electronic system of managing patients’ data (Jackson et al., 2018).
It was meant to ensure that doctors at different facilities could have historical records of patients’ treatments. The mechanism was meant to avoid repeating tests or making other medical mistakes because of misdiagnosis pr lack of data (Ali et al., 2017). The institution has also been working in collaboration with private institutions and international organisations to support research and development in the field of medicine.
Research Methodology
The previous chapter has provided a comprehensive review of literature based on the data collected from secondary sources. As Williams et al. (2020) explain, reviewing the literature helps to gather background information about a given field of study. A researcher is able to understand what other scholars have found out and gaps that exist in these studies. In this chapter, the focus is to discuss the method that was used to collect and process data.
Data sources and collection method and the analysis approach are discussed in this study. The researcher also discusses reliability and validity issues, ethical considerations, and challenges that the researcher faced when collecting data for the research.
Data Sources and Collection Method
When planning to collect data, one of the first steps that one needs to take is to define data sources. According to Rimmer and Wattar (2020), a researcher can use primary sources, secondary sources, or both to inform the study. It is always advisable to use both to have a comprehensive understanding of the research topic. Secondary data helps in understanding the current state of knowledge in a given field and existing knowledge gaps, while primary data provides information meant to address the gaps or possible conflicts in the existing knowledge.
It was desirable to use both sources of data, but the limited time and restricted interaction brought about by measures meant to curb the spread of COVID-19 made it impossible to use primary data. Finding the right individuals to provide reliable knowledge was not easy within such a short period that the study had to be completed. As such, the researcher relied on secondary data only.
Secondary data was obtained from books, journal articles, and reliable online sources. Journal articles were considered scholarly sources and they formed the bulk of sources that were used in the study. They were obtained from various databases such as Cochrane Database of Systematic Reviews, MedlinePlus, Medline, EMBASE, and PsycINFO.
Books were also obtained from online libraries because of the difficulty in accessing the school and community libraries during this period of corona virus outbreak. To help collect recent information, especially about COVID-19 and its impact on NHS, the researcher relied on some online sources, including reputable newspapers to collect current data. Key phrases such as NHS reforms, impact of COVID-19 on NHS, impact of Brexit on NHS, and NHS’s joint management were used to have access to the needed data.
Analysis of the Collected Data
When data has been collected from various sources, the next step that a researcher has to take is to conduct a comprehensive analysis. The analysis helps in answering specific research questions. When selecting an appropriate research design, Newton and Thompson (2017) advises that one has to consider the primary goal of the study and specific research questions that have to be answered. The design should allow the researcher to effectively answer all the critical questions in the study.
The nature of data to be analysed also defined the design that one should use. In this case, the researcher relied purely on secondary data. As such, the researcher considered descriptive research design as the most appropriate approach that would facilitate comprehensive analysis of the collected data. Ehrenfeld (2017) explains that descriptive statistics helps to answers questions such as what, when, and how of a given phenomenon. These were the questions that this study focused on addressing, as evident in chapter one of this paper.
This approach makes it possible to use case studies in the study. Although descriptive research design mainly uses quantitative research, it also allows the use of qualitative research. These are the characteristics that made it be viewed as the most desirable design for this study.
Reliability and Validity Issues
This report may play a significant role in informing policies that may influence the future of NHS. As such, issues of validity and reliability had to be taken seriously in this research. Greenberg et al. (2020) emphasise the need to ensure that data collected from a given source is factual and not misleading. The researcher ensured validity and reliability of data by using scholarly sources. Using of peer-reviewed journals was seen as one of the best ways of enhancing reliability and validity of data.
The researcher also made sure that books used had been reviewed favourably by various experts in the health sector. Using online data from government press release and publications from various reputable organisations such as the NHS itself, the Department of Health and Social Care, World Health Organisation, and such other similar organisations was important.
These deliberate steps were taken to ensure that the secondary data used could provide reliable information for the study. It was specifically important to take those steps because the study wholly relied on secondary data, as there was no time to collect primary data from a sample.
Ethical Considerations
When conducting an academic research, it is always essential to take into consideration ethical concerns. According to Asaria, Doran and Cookson (2018), one of the most important ethical concerns is the need to protect participants in the study. It helps in ensuring that they are not victimised in case their opinion is different from that of the majority. However, it is important to note that primary data was not used in this investigation. As such, the need to protect the identity of the participants did not exist.
The biggest ethical consideration that the researcher observed was the need to avoid all forms of plagiarism. Given the fact that the report relied entirely on secondary data, the researcher ensured that information was properly referenced using Harvard referencing style. It was also necessary to ensure that the paper was completed within the provided timeline.
Challenges Faced When Collecting Data
The researcher faced a few challenges worth discussing at this stage of the study. The limited time available for the research made it impossible to collect primary data. It meant that the researcher had to rely wholly on secondary data collected from books and journal articles. The fact that the school library is currently not open for use was another challenge.
It would have been desirable to have access to the library to have a wide collection of sources. This challenge was overcome by having access to online data sources. It is also necessary to note that some databases required subscription. However, this was not a major challenge as it was easy to have access to various other free online databases.
Findings
The National Health Service continues to play a critical role in ensuring that every resident of the United Kingdom has access to affordable quality healthcare irrespective of their financial capacity. It is important to understand how the NHS has evolved and reformed under the joint management of the government and the market, as well as the impact of Brexit and COVID-19 pandemic.
The previous chapter provided a detailed explanation of the method that was used to collect data. In this chapter, the focus is to present findings that were made in the investigation. This section will focus on responding to each of the questions presented above to ensure that the aim of the study is achieved.
How has the NHS evolved and reformed under the joint management of the government and the market?
The first question focused on determining how the NHS has evolved and reformed under the joint management of the government and the market. According to Holmes et al. (2018), this institution has gone through a major transformation since it was established over seven decades ago. One of the main areas of change that has been witnessed is in research.
When it was founded, the primary mandate was to ensure that it makes available quality healthcare services to all the residents when they need it. It has continued to discharge this duty diligently. However, the management has realised that the best way of maintaining quality services is to support research. According to Vallejo‐Torres, García‐Lorenso and Serrano‐Aguilar (2017), new diseases are emerging and some of those that existed before are mutating because of environmental factors.
The ability of the health sector to deal with these complications depends on the amount and quality of research that it conducts. The NHS has been supporting doctors and nurses who are interested in investigating how to improve the quality of healthcare services in the country. Barros and Braun (2017) observe that this support does not just come in the form of sponsorship but also granting these medical experts time away from the workstation so that they can concentrate in their studies. These initiatives have helped in improving service delivery at various healthcare institutions in the country. Managing chronic conditions has become relatively easier and cheaper because of the introduction of new strategies.
Expenditure is another area of change that has been witnessed at the NHS over the years. When the institution started its operation in 1948, the budget for the healthcare sector was about 11% that of the country’s GDP. However, the percentage has been increasing consistently and in 2016, it was estimated that the same ministry currently accounts for about 29.7% of the country’s GDP (Sallis et al., 2016). It means that it takes about one third of the country’s gross domestic product. The trend is partly attributed to the fact that people are currently living longer than before (Rimmer and Wattar, 2020).
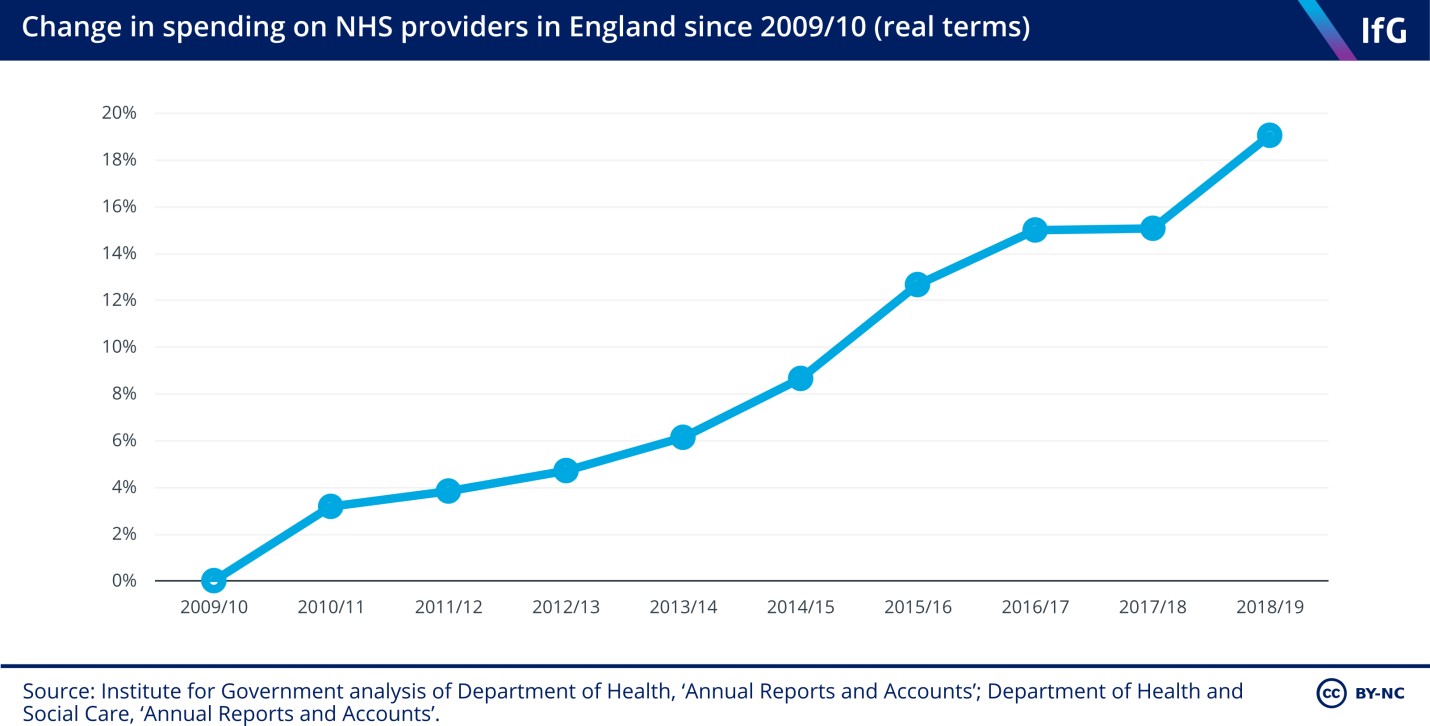
As they age, they become vulnerable to various chronic diseases, which make it necessary for them to receive regular medication. Figure 1 below shows the change in spending at the NHS in England over a period of 10 years, from 2009 to 2019. The statistics shows a consistent yearly increase in the expenses of NHS providers in the country over this period. Within this period, the expense at NHS has increased by 20%, which translates to about 2% increase every year.
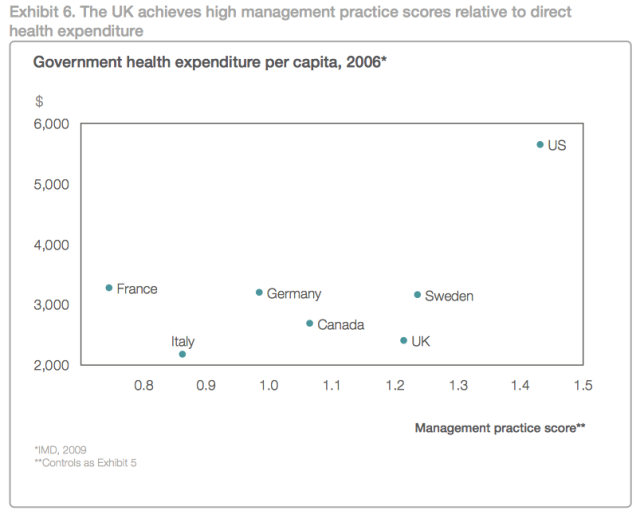
It was necessary to conduct a comparative analysis to understand how other countries have been spending on the healthcare sector. The above statistics show that the NHS and the Department of Health and Social Care in general have had a major increase in their total expenditure. Figure 2 below shows a comparative analysis of the expenditure in the health sector per capita in different European countries and the United States and management practices score.
The goal is to determine how much each of these countries spend and how it affects their efficiency in service delivery. The statistics show that the United States spends more than twice what the United Kingdom spends (in terms of the per capita) as shown in the figure below. In Europe, France, Germany, and Sweden spend more per capita than the United Kingdom. Canada also spends more than the United Kingdom. In fact, of all the countries that were included in this comparative analysis, it is Italy that spends less than the United Kingdom.
The analysis then compared the management practices score for each of these countries. It would be expected that the more a country spends, the better it will be in providing quality services to its people. However, the statistics show that higher spending does not necessarily reflect improved service delivery. The United States, which has the highest amount of expenditure per capita, has the best management practices score than all the countries that were included in the analysis.
Second in the list is Sweden, which spends more than the United Kingdom. However, the trend changes when the performance of this country is compared with that of Germany, Canada, and France. These three countries spend more than the United Kingdom, but their performance in management practices is poorer than this country. In fact, France’s performance was the worst in all the countries analysed although it has the second highest per capita expenditure on health.
Italy, which had the least expenditure, registered the second-worst performance in management practices. It is therefore true that the United Kingdom has developed unique ways of using its limited resources to achieve greater performance. The NHS is credited for such improved performance of the country’s healthcare sector (Davis, 2020). It has integrated technology and enhanced skills of its employees to ensure that people can get the best services in all hospitals in the country.
When evaluating the evolution and reforms at NHS, one of the areas that have to be taken into consideration is the quality of service delivery. The Department of Health and Social Care, through the NHS, has been keen on improving the overall quality of healthcare that people receive when they visit different hospitals across the country. As Bick et al. (2017) observes, there are different parameters that can be used to assess the quality of healthcare that hospitals offer.
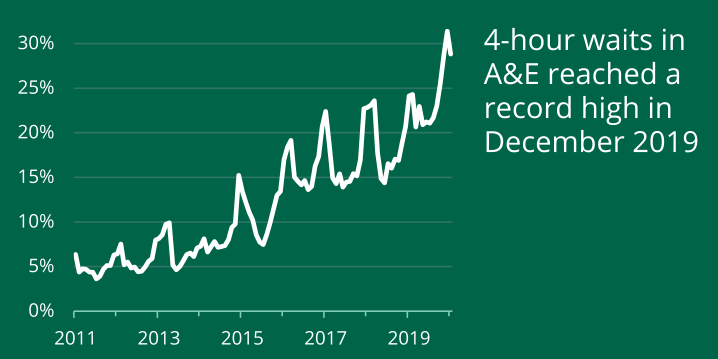
Although the most important one is the ability of the medical staff to accurately diagnose the condition of a patient and provide effective intervention, one can use other parameters to assess the performance. One of these parameters is the waiting time. When a patient visits a healthcare facility, they expect to get the service they need within the shortest time possible because of the pain and discomfort they may be experiencing (Holmes et al., 2018). In accident and emergency (A&E) section, time that it takes to deliver the service may be the difference between life and death.
At the emergency department, the medical staffs are often under pressure to attend all the patients within the shortest time possible. However, figure 3 below shows a worrying trend. From 2011 to 2019, there has been a consistent increase in the waiting time for patients who need emergency services. The statistics show that in 2011, only 5% of patients in need of emergency services spent about 4 hours as they waited to be served. This number has since increased to about 30% (Osipovič et al., 2020).
If nothing is done to address the issue, the trend may continue, and soon it will be normal for people to wait for four or more hours before they can get the services they need. As Greenberg et al. (2020) explain it may be true that patients wait for long but end up getting quality services at these facilities. However, the problem is that when dealing with cases of emergency, patients do not have time to wait for that long. They need to be attended to within the shortest period possible.
The primary reason why the waiting time has been on the rise at the accident and emergency department is that the staff is overwhelmed. The number of people seeking these services has been increasing at a greater rate than the NHS has been able to increase its staff. Most of them are struggling to meet the growing demand. The NHS has been keen on increasing the size of its staff over the years to meet the growing demand.
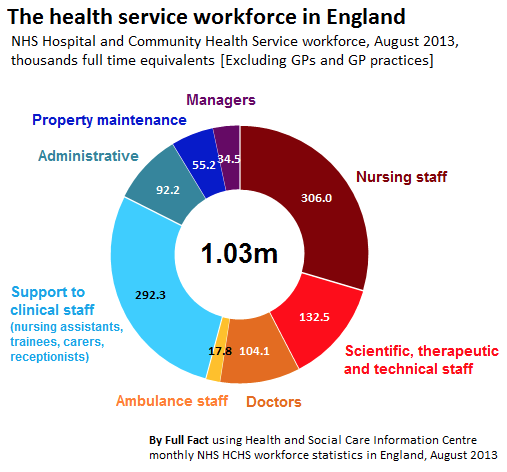
It employees people in different cadre, as shown in figure 4 below. The highest number of these employees is the nursing staff at about 306,000 people. Support staff to clinical staff, which includes receptionists, nursing assistants, and trainees account for about 292,300 people. The scientific, technical, and therapeutic staff accounts for about 132,500. The institution currently has 104,100 doctors serving at different institutions (Osipovič et al., 2020). Others include administrators, property maintenance unit, ambulance staff, and managers. The data was taken in 2013, and the numbers have changes since then. However, it shows the composition of employees at this institution.
What is the impact of Brexit (economic, social, and political factors) on the reforms and performance of NHS?
When evaluating the evolution and reforms at the NHS, it was considered necessary to look at how the Brexit has affected the process. The United Kingdom voted to leave the European Union in one of the most divisive elections in the country’s modern history (Greenberg et al., 2020). There were concerns about the effect of the Brexit on various sectors of the economy. Williams et al., 2020) conducted a research to determine the view of stakeholders in the healthcare sector about the effect of this decision on the country’s healthcare system.
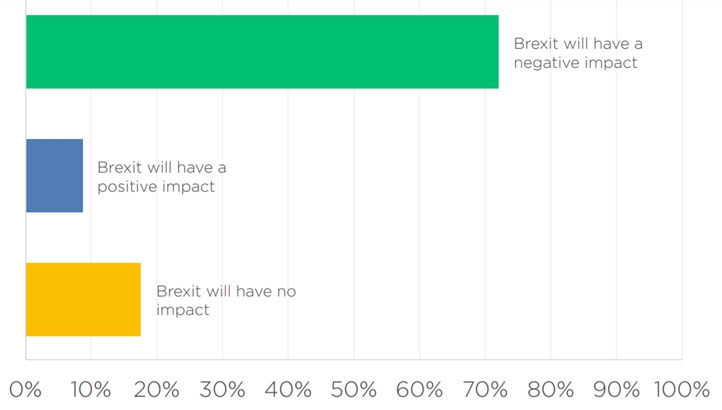
They were asked to state whether they believe the decision of the UK to leave the European Union will have any effect on the country’s healthcare sector. As shown in figure 5 below, an overwhelming majority of the respondents (72% of the total sample) believe that it would have a negative impact. Another 19% of the respondents stated that there will be a neutral impact on the healthcare sector. Only 9% of the total sample population was optimistic, stating that it would have a positive impact. It means that the general population believes that the decision of the country to leave the union will negatively affect the country.
The statistics above show that the majority of the stakeholders in the country feel that NHS will be affected negatively when the country finally leaves the European Union. It was necessary to go further with the investigation to understand why these participants had this view. Lombaerts et al. (2020) explains that the NHS has for many years been integrated with the other major EU organisations that if there is no proper arrangement for the exit, the consequences may be dire.
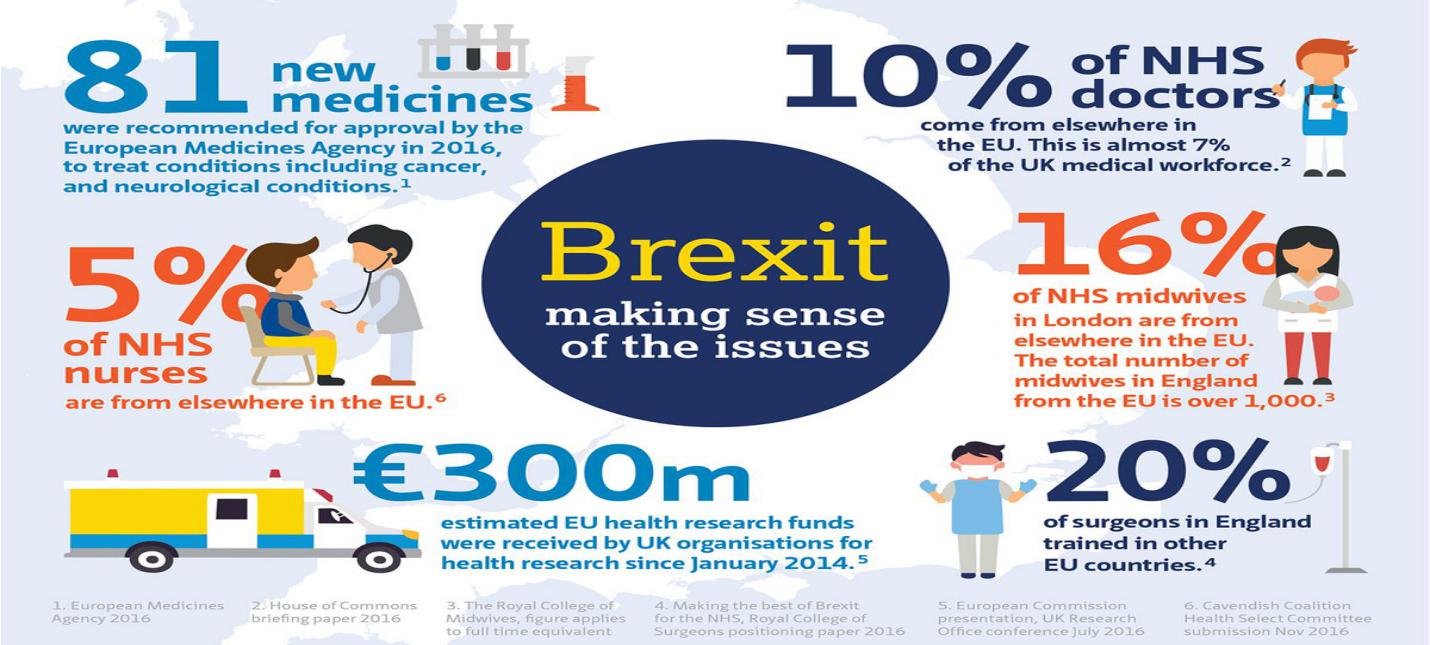
As shown in figure 6 below, 10% of doctors currently working at the NHS are from other countries within the EU (Greenberg et al., 2020). Their fate is yet to be known under the new arrangement that is expected. In case these doctors have to go back to their home country because of lack of agreement between the government and the EU, then the healthcare sector will be affected significantly.
The statistics show that 16% midwives in London are from other countries within the European Union. Another 20% of the surgeons in the country are from other EU nations and so are 5% of all nurses working across the country (Lombaerts et al., 2020). These statistics show how much the country relies on EU for its staff.
It is not clear what will happen to these individuals who play a critical role to ensure that residents of the United Kingdom have access to quality healthcare. It is also evident that the United Kingdom received over € 300 million from the EU to support medical research in 2014 (Greenberg et al., 2020). In 2016, the country received 81 new medicines that had been approved by EU to help in fighting different medical conditions.
What is the impact of COVID-19 (such an emergency) on the reforms and performance of NHS?
COVID-19 has had a major impact on the NHS and the general population in the United Kingdom. Like many other countries around the world, the country was not prepared to deal with such a major pandemic. The disease, which started in China, spread very quickly to European nations and to the rest of the world. The first case to be reported in the country was that of two family members who tested positive of the virus on January 31, 2020 (Rimmer and Wattar, 2020).
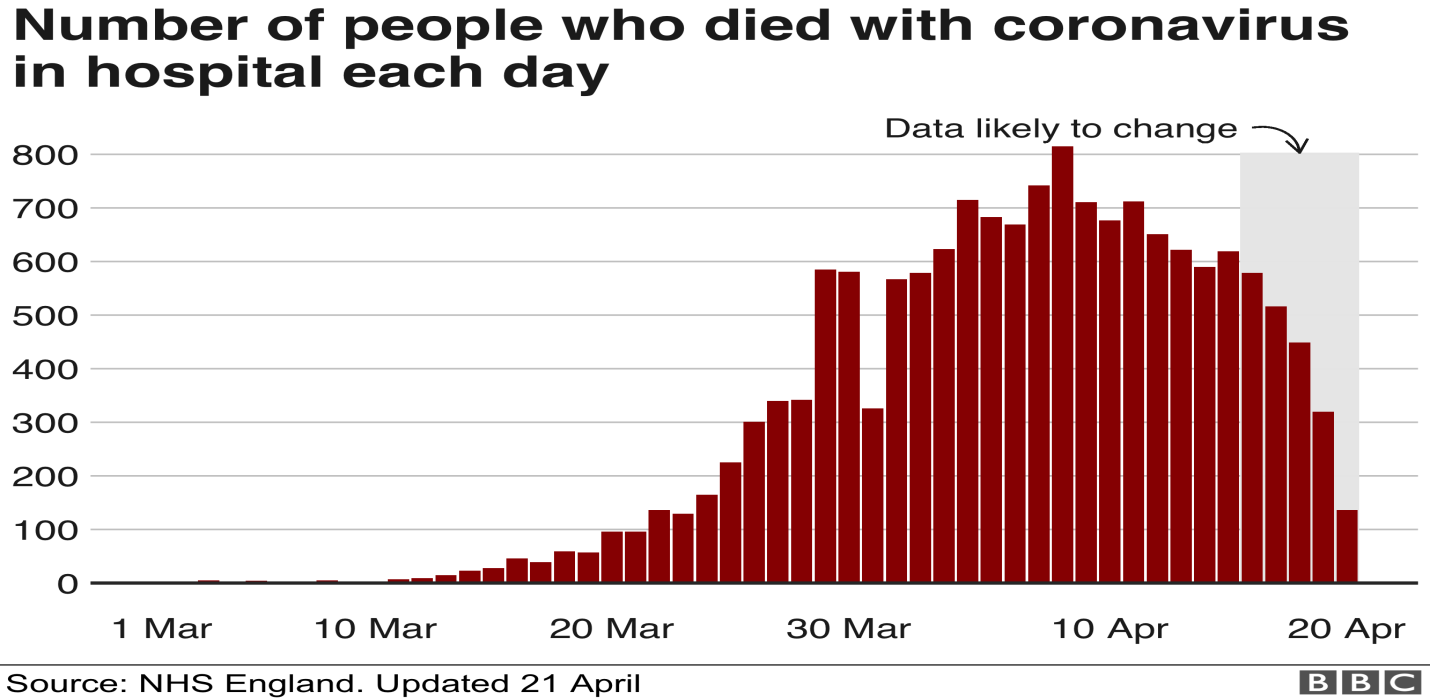
These cases started to rise rapidly in the late February. By March, the country had started recording deaths from the virus as shown in figure 7 below. From March 10 to March 30, the number of those who died of the virus started increasing rapidly it peaked on April 10, when over 800 people died of the virus on a single day. The number of deaths has since been going down as stakeholders struggle to find ways of dealing with it.
The outbreak of COVID-19 pandemic has had a devastating impact on the NHS. As Li et al. (2020) reports, the pandemic has overstretched the workforce and facilities in the country’s healthcare sector. The problem with this disease is that the condition of patients deteriorates very fast and many would need oxygen or ventilators.
The condition would require intensive care unit (ICU) services very rapidly. Fatalities are very high among patients with underlying conditions (Kerr et al., 2019). Doctors and nurses working with NHS could not cope with the massive demand for their services. It is important to note that those in the private sector were overwhelmed as well. The government has been forced to postpone most of its developmental and non-essential projects to focus on the fight against COVID-19.
The problem was worsened by the high rate at which the medical staff would be infected with this contagious virus as they worked to save lives of patients (Xiang et al. (2020). Many doctors, nurses, clinical officers, and non-medical staff working in hospitals have sacrificed their lives to protect residents of the United Kingdom from the pandemic. The government has realised the significance of increasing its expenditure on the health sector, especially in the fields of research and training to equip the NHS staff with skills needed to deal with such problems.
Discussion
The analysis of data in the previous chapter shows that the National Health Service Has evolved over the years since its inception in 1948. There has been a deliberate effort to ensure that the institution meets healthcare needs of residents of the United Kingdom. Under the joint management of the government and the market, there has been an effort to improve efficiency of service delivery at the NHS. Automation of the patient data is one of the major reforms that have been introduced over the recent past (Kerr et al., 2019).
When it started its operations and for decades that followed the institution relied on the use of paper files to manage patients’ data. The problem with this approach is that it was time-consuming to store and retrieve information of patients. One had to have access to the physical file to obtain the needed information. Sharing of data among practitioners was also a major challenge.
The problem was solved when the digital platform of managing data was introduced. The platform shortened the time that it took to record, store, retrieve, and share patients’ data. It reduced the waiting time for patients revisiting hospitals for check-ups or follow-up treatments (Ryder et al., 2020).
It was also easy for the NHS, at the national level, to collect and process data to understand emerging trends, such as the emerging diseases and the common health complications. Although there have been cases where patients’ data have been shared with large pharmaceutical organisations against the law, the new system has helped improve the performance of many institutions of healthcare in the country.
The Brexit has had a massive impact on the country socio-economic and political landscape. In the health sector, there have been concerns that the process may affect the ability of the NHS to deliver its mandate effectively. Many foreign nationals from European Union nations have been working in the country and benefiting from the universal healthcare coverage under the NHS. The problem is that their fate remains unclear even after the deal was finalised.
There is the fear that people who come from countries that do not have a special healthcare insurance arrangement with the United Kingdom may be considered illegible to receive the benefits (Kerr et al., 2019). There is also the group holding European Health Insurance Card who have been benefiting from the services of NHS. Many of them who are not citizens of the United Kingdom do not understand how they can continue getting health services they need under this cover in the new era within the country.
The United Kingdom was benefiting economically from the pooling of resources for research within the European Union. The decision to exit the union means that NHS will have to sponsor all its medical research fully, which is expected to cause economic strain. From the political angle, decision-making might have become easier than before for the institution because it no longer has to consult other countries.
However, the ease with which doctors, nurses, and clinical officers could come to the country might be affected. Davis (2020) explains that the about 10% of the medical staff in the country are from other countries within the EU. Their fate in the country is still unclear as the stakeholders could not make the decision when the country finally left the union. The world was hit with the corona virus and most of these decisions were deferred.
The United Kingdom was not prepared for a major pandemic as COVID-19, just like many other countries around the world. However, it had to act fast to ensure that the lives of its citizens are protected. NHS staff has been at the frontline, putting their lives at risk to ensure that they protect residents of the United Kingdom from the pandemic (Yao and Chen, 2020). The first case was reported on January 31, but the country became overwhelmed with the virus by March.
As it spread quickly in the society, the number of those who needed hospitalisation started to increase rapidly. The medical staff was constantly exposed to the virus as they handled COVID-19 patients. A significant number of them of them contracted the disease, with some losing their lives while others were lucky enough to recover. By mid-April, there was a crisis at NHS as the country continued to record over 800 deaths daily from the virus (Germain, 2020). The same unfortunate trend was witnessed in the neighbouring countries.
The Department of Health and Social Care now appreciates the significance of equipping the NHS to enable it deal with such unpredictable pandemics. Although the number of new cases and deaths from the virus has dropped significantly, the country is still struggling to regain normalcy.
One of the major reforms introduced specifically because of the COVID-19 pandemic is the approach towards managing infectious diseases. For a long time, the country has been using reactionary strategies where it responds to occurrences of major outbreaks. However, the NHS now understands that this problem could have been mitigated if only the country took a proactive approach (Lipscomb et al., 2020). If the issue were investigated as soon as it was detected in China, and measures taken to reduce its impact, then many people would not have lost their lives as was the case.
The government has realised that its expenses in the health sector have to be reviewed upwards. During this pandemic, it became evident that the country was over-relying on importation of important medical supplies and equipment from the United States and China. Some of the reagents needed for testing patients suspected to be infected with corona virus had to come from China.
That country also needed the same reagents to test their people. It meant that they took care of their needs first before they could consider meeting the global demand (Xiang et al., 2020). These events demonstrated that there was a need to redefine the approach that the country took to offer services to its people. For many years, the NHS has pride itself as an institution that offers the best medical services in the world. However, these events have revealed that having highly qualified doctors, nurses, and clinical officers is not enough.
It is equally be important for a country to be self-reliant when it comes to the production of equipment and consumables in the healthcare sector. The country cannot afford to continue relying on other nations for these important services because when disasters such as COVID-19 strike, many of these countries will take care of their needs first before considering helping other countries.
How the Management Model of NHS can Influence the Medical Systems of Other Countries
The National Health Service in the United Kingdom has gone through various reforms over the years since its establishment. Many countries in Europe, North America, Asia, and parts of Africa have borrowed concepts of this model as a way of improving their service delivery. One of the countries that have borrowed some of the concepts of NHS is the United States.
According to Lipscomb et al. (2020), for many years, the United States had struggled to find the best way of offering its citizens universal healthcare irrespective of an individual’s financial capacity. The political class could not agree on the best model that the country could embrace. On the one hand, a section of the policy-makers felt that introducing such a health cover for everyone would burden American taxpayers. Individuals and companies would be forced to pay more in health insurance cover.
The increased payment is to ensure that those who are not working or the retired would also get covered. The opponents of this model opposed it as being unnecessarily repressive. On the other hand, those who supported it felt that it was immoral for people to be denied healthcare primarily because they lack the ability to pay. They argued that it was the responsibility of the government to ensure that all its citizens have access to affordable healthcare irrespective of their financial capacity.
Reaching a consensus was not easy because of these deeply rooted conflicts in opinion. When President Barack Obama took over the presidency of the country in 2008, one of his primary goals was to introduce a healthcare system that would ensure everyone is covered. Despite facing a massive opposition from Republicans, the president was able to convince the Congress to pass the Affordable Care Act, which is popularly known as the Obamacare.
Most of the principles of the Affordable Care Act are a reflection of the NHS concepts in its revised form. In both cases, there is a deliberate attempt by the government to ensure that everyone can have access to the medical services when they need them. Some European nations have also borrowed this model to define their healthcare system.
Conclusion
The National Health Service was established with the mandate of ensuring that all residents of the United Kingdom can have access to quality healthcare services irrespective of their capacity to pay. The institution was established soon after the Second World War when the country was still reeling from years of destruction and limited economic activities.
The study shows that despite its obvious benefits to citizens of this country, a section of the society still believes that it is over-burdening the working class. These conflicting beliefs have led to a scenario where every administration wants to make changes that would reflect views of their constituents.
Winston Churchill came to power for the second time when the previous administration had just succeeded in introducing the NHS. His government was the first to introduce changes to the original draft to make it a requirement for people to pay for subscription drugs or at least part of it. It was seen as a way of making the service affordable to everyone but in a way that does not overburden taxpayers. Since then, NHS has evolved and reformed to reflect emerging changes in the global healthcare sector.
Brexit was seen by a section of the society as a way of reducing reliance on the European Union. However, data collected from secondary sources show that the NHS has been affected negatively by the decision of the UK to leave the union. The country benefited from the joint medical research that was conducted by various EU organisations.
Member countries pooled their resources to sponsor such researches, which benefited their citizens. Under the current arrangements, the United Kingdom can no longer benefit from such initiatives. It means that the country will be expected to sponsor all its medical researches without any form of assistance from the EU. The fate of the medical staff, especially the highly qualified doctors and nurses who come from other EU countries, is still unclear.
In case they have to go back to their home countries because of the new political, economic, and social restructuring in the country, then the NHS will lose valuable human resource. The outbreak of COVID-19 also had a major impact on the institution. It came when it was least expected and it overstretched resources at different facilities around the country. The NHS is yet to recover from the massive shock it got from the pandemic.
Reference List
Addicott, R. (2016) ‘Challenges of commissioning and contracting for integrated care in the National Health Service (NHS) in England’, Australian Journal of Primary Health, 22(1), pp. 50-54.
Ali A. et al. (2017) ‘Factors associated with 30-day readmission after primary total hip arthroplasty: analysis of 514 455 procedures in the UK National Health Service’, JAMA Surgery, 152(12), pp. 5-13.
Asaria, M., Doran, T. and Cookson, R. (2018) ‘The costs of inequality: whole-population modelling study of lifetime inpatient hospital costs in the English National Health Service by level of neighbourhood deprivation’, British Medical Journal, 70(10), pp. 1-7.
Barros, P. and Braun, G. (2017) ‘Upcoding in a National Health Service: the evidence from Portugal’, Health Economics, 26(5), pp. 600-618.
Bick, D. et al. (2017) ‘Maternity care for trafficked women: survivor experiences and clinicians’ perspectives in the United Kingdom’s National Health Service’, Plos One, 12(11), pp. 6-9.
Chantelle, B. et al. (2017) ‘Rasch analysis of the antimicrobial self-assessment toolkit for National Health Service (NHS) Trusts,’ Journal of Antimicrobial Chemotherapy, 72(2), pp. 604-61.
Clarke, R. and Youngstein, T. (2017) ‘Cyberattack on Britain’s National Health Service: a wake-up call for modern medicine’, The New England Journal of Medicine, 377(5), pp. 409-411.
Davis, J. (2020) ‘EU‐UK Brexit negotiations, covid‐19 and key roles for economists’, Euro Choices, 19(1), 3-7.
Ehrenfeld, J. (2017) ‘Wanna cry, cybersecurity and health information technology: a time to act’, Journal of Medical Systems, 41(104), pp. 1-2.
Germain, S. (2020) ‘Will COVID-19 marks the end of an Egalitarian National Health Service’, European Journal of Risk Regulation, 11(2), pp. 358-365.
Gorsky, M. (2008) ‘The British National Health Service 1948–2008: a review of the historiography’, Social History of Medicine, 21(3), pp. 437-460.
Greenberg, N. et al. (2020) ‘How might the NHS protect the mental health of health-care workers after the COVID-19 crises’, Lancet Psychiatry, 7(9), pp. 733-734.
Guest, J. et al. (2017) ‘Health economic burden that different wound types impose on the UK’s National Health Service’, International Wound Journal, 14(2), pp. 322-330.
Hers, N. (2017) ‘Addressing National Health Service (NHS) priorities: medtech innovation briefings’, International Journal of Technology Assessment in Health Care’, 33(1), pp. 2-7.
Holmes, D. et al. (2018) ‘Use of programme budgeting and marginal analysis to set priorities for local NHS dental services: learning from the north east of England’, Journal of Public Health, 40(4), pp. 578-585.
Jackson, R. et al. (2018) ‘CogStack: experiences of deploying integrated information retrieval and extraction services in a large National Health Service Foundation Trust hospital’, BMC Medical Informatics and Decision Making, 18(47), pp. 8-11.
Kerr, M. et al. (2019) ‘The cost of diabetic foot ulcers and amputations to the National Health Service in England’, Special Issue on Health Economics, 36(8), pp. 995-1002.
Khan, N. et al. (2017) ‘Advanced diagnostic genetic testing in inherited retinal disease: experience from a single tertiary referral centre in the UK National Health Service’, International Journal of Genetics, 91(1), pp. 38-45.
Li, W. et al. (2020) ‘Progression of mental health services during the COVID-19 outbreak in China’, International Journal of Biological Sciences, 16(10), pp. 1732-1738.
Lipscomb, D. et al. (2020) ‘Diabetic foot ulceration in COVID‐19 lockdown: cause for concern or unexpected benefit?’ Diabetic Medicine, 37(8) pp. 1409-1410.
Lombaerts, C. et al. (2020) ‘Homeopathy in the NHS (National Health Service): diluted but active’, Homeopathy, 109(1), pp. 1-28.
Newton, J. and Thompson, K. (2017) ‘NHS health check: national evaluation findings and implications’, Canadian Medical Association Journal, 189(4), pp. 172-177.
Ohannessian, R., Duong, T. and Odone, A. (2020) ‘Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action’, JMIR Public Health Surveillance, 6(2), pp. 1-7.
Osipovič, D. et al. (2020) ‘The regulation of competition and procurement in the National Health Service 2015–2018: enduring hierarchical control and the limits of juridification’, Health Economics, Policy and Law, 15(3), pp. 308-324.
Phillips, C. et al. (2019) ‘Adherence to antibiotic guidelines and reported penicillin allergy: pooled cohort data on prescribing and allergy documentation from two English National Health Service (NHS) trusts’, British Journal of Management, 9(2), pp. 1-7.
Pillai, D., Navas, S. and Walker, C. (2018) ‘You were rubbish!’ the challenges in developing a simulation programme for multi-cultural doctors new to the national health service (NHS)’, British Medical Journal, 4(2), pp. 17-20.
Pimpin, L., et al. (2018) ‘Estimating the costs of air pollution to the National Health Service and social care: an assessment and forecast up to 2035’, Plos Medicine, 15(7), pp. 1-6.
Regmiab, K. and Mudyarabikwa, O. (2020) ‘A systematic review of the factors – barriers and enablers: affecting the implementation of clinical commissioning policy to reduce health inequalities in the National Health Service (NHS), UK’, Public Health, 186(1), pp. 271-282.
Rimmer, M. and Wattar, A. (2020) ‘Provision of obstetrics and gynaecology services during the COVID‐19 pandemic: a survey of junior doctors in the UK National Health Service’, British Journal of Obstetrics and Gynaecology, 127(9), pp. 1123-1128.
Robotham, J. et al. (2016) ‘Cost-effectiveness of national mandatory screening of all admissions to English National Health Service hospitals for meticillin-resistant Staphylococcus aureus: a mathematical modelling study’, Journal of Infectious Diseases, 16(3), pp. 348-356.
Ryder, R. et al. (2018) ‘U.K. First National Health Service (NHS) endobarrier (EB) service-outcomes in first 38 patients to reach six months after device explants’, American Diabetes Association, 67(1), pp. 7-18.
Ryder, R. et al. (2020) ‘76-OR: UK 1st National Health Service (NHS) endo barrier (EB) service for uncontrolled disability: 2-Year outcomes for all 62 treated patients’, American Diabetes Association, 69(1), pp. 1-8.
Sallis, A. et al. (2016) ‘The effectiveness of an enhanced invitation letter on uptake of National Health Service Health checks in primary care: a pragmatic quasi-randomised controlled trial’, BMC Family Practice, 17(35), pp. 1-11.
Sanderson, M., Allen, P. and Osipovic, D. (2017) ‘The regulation of competition in the National Health Service (NHS): what difference has the Health and Social Care Act 2012 made?’, Health Economics, Policy and Law, 12(1), pp. 1-19.
Stokes, E., et al. (2018) ‘Accurate costs of blood transfusion: a microcosting of administering blood products in the United Kingdom National Health Service’, Transfusion, 58(4), pp. 846-853.
Thacoor, A., Bosch, P. and Akhavani, M. (2019) ‘Surgical management of cosmetic surgery tourism-related complications: current trends and cost analysis study of the financial impact on the UK National Health Service (NHS)’, Aesthetic Surgery Journal, 39(7), pp. 786-791.
Vallejo‐Torres, L., García‐Lorenso, B. and Serrano‐Aguilar, P. (2017) ‘Estimating a cost‐effectiveness threshold for the Spanish NHS’, Health Economics, 27(4), pp. 746-761.
Walker, C., Hanna, P. and Raisborough, J. (2020) ‘Representations of the National Health Service (NHS) in UK print media’, Health Promotion International, 44(1), pp. 1-5.
Watson, N. (2017) ‘Support and its impact on the lived experiences of African Caribbean nurses as students and practitioners in the British National Health Service (NHS)’, Journal of Healthcare Communications, 2(4), pp. 39-44.
Williams, I., and Dickinson, H. (2016) ‘Going it alone or playing to the crowd: a critique of individual budgets and the personalisation of health care in the English National Health Service’, Australian Journal of Public Administration, 75(2), pp.149-158.
Williams, M. et al. (2020) ‘Service users’ experiences of contacting NHS patient medicines helpline services: a qualitative study’, British Medical Journal, 10(6), pp. 5-9.
Wong, D. et al. (2018) ‘Cancelled operations: a 7-day cohort study of planned adult inpatient surgery in 245 UK National Health Service hospitals’, British Journal of Anaesthesia, 121(4), pp. 730-738.
Worthington, J. et al. (2017) ‘A randomised controlled trial to determine the clinical and cost effectiveness of thulium laser transurethral vaporesection of the prostate versus transurethral resection of the prostate (TURP) in the National Health Service (NHS)-the UNBLOCS trial: a study protocol for a randomised controlled trial’, BioMed Central, 179(18), pp. 1-11.
Xiang, T. et al. (2020) ‘The COVID-19 outbreak and psychiatric hospitals in China: managing challenges through mental health service reform’, International Journal of Biological Sciences, 16(10), pp. 1741-1744.
Yao, H. and Chen, J. (2020) ‘Rethinking online mental health services in China during the COVID-19 epidemic’, Asian Journal of Psychiatry, 50(1), 1-17.