Introduction
Buprenorphrine is replacing methadone in detoxification of opiate addiction. Buprenorphrine suppresses withdrawal symptoms in opiate addiction. This study was conducted on 200 opiate addiction patients at the Sunrise Detoxification Center. The effectiveness of buprenorphrine in reducing pulse, sweating, anxiety, tremor, and nausea among other withdrawal symptoms was evaluated.
Background
Opiate abuse and dependence is overwhelming with 8% of American population abusing opiates.
More children aged below 13 years are currently abusing opiates but majority of opiate abusers are 13-30 years old. Opiate abuse mainly commences at 10 to 13 years of age and addiction heightens in late teens
Some opiates commonly abused in the U.S. include: morphine, heroin and hydrocodone. The opiates are either sniffed, smoked or injected into the body. These drugs cause dizziness and a relaxing effect.
Misconceptions on opiate abuse
Sniffing and smoking does not lead to addiction. Opiates are cool and users of the drugs become cool too. Opiates are good stress relievers. If you can control it and use it once in a while, then the drug is good
Unfortunately, the misconceptions lead to serious addiction.
Addiction to opiates becomes difficult to overcome with side effects such as nausea, vomiting, stress, coma and even death occurring.
Treatment of opiate addictionWithdrawing from opiates leads to symptoms such as shaking sweating, and nausea among others.
There are psychological and conventional treatment programs.
Psychological treatment focuses on empowering and motivating the mental and psychological components of the patient.
This reduces the possibility of reverting to opiate abuse.
Psychological healing however requires integrating medication to address physical withdrawal symptoms.
Rapid opiate detoxification (ROD)
It does not offer instant and immediate healing to opiate addicts.
ROD causes renal and heart failure with death occurring in some cases.
Withdrawal symptoms are felt after 24 hours and within 6 months, up to 80% of patients revert to opiate abuse.
Agonist medicines therefore remain more promising in opiate detoxification as they reduce fatalities while relieving withdrawal symptoms effectively.
The traditional detoxification approaches lead to gradual detoxification thus avoiding withdrawal symptoms eventually leading to independence from opiates.
Buprenorphrine
Buprenorphrine is a synthetic opioid (phenanthrene) widely used in opiate detoxification to minimize withdrawal symptoms.
Although buprenorphrine has a few side effects, these are not as strong as those of natural opioids.
It is more competitive in binding to brain cells than natural opioids and relieves severe stress in opiate withdrawal.
Excess buprenorphrine does not result into dizziness since agonist effects reach a plateau.
Buprenorphrine has a long half life (up to 72 hours) hence it reduces withdrawal symptoms for long.
Patients can self administer buprenorphrine.
Buprenorphrine is administered:
- Intravenously- rapid distribution and slow elimination, rapid ease of withdrawal symptoms.
- Intramuscularly –slower distribution rate
- Sublingually – cumbersome to administer and slow rate of absorption.
Buprenorphrine is quite new and not extensively tested hence not recommended for pregnant women.
Not recommended for people who are not addicted to opiates since it is a mild opiate.
Methadone
The earliest (over 30 years) drug in treatment of opiate addiction.
It effectively treats addiction withdrawal symptoms for opiate drugs only.
Methadone has a shorter half-life than buprenorphrine.
It is clinically safe and has no physiological damage hence it is an effective alternative to buprenorphrine.
Although methadone and buprenorphrine cause some addiction, patients undergoing treatment still carry their normal lives well.
Program Evaluation of Opiate Addicts
- Ho: There is a correlation between the patient effects observed and the detoxification procedures used at the Sunrise detoxification centre.
- H1 : There is no correlation between the patient effects observed and the opiate detoxification procedures used at the Sunrise detoxification centre.
Research structure: collection of data from patients’ records, evaluation of the data, making records of the collected data and interpretation of the results.
A random sample of 200 charts from Sunrise Detoxification Center.
Data analysis was conducted using SPSS software.
Study assumptions
- There is no marked difference in opiate resistance related to the age and gender of patients
- The effects of buprenorphrine are similar in each patient
- There is no difference in patient outcomes related to years of abuse
Findings
Age of opiate addicts:
76% of all subjects were 18-46 years old while 23% of all subjects were 46-65 years of age.
Most opiate addicts were below 40 years thus opiate addiction is a problem among the young.
Mean age for opiate addicts was 23.4 years.
Half of the addicts (100) were 18 -32 years old which is the critical age when most opiate abusers seek medical help.
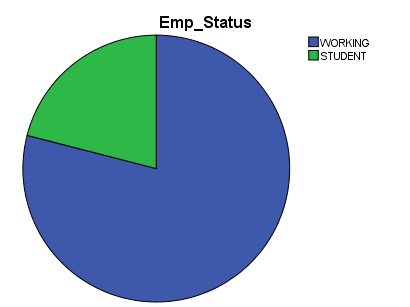
Employment status of patients
Most patients (79%) were working citizens and a small percentage (21%) were students.
Pulse rates
80% of patients had pulse rates above normal (100-120) prior to administration of buprenorphrine.
56% of these had developed normal pulse rates of below 80beats/min 30 minutes after induction.
Mean pulse rates fell gradually afterwards until the rates normalized in two hours.
Sweating and chills
Patients had severe sweating before buprenorphrine administration.
There was marked decrease in sweating in 88% of the patients 30 minutes after buprenorphrine administration.
There was a significant drop in the number of patients suffering from severe sweating as time progressed to 4 hours
Restlessness
Prior to administration of buprenorphrine, 72%of the patients were unable to sit well even for a few seconds and had extraneous limb movement.
58% of the patients were able to sit well within 30 minutes after treatment.
At 2 hours after induction, restlessness had improved tremendously
At four hours, the relaxing and easing effects of the drug had stabilized.
Pupil size
Buprenorphrine reduced the number of patients with severe pupil dilation so that only the rim of the iris was visible and increased the number of patients with normal pupil size.
64% of the patients had normal pupil size after within 2 hours of induction and 22% had near normal pupils.
Only 8% of all subjects had dilated pupils 2 hours after buprenorphrine administration.
Four hours after the first dose was induced, the effects of buprenorphrine were still evident.
Bone/joint aches
Before induction of buprenorphrine, patients had mild to severe and diffuse joint pain.
30 minutes after first induction, 51% of the patients had mild pains while 38% did not feel any pain.
63% of patients were free of joint pain at 2 hours after induction.
Running nose and tear development
The number of patients with constant running noses reduced from 79% to 6% after 2 hours of buprenorphrine administration.
Nose stiffness and rhinorrhea had reduced remarkably after buprenorphrine administration.
Effects of buprenorphrine of the GIT
Within 30 minutes of induction, episodes of vomiting and multiple diarrhea reduced from 140 to 25.
At 2 hours, the efficacy of the drug remained stable with a slight decrease in nausea and multiple diarrhea cases.
At 4 hours, the effects of buprenorphrine had stabilized and were similar to those recorded at 2 hours.
Anxiety and irritability
The number of patients who were obviously irritable and severely irritable reduced from 165 to 51 thirty minutes after drug induction.
4 hours after initial induction, 58% of the patients were not irritable and 30% were slightly irritable.
Only 12% (26 patients) were still obviously or extremely irritable 4 hours after the initial dose.
Yawning
Yawning behavior reduced at 30 minutes after the first dose.
The number of patients who did not yawn increased from 27% to 57% after the 4 hours of treatment.
On a scale of 1-8, buprenorphrine scored a mean of 5.64 thus its performance was satisfactory.
Hypothesis Testing
Chi-Square analysis was used to determine the effectiveness of the chosen hypothesis.
There was a 5% chance that the observed readings were incorrect.
However, even if there was a variation of 5% in the data due to errors the alternative hypothesis would still hold true. It is for this reason that the hypothesis: There is a correlation between the patient effects observed and the detoxification procedures used at the Sunrise Detoxification Centre, was accepted.
Conclusion
Buprenorphrine treats withdrawal symptoms in opiates addiction effectively.
The study supported that buprenorphrine: decreases pulse rate, reduces sweating, eases pupil dilation, eases and prevents joint pain, normalizes running nose, eases nausea and vomiting, reduces anxiety, eases tremors, and prevents unnecessary yawning
Buprenorphrine has a long half-life (25 hours – 72 hours) and therefore it can ease opiate withdrawal symptoms for a relatively long period.
Suboxone is the main buprenorphrine drug used in the center and it is effective in small doses (8mg/patient) with only a small percentage (2%) requiring 16mg.
To avoid relapse of symptoms, the taper process should be done under the guidance of a healthcare professional.
The taper process should be slow to allow the body to adjust to falling levels of opioids.
The study supported that buprenorphrine is effective in treating withdrawal symptoms that are associated with opiate addiction.
References
Bolourian, S. (2010). Buprenorphrine: a guide for readers. New Jersey, NJ: Dane Publishing.
Courtwright, D. (2001). Dark paradise: a history of opiate addiction in America. New York, NY: Harvard University Press.
Cowan, A. (1995). Buprenorphrine: combating drug abuse with a unique opioid. Michigan, MI: Wiley-Liss.
Doweiko, H. (2006). Concepts of chemical dependency. California, CA: Cengage Learning.
Hales, R. (2008). Study guide to substance abuse treatment. Arlington, VA: American Psychiatric Publishing.
Junig, J. (2009). User’s guide to suboxone: taking buprenorphrine for opiate dependence. Wisconsin, WI: Terminally Unique Publishing.
Kleber, H. (2008). The American Psychiatric Publishing textbook of substance abuse treatment. Arlington, VA: American Psychiatric Publishing.
Langrod, J. (2007). The substance abuse handbook. Philadelphia, PA: Lippincott Williams and Wilkins.
Marquete, P. (2002). Buprenorphrine therapy of opiate addiction. New Jersey, NJ: Humana Press.
Millman, R. (1997). Substance abuse: a comprehensive textbook. Philadelphia, PA: Lippincott Williams and Wilkins.
Renner, J. (2009). Handbook of office-based buprenorphrine treatment of opioid dependence. Arlington, VA: American Psychiatric Publishing.
Silk, K. (2009). Cambridge textbook of effective treatments in psychiatry. New York, NY: Cambridge University Press.
Strain, E. (2005). The treatment of opioid dependence. Maryland, MD: John Hopkins University Press.
Thakkar, V. (2008). Addiction. New York, NY: Infobase Publishers.
World Health Organization. (2009). Guidelines for the psychosocially assisted pharmacological treatment of opioid dependence. Geneva: World Health Organization.