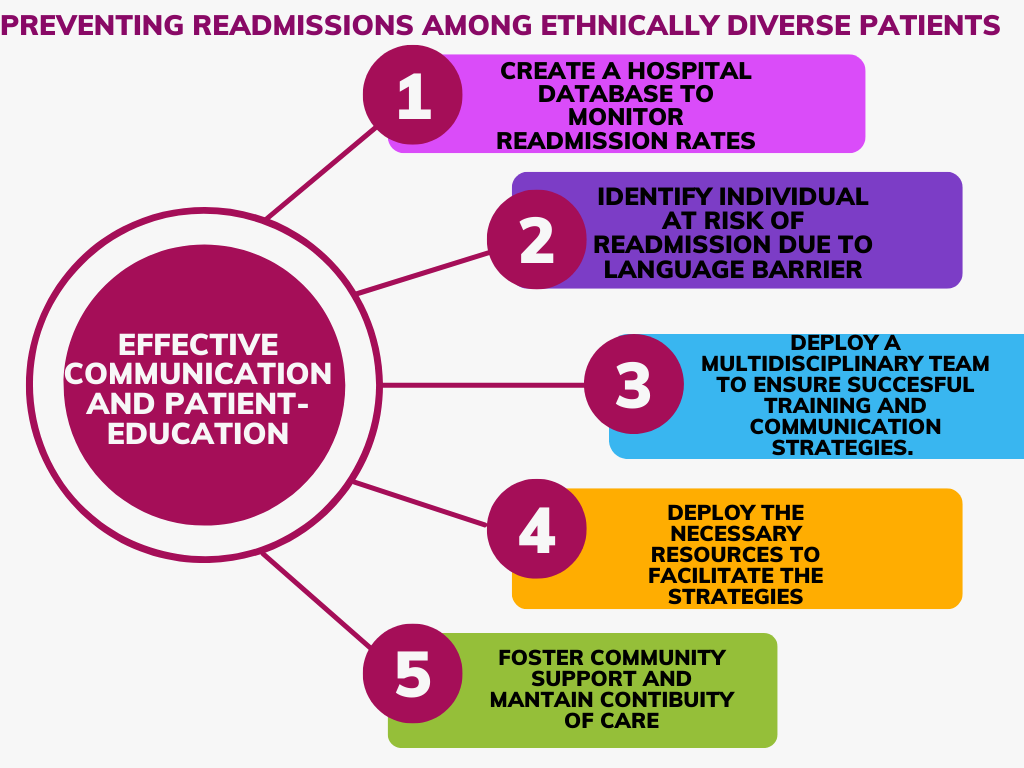
The growth of healthcare reforms calls for change management as medical facilities establish systems that increase the quality of care. One of the major moves that can contribute toward quality of care is preventing avoidable readmissions among ethnically diverse patients to hospitals for chronic conditions. Reducing readmission is important because of its cost-controlling implications. According to the Agency for Healthcare Research and Quality, hospital readmissions cost Medicare paid for 2.3 million readmissions among adults in 2018 (Chamberlain et al., 2018). In addition, hospital readmissions can indicate that the patient is at risk of complications due to ineffective treatment strategies during their first visit. In response to the implications of readmissions, the Centers for Medicare & Medicaid Services (CMS) implemented the hospital Readmission Reduction Program (HRRP) in 2022 to establish penalties for hospitals with excessive Medicare readmissions. As a result, healthcare readmission became a public health concern because of its relation to the patient’s safety and the additional costs that come with the process. Studies have shown that patient-related factors like language barriers can increase readmission risks. According to the Hospital Readmission Reduction Program (HRRP) evaluations, patients from minority populations are more likely to get readmitted within 30 days of hospitals discharging them for chronic conditions than their white counterparts (Qiu et al., 2022). Because of the costs to the system and the individual, healthcare leaders need to address readmissions while meeting the needs of the ethnically diverse population. There is a need for strategies to implement a system-wide reform that prevents readmissions among minority populations. Readmissions related to ethnic disparities are preventable, thus the need for action. This analysis recommends patient education and effective communication as an approach hospitals can undertake to reduce readmissions among limited English proficiency individuals from minority populations.
Summary of the Target Group
The Federal Department of Health and Human Services aims to eliminate disparities faced by ethnic groups when it comes to the treatment of chronic illnesses. Currently, chronic diseases affect millions of people in the United States of America. However, there are differences in the health outcomes in minority groups because of barriers that affect their treatment, patient education, and self-management. one would expect that a person hospitalized for a chronic condition would eventually learn to manage the condition. However, chronic disease management requires adequate education on follow-up care in the post-admission season. A study by Al Shamsi et al., 2020 showed that patients who do not understand the local dialect of the hospital where they are receiving treatment are more disadvantaged regarding quality care. The study also showed that patients in the US who have limited English proficiency experienced more adverse events compared to their counterparts (Al Shamsi et al., 2020). Minority patients that speak little English face additional barriers to health like discomfort in engagements, misunderstanding discharge instructions, mistrust issues, and health illiteracy. Language barriers may also cause miscommunication between the patient and the medical practitioner, which may affect the quality of care and lead to more readmissions. Healthcare practitioners can facilitate care coordination, improve self-management strategies, and minimize readmissions through communication and patient education.
The Role of Leadership and Change Management in Addressing the Problem
Being a leader in the nursing profession is critical because one plays the role of promoting the successful adoption of changing policies. Leadership and change management processes contributed toward effective planning of the change process. Leadership is also important for implementing policies monitoring progress, communicating expectations, and analyzing reasons for the failure of change in the organization. A leader has to be an agent of change by leading his group towards the goals and motivating them to be persistent in embracing change (Junnaid et al., 2020).
On the other hand, change management is vital for controlling and monitoring procedures for creating systems that support the implementation of change. Lack of leadership and change management are likely to develop strategies and negative attitudes of employees towards the process of change leading to failure. Likewise, being a leader in nursing calls for commitment to optimal health for all and promoting equity in healthcare. Healthcare disparities are a complex issue requiring collaboration and partnerships among healthcare leaders. Leaders can work to facilitate training on strategies to promote effective communication and patient education in their areas of work. In addition, leaders can support new solutions that can bring innovative breakthroughs in the campaign to end health disparities. Moreover, leaders can lead research and regulatory reviews on practices contributing to higher readmissions among minorities seeking treatment for chronic illnesses.
The nursing code of ethics provides a guide on four moral principles and obligations when treating patients from marginalized groups (Baptiste et al., 2020). For instance, the ethical code of Justice recommends that all nursing decisions come from a level of fairness and openness to an individual regardless of ethnicity. In addition, the beneficence code of ethics requires nurses to be guided by compassion while contributing to the welfare of others. Likewise, the code of non-maleficence advises nurses to ensure all patients ourselves and to recommend treatment options that will have a beneficial outcome regardless of the patient’s background. On top of that, the nursing code of autonomy asks caregivers to ensure that patients receive all education on the best medical options so that they can make adequate plans for treatment. The nursing code of ethics informs the development of a proposed intervention by calling for leaders in the nursing profession to contribute to creating values and policies that address health disparity.
A Copy of the Intervention/Solution/Professional Product
Strategies for Communicating and Collaborating with the Patient, Family, or Group to Improve Outcomes Associated with the Problem
The focus group for this study involves racial and ethnic minorities with limited English proficiency. Even though not all readmissions are preventable, it is important to minimize avoidable readmissions by addressing the barriers that the patients face. Minority patients with limited English proficiency are more likely to experience a higher readmission rate due to language barriers in communicating medication and lower health literacy. The best strategy is to overcome barriers to communication that could compromise the patient’s health literacy. Therefore, these patients might need interpretation to understand instructions, medical diagnosis, preventive services, and adherence to the dosage. The provision of interpreting services in the hospital can significantly decrease communication errors leading to quality care. It is important to gather the output of the group members to understand if they are linked to any other primary caregiver or if they prefer the translation of instructions. Before carrying out patient education, the medical caregiver should try to understand the patient. It is necessary to understand their health literacy to gauge the patient’s awareness and ability to understand diagnosis and treatment. Nurses also need to know the cultural beliefs that could influence the members’ perception of healthcare. Lastly, the nurse should understand the socioeconomic determinants that could affect readmission rates for patients at hospitals. The health caregiver should ensure that the patient understands medication management to avoid readmissions due to failure to understand recommendations for treatment (Al Shamsi et al., 2020). The nurse should ensure that they communicate in a culturally and linguistically appropriate way that the person will understand without using nursing jargon. One can also include a family member, a caregiver, or an interpreter if it is appropriate to help communicate with patients with limited English proficiency. The nurse can also ask for help from hospital staff who can speak the same language. In addition, the nurse should follow up with the patient to determine if they have understood the instructions to reduce readmission rates related to failure in understanding medication. Understanding the patient helps in identifying the root causes of readmission.
State board nursing practice standards and/or organizational or governmental policies guided the development of your proposed intervention
The standards and policies that guided the recommendations in this work come from government policies and the state nursing board. The 2000 US executive order 13166 has provisions for health institutions to receive finance from the federal government to finance programs that improve services for low English proficiency patients (Pearson et al., 2008). In addition, the state nursing board advises that people shall not be denied benefits or be subjected to discrimination during access to healthcare services based on color, national origin, or race. The affordable care act tackles discrimination and promotes establishing language access services to monitor the disparities in healthcare delivery (Lu & Myerson, 2020). In addition, the American Medical Association(AMA) recommends a commitment to ending healthcare disparities by providing programs that end disparities in healthcare based on language barriers (O’Reilly, 2020). According to Pearson et al.,2008, executive order 13166 has addressed issues of limited proficiency in relation to accessing healthcare services. The author carried out a pilot study that showed that a culturally relevant Spanish language program increased the knowledge level of Hispanic patients with diabetes, leading to increased adherence to recommended preventive services (Pearson et al., 2008). Ever since the affordable care act was implemented in 2010 with provisions for supporting English-speaking citizens, there has been improvement in access to care and deduction of disparities caused by low English proficiency (Lu & Myerson, 2020). likewise, the AMA has collaborated with appropriate stakeholders to develop recommendations on how to improve discriminatory policies and practices in health care (O’Reilly, 2020). In addition, Gerchow et al.,2021 noted interpreters can help in improving nurses to deal with linguistic complexities. Language barriers may create obstacles in receiving instructions that lead to medical errors that increase patient readmission. To reduce the risk of health disparities among people with low English proficiency, the best method is to bridge the gaps that come with language barriers.
How the Proposed Intervention will Improve the Quality of Care, Enhance Patient Safety, and Reduce Costs to the System and Individual
When the patient has limited English proficiency, it can contribute to avoidable admissions because there is a low rate of following up with preventive services, discharge instructions, and medical care strategies. According to Starr et al. (2022), the disparities in patient-clinician communication among ethnic minority patients could cause a disadvantage in the quality of care they receive. Improving communication will ensure that the patients understand the discharge instructions and become aware of the recommendations from the hospital. It is also important to determine if there is an available caregiver so that the nurse can coordinate with them to help the patient understand the recommended diagnosis and instructions. If possible, the medical practitioner can enquire about the patient’s preferred spoken language and offer medication in that language. On the other hand, patient education is important because it can influence their health behaviors. The patient might have deferring perceptions of healthcare and thus a need to educate them on the appropriate medical information. Patient education can facilitate trust with patients because it demonstrates that the medical facility respects their cultural practices and beliefs and is committed to understanding, treating, and managing the patient. Patient education also improves independence in self-management, which reduces the chances of admission. Patient education also addresses other factors, like the side effects of medical non-adherence. It explains to the patient the risks they cause to themselves if they do not follow medical instructions. According to a study by Starr et al. (2022), higher social support can reduce the odds of minority patient admission or death by 65%. Education also gives the medical practitioner a chance to research how patients with low health literacy have a higher risk of readmission and collect critical data regarding the matter.
How Technology, Care Coordination, and the Utilization of Community Resources Can Be Applied in Addressing the Problem
Technology can provide self-management support and care planning for the patient. In addition, technology enhances the coordination of multiple teams in providing healthcare. Technology can also provide tailored support to the patient, which will meet their healthcare needs, thus reducing the chances of readmission. In addition, physicians can use telephonic interpreting services to communicate with patients in their preferred languages. Multilingual applications can provide a cheaper and more convenient solution for nurses who need translators to communicate with their patients. Since there is a shortage of trained interpreters in the medical field, medical practitioners might have to be innovative with technology to cover these gaps. Coordinated care is important because the patient needs social support. Limited English proficiency patients may need the support of members who understand them to avoid miscommunication and errors during the diagnosis. Family support is also important to encourage the patient to seek early treatment and commit to the recommended medical treatment program. Likewise, there needs to be effective communication between the patient and the caregivers to ensure successful treatment and management of chronic conditions. There needs to be coordination between stakeholders in the public health system, like employers, investors, and lawmakers, to support initiatives that reduce inequalities for ethnic minorities when seeking treatment for chronic illnesses. Leaders in healthcare facilities also need to ensure that there are changes made in policies that could cause discrimination toward healthcare access for minorities. Patients who utilize community resources are less likely to encounter hospital readmission because of the additional support and guidance they can get. Public healthcare initiatives usually target populations according to their needs and their special challenges. For example, the public health officers fight to carry out diabetes awareness in Spanish to target community members who speak that language. Therefore, patients from ethnic minority groups may benefit from community resources and programs that help them overcome language barriers among individuals with limited English proficiency. In conclusion, everyone has the right to access quality healthcare regardless of their dress, color, or language. Eliminating communication barriers caused by English proficiency and patient education can improve the patient’s self-management ability, reducing the chances of readmission among ethnic minorities with chronic illnesses.
References
Al Shamsi, H., Almutairi, A. G., Al Mashrafi, S., & Al Kalbani, T. (2020). Implications of language barriers for healthcare: A systematic review. Oman medical journal, 35(2), e122. Web.
Baptiste, D. L., Commodore‐Mensah, Y., Alexander, K. A., Jacques, K., Wilson, P. R., Akomah, J.,… & Cooper, L. A. (2020). COVID‐19: Shedding light on racial and health inequities in the USA. Journal of clinical nursing.
Chamberlain, R. S., Sond, J., Mahendraraj, K., Lau, C. S., & Siracuse, B. L. (2018). Determining 30-day readmission risk for heart failure patients: the Readmission After Heart Failure scale. International journal of general medicine, 11, 127. Web.
Gerchow, L., Burka, L. R., Miner, S., & Squires, A. (2021). Language barriers between nurses and patients: A scoping review. Patient Education and Counseling, 104(3), 534-553.
Junnaid, M. H., Miralam, M. S., & Jeet, V. (2020). Leadership and Organizational Change Management in Unpredictable Situations in Responding to Covid-19 Pandemic. Leadership, 11, 16. Web.
Lu, T., & Myerson, R. (2020). Disparities in health insurance coverage and access to care by English language proficiency in the USA, 2006–2016. Journal of general internal medicine, 35(5), 1490-1497. Web.
O’Reilly, K. B. (2020). AMA: racism is a threat to public health. American Medical Association. Web.
Pearson, W. S., Ahluwalia, I. B., Ford, E. S., & Mokdad, A. H. (2008). Language preference as a predictor of access to and use of healthcare services among Hispanics in the United States. Ethnicity and Disease, 18(1), 93.
Qiu, L., Kumar, S., Sen, A., & Sinha, A. P. (2022). Impact of the Hospital Readmission Reduction Program on hospital readmission and mortality: An economic analysis. Production and Operations Management, 31(5), 2341-2360. Web.
Starr, L. T., Ulrich, C. M., Perez, G. A., Aryal, S., Junker, P., O’Connor, N. R., & Meghani, S. H. (2022). Hospice enrollment, future hospitalization, and future costs among racially and ethnically diverse patients who received palliative care consultation. American Journal of Hospice and Palliative Medicine®, 39(6), 619-632.