Introduction to the Study Level
Introduction
The study focuses on women who have undergone a hysterectomy in Mississippi without comprehensive informed consent law. Hysterectomy is one of the most complicated surgical procedures that may result in serious damages to the woman’s reproductive system (Senie, 2013). In some severe cases, hysterectomy may result in fatalities (Senie, 2013). The comprehensive informed consent law is aimed at providing women with more information concerning various options for treatment (Chima, 2013). The study is critical in understanding the feelings and experiences of women who have undergone the surgical procedure without the comprehensive informed consent law, not only in Mississippi but also across various states in the United States.
Besides providing a brief summary of the literature and describing the gap in knowledge on the concerned topic on the background, this chapter will include the research problem and provide a clear statement that connects the problem being addressed and the focus of the study. In addition, the chapter will include the research questions as well as the theoretical or the conceptual framework on which the study is based.
Background of the Study
Hysterectomy is one of women’s major health issues (Senie, 2013). However, the cases of hysterectomy are prevalent among the minority women. Studies indicate that about 23% women of native origin undergo hysterectomy compared with non-Hispanic white (Wong, Jim, King, Tom-Orme, Henderson, Saraiya, Richardson, Layne, Suryaprasad & Espey, 2011). However, the cases of hysterectomy are minimal compared with other women’s health problems such as ovarian cancer. Also, studies indicate that in the United States, women undergoing the surgical procedure are twice the number in the UK and Sweden.
Further, studies indicate that about 25% of women in the United States have undergone the surgery due to reproductive complications such as severe vaginal bleeding, uterine fibroids and cervical cancer. The reasons why women undergo hysterectomy are diverse, ranging from the relief of pain to the removal of fibroids (Burbank, 2009).
While hysterectomy is not new, it is widely applied without a legal framework that allows doctors to provide information concerning alternative and safer treatments (Chima, 2013). In particular, only three states have established comprehensive consent statutes that act as a cover against potential dangers of hysterectomy. In other words, the rest of the states lack a policy framework aimed at offering physicians an increased opportunity to provide information and enhance the understanding of the alternative and safer treatments.
Streicher (2013) provided alternative surgical procedures, which are exclusive knowledge to women who undergo hysterectomy. However, doctors are expected to provide this knowledge. The comprehensive informed consent law mandates doctors to disclose all information on hysterectomies, including alternative treatment options. The disclosure would provide women with a wide variety of treatment choices. Streicher (2013) provided unconventional and secure procedures that women should know could there be comprehensive informed consent that permit medical practitioners to make known and share out pamphlets on hysterectomy containing information about all therapeutic preferences.
Essentially, the purpose of comprehensive informed consent is to authorize Department of Health (DH) to issue a pamphlet containing information concerning hysterectomy and other therapeutic alternatives. However, few studies have been conducted on women who undergo hysterectomy without information in relation to alternative treatments. Therefore, this study will fill the missing data on the study of hysterectomy as it relates to the lack of policy and comprehensive consent statutes that allow medical practitioners to provide information regarding safer treatment alternatives.
Problem Statement
Twelve out of 10,000 women who undergo a hysterectomy die of complications arising from the procedure. Due to the high mortality associated with this procedure, women should only undergo hysterectomies in life-threatening cases like uncontrollable bleeding, complications arising from childbirth, and severe infections. Approximately 90% of hysterectomy cases recorded in the United States annually are the result of localized illnesses (Bouchez, 2001; National Women’s Health Network, 2005; Nickson, 2014).
Some states have instituted laws aimed at educating women about the potential risks of undergoing hysterectomies. New York has a documented informed consent law that seeks to protect millions of women who are potential candidates of the hysterectomy procedure (Bouchez, 2001; Nickson, 2014). This study will explore the lived experiences of women who have been given the hysterectomy recommendation and undergone the procedure in Mississippi, a state without an instituted comprehensive informed consent law.
The comprehensive informed consent law aims to provide women with an opportunity to understand the alternatives that are available for hysterectomy. Ogdon (2014) purported that the patient and surgeon should have shared decision making, which includes an understanding of the procedure, alternatives, potential risks, and complications. A comprehensive informed consent law is a method of ensuring appropriate and adequate patient knowledge with regard to hysterectomy during the decision-making process (Nickson, 2014).
It is possible to distinguish two variables that are important for this research. In particular, one should speak about the connection between health literacy and informed consent. In this context, health literacy can be defined as the degree to which a person can understand the information about healthcare services, drugs, or medical procedures (American Medical Association, 2007; Nickson, 2014). In turn, health literacy affects the ability of a person to make informed decisions regarding his/her health. This issue is particularly relevant at the time when informed consent of a patient is required (French & Hernandez, 2013).
Hence, a person who does not have health literacy skills is more likely to endanger his/her life and health at the time when he/she has to make choices about different forms of treatment (American Medical Association, 2007; Nickson, 2014). It should be kept in mind that sometimes those patients who have low literacy skills are ashamed of asking physicians about informed consent. As a result, they can become more exposed to various health risks. Thus, these variables are closely related with one another.
Increased complications rates are associated with hysterectomy. In fact, studies indicate that about 120 in 1000 women who undergo the procedure develop post- operative complications (Butt, Jeffery & Van DerSpuy, 2012). The most common complication is the fibroid-related menorrhagia and the uterine bleeding (Butt et al., 2012). Butt, et al., (2012) also found that the patients with malignant disease are more likely to develop intraoperative complications. Post-operative complications are prevalent in abdominal surgery compared with vaginal surgery (Butt et al., 2012). Severe uterine complications normally exacerbate the problem (Freed & Spies, 2010).
Magon and Chauhan (2012) argued that despite the medical significance to women, hysterectomy is still a controversial issue. Further, Magon and Chauhan (2012) observed that the surgical procedure and its role in women’s healthcare is the cause of disagreement. Despite the effects and advancements in medical practice, the procedural choice of a particular hysterectomy is not normally based in evidence, rather on personal notion (Magon & Chauhan, 2012).
Regardless of the incessant cases of hysterectomy, about 45 states have not enacted consent laws aimed at providing more information concerning various options to the surgical procedure (Senie, 2013). To that end, legal frameworks aimed at educating women concerning the potential safer alternative therapies are lacking. Even though the aforesaid studies elucidate significant findings concerning women who have undergone a hysterectomy, there exists a deficiency in the study of hysterectomy as it relates to the policy and comprehensive consent statutes (Berg, Appelbaum, Lidz & Parker, 2009). As a result, the problem of lack of comprehensive informed consent law aimed at providing women with the opportunity to understand the alternatives that are available for hysterectomy exists.
Previous studies have focused on issues concerning the consequences of the surgical procedure (Cofey, 2013). Also, the most recent studies indicated that the decisions of women undergoing the surgical procedure differ greatly between the states that have enacted the comprehensive informed consent statute and those that lack the law (Senie, 2013). Even though the study focuses on the case of Mississippi, the research will provide data that will be applied generally in all states that have not enacted the comprehensive informed consent law.
The Purpose of the Study
The study tends to explore the decision-making processes of women in Mississippi who have undergone hysterectomy in the absence of comprehensive informed consent. In particular, the study aims to examine the attitudes and beliefs of women in Hinds County, Mississippi, who have undergone hysterectomy without any comprehensive law concerning their informed consent. Additionally, the study will identify the perceptions and new ideas emerging from the lived experiences of women who have undergone hysterectomy in the absence of comprehensive informed consent law.
The study will utilize the health belief model (HBM) to explain the behavioral aspects of patients based on the principles of individual perceptions. In addition, the study will primarily apply the phenomenological approach, which is utilized extensively to gather more information concerning individual perceptions through qualitative research methods (John, Malekpour, Parithivel & Goyal, 2014). Since the main purpose of the study is to examine the beliefs and attitudes of women in Hinds County, the study will fully utilize interviews to gather the information. The interviews will focus on the participants’ personal experiences and detailed accounts of the occurrences of women who have undergone hysterectomy in the absence of comprehensive informed consent.
Research Questions
Upon completion of the study, the following questions will be answered
- What are the perceptions of women who have undergone hysterectomy without prior awareness of comprehensive informed consent?
- What are the new themes that emerge from the lived experiences of women who have undergone hysterectomy in the absence of comprehensive informed consent law?
Theoretical Framework
The theoretical framework of the proposed study will be based on the health belief model (HBM). This model was originally developed to explain why patients fail to participate in preventive care and treatment (Rosenstock, 1974; Nickson, 2014). The HBM is one of several behavioral theories that has been used to help explain individual health-related behavior based on several principles. The principles of this model are the “individual’s overall perception of his or her susceptibility to disease, perception of the severity of the disease and perception of the benefits from the barriers to modifying behavior” (Bellamy, 2004, Abstract).
The HBM purports that an individual makes decisions regarding health behaviors (surgeries, preventive care, and follow-up treatment) based on perceptions. Adequate patient education aids in making an informed choice regarding health behaviors and is an important part of how the behavior is perceived (Bellamy, 2004; Nickson, 2014; Watson, 2011). The HBM will help address the lived experiences of women who have undergone hysterectomies in Mississippi by exploring how the absence of the comprehensive informed consent law affected the participants’ decisions to undergo the surgery. The HBM is useful in answering the research questions and uncovering themes related to the common phenomenon experienced by the subjects.
The theory is based on the principle of individual perception of personal health-related issues. The model asserts that individuals make decisions based on the perceived medical care (Schiavo, 2013).
According to Huber and Tu-Keefner (2014), HBM has been widely applied in various fields within the health sciences to explain human behavior. The model is useful in answering the research questions and uncovering new areas that relate to the common incidents the participants experienced.
Nature of the Study
This study is qualitative in nature. Qualitative study approaches aim to investigate the interpretation individuals give to a social or human problem (Creswell, 2013; Nickson, 2014). Thus, this study will focus on the attitudes and beliefs of women in Hinds County, Mississippi who have undergone hysterectomies without the presence a comprehensive informed consent law. It will be necessary to recruit subjects who have at least a high school diploma (Nickson, 2014).
In this way, one can ensure that the subjects have comparable perceptions of informed consent. They are more likely to act similarly in a medical setting. Much attention should be paid to the patients’ abilities to understand the informed consent. In particular, one should ask several questions about the legal consequences of signing informed consent documents. This precaution can help the researcher to understand the perceptions and attitudes of respondents. Admittedly, the study may become more time-consuming; nevertheless, by asking these questions, one can gain better insights into the decisions of the patients (Nickson, 2014).
The study design approach that best suits the study is the phenomenological approach. Phenomenological approaches are utilized to illuminate and identify phenomena by deciphering how they are viewed by individuals in a situation (Creswell, 2013; Nickson, 2014). It is applied in the human sphere to gather deep information and perceptions through qualitative research methods. The methods could be interviews, observations and discussions, among others (Creswell, 2013; Nickson, 2014). Specifically, the approach focuses on the study of experiences from the perspective of actors.
Owing to its extensive application as a qualitative interview technique in the social and health sciences, this approach would allow the structuring of interviews with predetermined questions (Creswell, 2013; Nickson, 2014). A comprehensive interview questionnaire will be administered to the study participants randomly selected from members of a support group in Hinds County, Mississippi. Using data collection technique, the responses will be sampled using a phenomenological approach.
The questions would be modified when necessary to reflect the dynamics of the study. Creswell (2013) asserts that phenomenological research commences with detailed descriptions of lived circumstances, most often first-person accounts, organized in an everyday language that avoids the use of scholarly and theoretical terms. The approach will enable the researcher to gather a detailed account of the lived experience of women who have undergone hysterectomies. The approach will aim to reduce the participants’ personal experiences with a phenomenon to a representation of the shared core (Nickson, 2014).
Definitions
- Hysterectomy – A surgical procedure to remove the uterus
- Mortality – The state of being susceptible to death
- Cyst – a pocket of human tissue
- Antisepsis – A medical practice of using antiseptics to eliminate disease-causing mechanisms
- General Anesthesia – A medical treatment that puts patients into a deep sleep to help them avoid pain
Assumptions
Interviews are the main data collection technique. Based on this research instrument, we assume that the respondents would answer the questions truthfully. Similarly, since a specific research sample is used, we assume that the sample would be representative of the views of women who have undergone hysterectomy in Mississippi. However, to overcome this assumption, the methodology of this paper includes a random sampling technique to make sure that the sample chosen represents the desired demographic.
Scope and Delimitations
Delimitations of a study refer to issues that are within the researcher’s control. The geographical region covered by the study is a delimitation of this study. In this study the experiences of Mississippi women who have undergone hysterectomy are covered. Another delimitation of the study is the selection of the respondents for the interviews as the main reference point for gathering information concerning the experiences of women who have undergone hysterectomy (Grove & Gray, 2010).
Limitations
Study limitations refer to issues that are out of the researcher’s control. In this study, time is a significant limitation in particular, during the data collection process where the interviews may be restricted depending on the time allowed by the respondent. Another limitation is the demographic of analysis. While the study would have been better conducted in large and diverse female populations, the study is restricted to only a few women in Mississippi. The study will mainly focus on sampling the views of Mississippi residents. Therefore, its findings may be limited in the same regard.
Significance
This study is significant because it focuses specifically on the decision-making process of women in Mississippi who have undergone hysterectomies in the absence of a comprehensive informed consent law. By focusing on the lived experiences of this population, this study will bring insights into the perceptions of participants’ abilities to make patient-centered decisions related to their health outcomes. Hence, the study’s findings have the potential to bring about positive social change in women (Nickson, 2014).
This research can lead to the improvement of health services. In particular, medical workers such as nurses and physicians can better understand the experiences of women who underwent hysterectomies. Thus, healthcare professionals can better educate these women who may not easily cope with the effects of hysterectomy. These women often find it difficult to adjust to the problems originating from this surgery (Reis et al., (n.d; Nickson, 2014). Therefore, educational assistance of medical workers is of great value to them. This is one of the benefits that this study may bring.
Additionally, by understanding the challenges faced by these women, medical workers can better explain the options which are available to women who may need to undergo hysterectomy. In particular, they should fully understand the effects of this surgery on the health of a woman. This is another example of positive social change. Furthermore, this study can demonstrate what particular issues are most pertinent to women who may need to undergo a hysterectomy. By using the findings of the study, medical workers can help patients make informed decisions. This is one of the positive social changes that should be considered (Nickson, 2014).
Moreover, it may be necessary to provide counseling to women who underwent this surgery in the past. This type of assistance can also be viewed as one of many health services. In turn, the results derived in the course of this study can assist such counselors who will be able to work more effectively. Thus, one can say this research can eventually promote the practices which can improve the experiences of many individuals whose needs could have been previously overlooked by medical professionals (Nickson, 2014).
Data from this study may inform legislatures regarding the need for a comprehensive informed consent law that provides clear guidelines for both patients and physicians. Because some patients do not understand surgical procedures and associated risks, informed consent is fundamental in healthcare. It signifies the physician is speaking to a patient in simple terms that the patient understands, as well as disclosing all pertinent information and dangers. As a result, the patient understands that surgery is a choice (Bouchez, 2001; Nickson, 2014). Standards of care are established in guidelines and in the medical evidence and patients have a right to know all reasonable alternatives consistent with high-quality medicine (Bouchez, 2001; Nickson, 2014).
The findings of this study will contribute to existing academic knowledge regarding hysterectomy and the absence of informed consent when undergoing such procedures. Policymakers and health practitioners would also find this information useful in developing policies and procedures that guide this health process. This way, they will have a proper guiding framework for the development of informed consent law in Mississippi and around the country. With law guiding the informed consent, women will be able to undergo hysterectomy fully aware of the procedure and the consequences.
In addition, women will be capable of making decisions based on the disclosed information. As a result, women will have various treatment alternatives as indicated in the booklets.
Summary
This chapter highlights the nature of the study and sets the tone for the rest of the dissertation. It shows that the study will explore the lived experiences of women who have undergone hysterectomy without informed consent. The findings of the study will add more knowledge to existing literature. Similarly, policymakers will use the study findings to understand the importance of informed consent law when undertaking the medical procedure.
Literature Review
This chapter evaluates previous research studies that have explored the intrigues surrounding women who have undergone hysterectomy without informed consent. It highlights key variables and concepts surrounding the medical procedure and the different ways that researchers have approached the issue. This way, it is easy to understand the major theoretical composition of the research issue and any major hypothesis that may arise from the same.
Literature Search Strategy
Information included in this study has come from credible sources primarily from previous studies. Most importantly, there has been a keen focus on previous studies published in books, journals, peered reviewed journal articles and credible websites. Some key databases consulted include emerald insight and sage journals. In addition, Cochrane Menstrual Disorders (CMD) and Subfertility Group Trials Register (December 2009 to January 2014) were searched.
Besides, the following health sciences electronic databases were searched into including CENTRAL (The Cochrane Library 2013, Issue 12), CINAHL Plus (January 2009 to January 2014), MEDLINE (January 2009 to January 2014), Health and Medical Complete (January 2009 to January 2014), EMBASE (January 2009 to January 2014), and PsycINFO (2009 to January 2014). Key search terms included “hysterectomy” and “informed consent.”
Theoretical Foundation
As highlighted in the first chapter, the HBM model outlines the main theoretical foundation of this paper. This framework guides the research process outlined in this paper by narrowing down our focus to behavioral responses and perceptual influences about hysterectomy. Researchers such as Boosz, Lermann, Mehlhorn, Loehberg, Renner, Thiel, and Mueller (2011) have used this theory (before) to investigate the behavioral patterns of patients, based on perceptual responses to policy and environmental issues.
Literature Review Related to Key Variables and Concepts
Hysterectomy has its origin in pre-historic times, with the first operation performed as early as 120 AD by Soranus in Greece. Alsaharavius, a physician in the 11th century, made a commentary about a surgical excision of the uterus. Vaginal hysterectomies had been performed in the Middle Ages, as revealed by some medical writings.
In 1809, Ephraim McDowell performed the first abdominal hysterectomy on Jane Todd Crawford, who had a massive ovarian cyst weighing 10.2 kilograms. It took McDowell 25 minutes to remove the left tube and the ovary, while outside his house townsfolk were building a gallows for him in case the patient would die. Five days later, Jane Todd was well and up in McDowell’s house and after 20 days, she went home to Greensburgh, Kentucky. At that time, surgeons operated without anesthesia, antisepsis or antibiotics, and the patient was allowed to recite the psalms to slightly ease the pain. McDowell performed 13 hysterectomies in the course of his practice, with only one death. It was an extraordinary feat considering that sepsis and peritonitis were complications after laparotomy.
Charles Clay came up with the word “ovariotomy.” On September 13, 1842, he removed a 17-pound, 5-ounce ovarian tumor, with the patient having a brandy and milk for analgesia. When anesthesia was discovered, Clay did not want to apply it for his patients as he considered it a distraction. He reasoned out that patients who had the courage to undergo surgery without anesthesia were imbued with a strong will to live. On January 3, 1863, Clay (1863) performed the first successful hysterectomy with oophorectomy and salpingo-oophorectomy.
In 1853, Ellis Burnham successfully performed a subtotal hysterectomy and the patient survived. Another surgeon named Kimball performed a deliberate but successful hysterectomy due to fibroid tumor. Chloroform as a form of anesthesia was used during the operation. Before this time, surgeons used opiates, which contained Hyoscyamus and mandragora, mixed with alcohol to desensitize patients undergoing surgery. The nitrous oxide gas was introduced which could induce amusement and euphoria and reduce sensitivity to pain. In 1831, a combination of ether, nitrous oxide and chloroform was later used as anesthesia. Dentists used ether as dental anesthesia and it was Oliver Wendell Holmes who first coined the word anesthesia.
Many women undergo hysterectomy for noncancerous illnesses and as a preemptive measure for ovarian cancer. Gynecological problems and cancer are the primary causes of hysterectomy (Sparić, Hudelist, Berisava, Gudović & Buzadzić, 2011). Many hysterectomy cases in the United States are result of localized sickness, which means the sickness does not spread to the uterus, and removal of the uterus is not necessary (Sparić et al., 2011).
About a quarter of women in the United States may have undergone hysterectomy when they have reached 60 years old, whereas in the United Kingdom, the ratio is one to five women. More than 90 percent of those surgeries were performed for benign tumors and symptoms for uterine fibroids, vaginal bleeding, and others which are non-life threatening. However, some women undergo complex surgeries such as the peripartum hysterectomy (Suwannarurk, Thaweekul, Mairaing, Poomtavorn & Bhamarapravatana, 2014).
Gupta and Manyonda (2014) indicated that 40 percent of all women worldwide will have a hysterectomy when they reach 64 years old, with the primary objective of relieving pain and enhancing quality of life. With the introduction of alternative treatment, hysterectomy has become less prevalent in most countries (Forsgren & Altman, 2013).
There are still doubts surrounding hysterectomy and why women should undergo hysterectomy. Forsgren and Altman (2013) have asked these questions: Can hysterectomy provide the essential treatment for diseases in women’s reproductive organs? Should other less invasive treatment be considered first before a woman should undergo hysterectomy? How informed are women of the legal aspects of hysterectomy, particularly the subject of informed consent?
Women have to be informed on treatment options other than hysterectomy which has complications. A comprehensive informed consent law requires physicians to provide information concerning other alternative therapy (Chima, 2013). The benefits of informed consent law will allow women to decide before any treatment is performed (Chima, 2013). This information and knowledge of the law should be properly understood by women.
Hysterectomy is one of the most frequently used operative techniques among many gynecological procedures, but is significantly decreasing because there are alternative options and patients have reported some complications after hysterectomy (Darwish, Atlantis, & Mohamed-Taysir, 2014). Firouznia, Ghanaati, Sanaati, Jalali and Shakiba (2009) found out that the complexities in the surgical procedure a rise when pregnancies occur. A longitudinal study found that more women who belonged to lower socio-economic class had undergone hysterectomy than those of the higher socio-economic status. Knowledge about, and access to, other treatment may not be available in specific areas, which is one of the reasons why those who are of the lower socioeconomic status mostly undergo hysterectomy (Bower, Schreiner, Sternfeld, & Lewis, 2009).
Mississippi Delta Region is one of the specific areas where socio-economic status of women is lower and accessibility to other treatment options is limited (Wong et al, 2011). As a result of the prevailing situation, women also lacked education and experienced poor nutrition as well as healthcare (Wong et al, 2011). These factors could have resulted in lack of valuable information for women who might have undergone hysterectomies, and there was also dearth of knowledge on cancer screening and other health-care expenses (Wong et al, 2011).
Every year, approximately 600,000 American women undergo hysterectomy for non-cancerous causes (Perera et al., 2013). The Centers for Disease Control and Prevention (2014) reported that there were 5.4 hysterectomies for every 1,000 women annually during the period 2000 to 2004. However, hysterectomy rate is decreasing in the Scandinavian countries and in the United Kingdom (Schollmeyer et al., 2014).
Ovarian and uterine cancers are primary causes for hysterectomy (Singh, Ryerson, Wu, & Kaur, 2014). In a study on cervical cancer, researchers found that hysterectomy did not reduce the survival rate but provided comfort in the pelvic region. Moreover, some doctors performed hysterectomy on complaints of endometriosis, which can be treated with analgesic therapies and other non-invasive methods (Graaff et al., 2013).
A study on endometriosis and its effects on the quality of life revealed that this sickness impacted on impacted on women’s quality of life, particularly on their work, education and home and family life (Graaff et al., 2013). The effect of endometriosis on work was more pronounced with 51 percent of the participants saying that endometriosis significantly affected their work life. Endometriosis also affected the women’s relationships with their husbands, with some participants saying that their sickness caused divorce.
The data collected in the study confirmed the negative effects of endometriosis on women’s quality of life (Graaff et al., 2013, p. 2682). Uterine myomata or leiomyomas are some common causes of menstrual bleeding. Approximately 30 percent of hysterectomies are performed due to diagnosis of fibroids. Myomectomy is an alternative to hysterectomy in removing fibroids, but it requires a longer recovery period.
Meaning and causes
Hysterectomy is a surgical method to treat gynecological problems with the aim of removing the ovaries or the fallopian tube. The removal of the ovaries or the fallopian tube may result in a menopausal period and the woman will be unable to become pregnant. Uterus amputations do away with uterine cancer. On other hand, oophorectomies get rid of the possibility of ovarian cancer (Wong et al., 2011).
Yeh et al. (2013) indicated that bilateral salpingo-oophorectomy (BSO) can reduce the risk of ovarian cancer − the reason it is performed bilaterally with some hysterectomies. While ovarian cancer can be avoided, oophorectomy increases risks of heart disease and lung cancer. Papadopoulos, Tolikas and Miliaras (2010) also argued that the new methods of the surgical procedure could be used to avoid risks associated with the surgical procedure. Cardiovascular risks may be higher due to reduced production of endogenous sex hormone (Yeh et al., 2013). A previous cohort studies supported evidence on the relation of hysterectomy and cardiovascular disease in women who were less than 45 years of age during operation.
Relation of HRT and CHD
There have been studies saying that hormone replacement therapy (HRT), which is prescribed for women who have undergone hysterectomy, causes coronary heart disease (CHD). However, there were studies reporting that HRT users did not have cardiovascular risks, while some studies showed that the effects of HRT were not clear and “over-estimated” (Matthews, Kuller, & Wing, 2009; Posthuma, Westendorp, & Vandenbrouche, 2010; Lambert, Straton, Knuiman, & Bartholomew, 2012).
Women with the uterus intact take prescribed estrogen and progestin as protection from cancer occurrence. HRT, which has a dose of progestin, can ease estrogen in controlling CHD, although there has been a reported little increase in CHD in women who take the combined dosage. The study of Lambert et al. (2012) provided inconclusive evidence that HRT caused CHD, but the findings also stated that HRT was associated with hysterectomy. Women who use HRT have lower levels of systolic blood pressure and low cholesterol (Prior, Stanley, Smith, & Read, 2012).
Techniques and types of hysterectomies
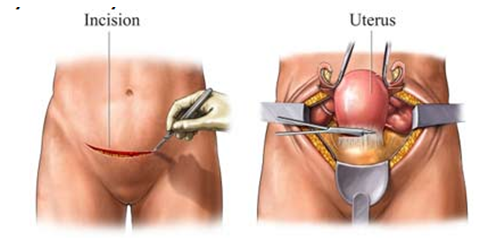
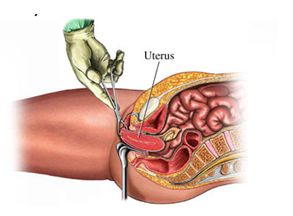
Techniques in hysterectomy include open surgery performed through the vagina or a method using laparoscopy, and the most modern, which is robot-assisted operation (Tapper et al., 2014). Laparoscopic hysterectomy (LH) is usually applied in benign and malignant tumors. Vaginal hysterectomy is used in many cases while LH is usually performed in cancer cases (Tapper et al., 2014). LH can be performed vaginally accompanied by laparoscopic procedures or where there is no vaginal component.
The American Gynecologic Laparoscopists issued a statement in 2010 that hysterectomies for benign cases should use vaginal or laparoscopic procedures because of the benefits on women (Gupta &Manyonda, 2014). These benefits include lower costs effective, shorter hospital stay and quick recovery (Weber & Lee, 2009). However, in a later study in Ohio by the same authors, they found that this method was associated with higher charges than the other two techniques of hysterectomy. In this same study, Weber and Lee (2009) found that the rate of hysterectomy in the state decreased between 1988 and 1994 due to the introduction and constant use of laparoscopically-assisted vaginal hysterectomy.
Complete hysterectomy aims for the uterus along with the cervix while partial hysterectomy does not aim for uterus removal. Supracervical hysterectomy is performed when complications during operation necessitates completing the required surgery as early as possible. However, supracervical hysterectomy should be planned for patients who are perceived to have higher perioperative complications.
Vaginal hysterectomy is surgery performed through the vagina wherein the surgeon conducts operation on the vaginal wall to be able to see the ligaments and tissues of the uterus, ovaries, and fallopian tubes (Sheth, 2013). These organs can be removed through the vagina. Findings in randomized trials have shown that “vaginal hysterectomy is the most beneficial hysterectomy procedure for women, as well as being the most cost-effective” (Benassi et al., 2003; Ayoubi et al., 2003; Ribeiro et al., 2003 as cited in Boosz et al., 2011, p. 269).
In total hysterectomy, the portion called the “top” of the vagina is closed, creating a “blind” pouch. In this case, intestines are placed (instead of the uterus) in the blind pouch created due to hysterectomy (Harvard Women’s Health Watch, 2009). Abdominal hysterectomy is performed when the woman has acquired an enlarged uterus and cancer has been diagnosed or suspected. This procedure takes a vertical incision, about 4” to 6”, along the pubic section and the navel (Harvard Women’s Health Watch, 2009).
With respect to morbidity and mortality, research found complications in 44 percent for abdominal and 27.3 percent for vaginal hysterectomies. A Cochrane study found fewer infections and rapid recovery attributed to vaginal and laparoscopic hysterectomies than abdominal hysterectomy (Gupta & Manyonda, 2014).
Hysterectomy is most necessary when pain cannot be controlled due primarily to fibroids, or pressure and severe bleeding. It can be applied to postmenopausal women who might have malignant tumors and for symptoms of endometriosis which cause pelvic pain, pain during intercourse, and when there is extreme bleeding (Harvard Women’s Health Watch, 2009). Hysterectomy is effective treatment for menometrorrhagia, leiomyoma, and symptoms associated with post-menopause.
Women that have not been associated with ovarian disease would not have their ovaries and fallopian tubes removed. In such women, the production of hormones would be normal even if they experience lapse in their menstrual cycles. However, when they undergo hysterectomies, they will occasionally cease from producing estrogen and experience the menopausal stage (Harvard Women’s Health Watch, 2009).
Complications in hysterectomy
Hysterectomy can lead to psychological or mental problems, but some studies have found that hysterectomy provided comfort to women and improved their quality of life. However, women should seek other options before undergoing hysterectomy (Harvard Women’s Health Watch, 2009). The doctor and the patient should have substantial discussion before proceeding and the doctor must observe the highest ethical standards of medical practice.
There are valid medical reasons for hysterectomy but there are as many valid reasons as possible for not performing it, which means there are other options rather than immediately subjecting the woman’s reproductive region to surgical procedures. Epidemiological studies showed that for two decades approximately 90 percent of hysterectomies were done for only benign surgical reasons (Darwish et al., 2014; Papadopoulos, Tolikas & Miliaras, 2010). Women who undergo this surgical procedure must be informed of the reasons why it has to be done, how it should be done, including other medical options and complications in later life. Patients have to think of it and give their consent only on life-threatening conditions (Harvard Women’s Health Watch, 2009).
Due to the results of the various studies, the medical profession has raised concerns over the long-term effects of hysterectomy. For example, there have been reported six complications for every 10,000 surgeries performed in the United States (Ruuskanen, Hippelainen, Sipola, & Manninen, 2010). Additionally, studies have found that women who had bilateral oophorectomy had a 17 percent risk of having heart disease and a 28 percent risk of succumbing to death due to complications.
Lung cancer was also one of the complications (Harvard Women’s Health Watch, 2009). Moreover, “hysterectomy with oophorectomy has been shown to accelerate menopause by 3-4 years,” which is caused by the disturbance of blood supply in the ovaries and “can have a deleterious effect on cognitive functions” (Phung et al., 2010, p. 44). Some studies also found that women who had undergone premenopausal bilateral oophorectomy showed signs of reduced cognitive functions, but those taking HRT reported improved cognitive functions.
The reported dementia because of hysterectomy is still unexplored, but a longitudinal study of homozygous twins who had undergone hysterectomies showed symptoms of Alzheimer disease (Phung et al., 2010). Brown, Sawaya, Thom and Grady (2009) reported six deaths in 10,000 hysterectomies.
Some studies reported major complication in urinary incontinence (loss of control in urination) and bowel dysfunction, which occur in old age and affect women’s quality of life. However, the study of Forsgreen and Altman (2013) on a few randomized clinical trials focusing on the relation of hysterectomy and urinary incontinence provided inconclusive evidence. This is shown in Table 1.
Table 1. From “Long-term effects of hysterectomy: A focus on the aging patient,” by C. Forsgreen and D. Altman, 2013, Aging Health, 9, p. 183. Reprinted with permission.
Randomized clinical trials, shown in table 1, indicated that the studies had little evidence to offer because of the few cohort studies conducted. Despite this few evidence of cohort studies, Forsgreen and Altman (2013) still concluded that urinary incontinence and bowel dysfunction were complications for hysterectomies when women reached old age. Brown et al. (2009) supported this finding when they researched on urinary incontinence through Medline articles, using search words, and found that women who had hysterectomy were 40 percent higher in acquiring urinary incontinence at later life than women who had not undergone hysterectomy (Brown et al., 2009). Other complications included occasional fever, hemorrhage, and other life-threatening events (Brown et al., 2009).
Pelvic floor dysfunction is a common problem of women who are at menopausal stage (Wright, Tergas, Burke, Cui, Ananth, Chen & Hershman, 2014). Uterine problems can greatly affect women’s social lives, especially in this age of globalization where women have vast roles in society. Hysterectomy can relieve symptoms that have interfered in their daily activities. Studies indicate that over 40 percent of women who have their ovaries removed have a decreased degree of depression. Moreover, women having positive perception of their social support network in both pre and post hysterectomy indicate increased chances of having quality of life. Physical complications in hysterectomy include edema and swelling in both legs. Long-term physical effects include numbness, tingling, and limited movement of the legs.
Another factor that affects women undergoing hysterectomies is inequities. Studies have found evidence of inequities for women which need to be addressed by healthcare professionals for a corresponding intervention. The team should determine the psychosocial drawbacks of hysterectomies and meet the psychological needs of women.
There are cases that hysterectomy is necessary, such as the occurrence of postpartum hemorrhage (PPH), which is related to birth events threatening a mother’s life that affects her adjustment to motherhood (Elmir, Schmied, Wilkes, & Jackson, 2012). Severe PPH is described as blood loss equivalent to about 1,000 milliliter right after giving birth until weeks postpartum (Elmir et al., 2012, p. 1120). There are cases that PPH needs emergency hysterectomy to control the bleeding (Elmir et al., 2012). PPH and subsequent hysterectomy are two difficult situations that a mother should be able to adjust to after giving birth.
Elmir et al. (2012) conducted a study on perspectives of early mothering by describing their adjustment and recovery from an emergency hysterectomy after a severe PPH. During the recovery period, the mother may be separated from her baby, as she has to be admitted to the Intensive Care Unit (ICU) for observation and careful recovery (Elmir et al., 2012). During this time, the mother may experience guilt feelings, shame and failure. In Australia, the incidence of women admitted to ICU after birth is 1.84 to 2.6 percent of all pregnant women (Elmir et al., 2012). UK has 0.9 percent of pregnant or postnatal women admitted to ICU (Elmir et al., 2012).
On the relation of hysterectomy and breast cancer rate, the study by Woolcott et al. (2009) found no relation between breast cancer rate and simple hysterectomy. However, the researchers found that risk factors for hysterectomy were also common risk factors for breast cancer. This meant the conditions were similar for both illnesses but there was no relation between hysterectomy and breast cancer.
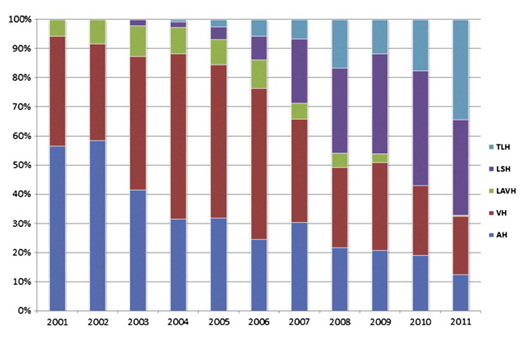
An analysis of hysterectomy performed for benign disease was conducted at the Department of Obstetrics and Gynecology, University Hospital Schleswig-Holstein, Campus Kiel, Germany, in which the data were taken from hospital records. The causes for surgery included fibroids and precancerous abrasions of the uterus (Schollmeyer, et al., 2014, p. 45). The techniques used in the various operations included vaginal hysterectomy, abdominal hysterectomy, TLH, LSH, and laparoscopically assisted vaginal hysterectomy (LAVH). Only 766 patients qualified for the criteria of the study. The common cause for hysterectomy was uterine myoma, which accounted for 58.6 percent of the study.
Vaginal hysterectomy was the common technique used for uterine prolapsed. In the study period, the researchers found no mortalities for hysterectomy for benign reasons but there were 52 (5.5 percent) cases, which had complications out of the total 953 operations. For the period 2007 to 2010, the numbers of abdominal hysterectomy and vaginal hysterectomy decreased due to the increase of laparoscopic hysterectomy (LH) and total laparoscopic hysterectomy (TLH).
Some studies found symptoms of psychological co-morbidity due to hysterectomy which can result into negative feelings about body image, sexual orientation, youth, energy and physical activities, and reduced child-bearing ability (Darwish et al., 2014). However, in conducting a meta-analysis of the different studies and articles on hysterectomy, Darwish et al. (2014) found that hysterectomy performed for benign gynecological conditions was positively associated with depression or anxiety outcomes. Moreover, long-term studies suggested that women returned to their physical and psychological functioning after hysterectomy.
Darwish et al. (2014) study further found that hysterectomy, no matter what type and technique used, had improved the quality of life and psychological outcome of women. There was a reduction in the symptoms of depression and depression scores compared to the preoperative indications. This suggests that women usually felt comfort after the non-malignant indications were removed due to hysterectomy. Sexual pleasure, arousal and desire improved after hysterectomy, regardless of the surgical technique used (Darwish et al., 2014).
Impact of hysterectomy on women’s lives
In other cases, hysterectomy creates psychological problems such as depression and low self-esteem, and negative outcome on patients’ social lives. Elmir et al. (2012) indicated that women feel intense pain right after hysterectomy. In a similar case, Linenberger and Cohen (2004 as cited in Elmir et al., 2012) studied 65 women, who had a mean age of 42 years, experiencing abdominal or vaginal hysterectomies. The researchers found that hysterectomies limited their physical activities while others felt the experience was worse than a caesarian operation. A caesarean operation accompanied with hysterectomy requires time to recover, as this may result into emotional, physical and psychological stresses (Elmir et al., 2012).
Hysterectomy without ovary removal is a different case. It has argued that hysterectomy do not greatly affect women when the ovaries are not removed. However, quality of life should be considered when determining the effects of illness. Quality of life is linked with the individual’s sense of comfort and happiness in life.
Studies in Taiwan and Turkey have found that women regard “the uterus as the symbol of femininity, sexuality, fertility, and maternity, and the loss of this organ is identified as the loss of womanhood because giving birth to a child is an important function for many women” (Pinar, Okdem, Dogan, Buyukgonenc, &Ayhan, 2012, p. E99). In the study on women who have undergone hysterectomy, Pinar et al. (2012) found that hysterectomy adversely effects on patients’ body images, self-respect, and matrimonial status.
In order to answer the various concerns about the overuse of hysterectomy, scholars from the University of California at San Francisco conducted a study on hysterectomy and other treatment options and their impact on women’s quality of life. The study employed 63 participants, aged 30 to 50, who were suffering from excessive bleeding for four years. The women took synthetic progesterone treatment, but this was unsuccessful.
The researchers recommended hysterectomy to a group of participants and some to hormonal medication or birth control pills. The researchers asked the participants of their opinion about quality of life, their physical and mental conditions, and their feeling after hysterectomy. After a period of six months, the participants who underwent hysterectomies reported reduced abnormal bleeding, and had improved sleep and quality of life, including overall health and wellbeing. Seventeen of the 32 members of the medication group opted to have hysterectomy and also reported improved well-being. But the participants who did not undergo hysterectomy also reported improvement in their quality of life (Harvard Women’s Health Watch, 2009).
Additionally, in a 2000 survey of women who have undergone the surgery, the researchers found that respondent women reported improved sexual functioning (Harvard Women’s Health Watch, 2009). A randomized survey in 2007 by “BJOG: An International Journal of Obstetrics and Gynecology” supported this finding, wherein respondents who had hysterectomy reported enhanced sexual functioning than they had before they underwent hysterectomy (Harvard Women’s Health Watch, 2009).
In a report by the Maine Women’s Health Study, many women indicated that they were satisfied with the result of hysterectomy. In a study on women aged 25 to 50 who had either hysterectomy or noninvasive treatments for benign tumors, fibroids, abnormal bleeding, and pain in the pelvic region, Dr. Karen Carlson of the Women’s Health Unit at Massachusetts General Hospital in Boston found positive perceptions of hysterectomy. The respondents reported that hysterectomy relieved their gynecologic problems and that their physical and mental health improved. A small percentage of the population indicated that they lost libido and had little sex enjoyment (Harvard Women’s Health Watch, 2009).
Women and informed consent law
It is noteworthy to provide some actual cases of hysterectomy in this section to define the impact of this medical practice on women’s lives. Nora Coffey (2013) underwent surgery to get rid of a benign cyst but later found out that the doctor who operated her also removed the uterus and ovaries. It was a traumatic experience for this woman that led her to some unexplored activities as a woman and as a health activist later on. Coffey then founded a not-for-profit foundation known as the “Hysterectomy Educational Resources and Services Foundation” (HERS) to provide valuable information for women who might experience non-life threatening medical situations and the benefits of an informed consent law before they undergo hysterectomy (Coffey, 2013).
Brahams (2009) provides another case involving a happily married woman who was rushed to a hospital for emergency appendectomy. During the operation, the surgeon found severe endometriosis. A gynecologist was asked to give an opinion and she concluded that the best option was to remove the fallopian tubes and the ovaries. It was found that the patient had a bilateral ovarian cystectomy for endometriosis in 1979 but was not informed that it would create a severe problem in the future. The patient was completely depressed to learn that she had lost her reproductive organs. She went into a depression and her marriage crumbled.
In 1992, her case was reopened upon the woman’s request, and the review stated that the gynecologist did not have a chance to talk to the patient. The endometriosis was so severe that the patient would not have a chance of natural conception and the cysts should be removed. The review also concluded that new consent forms should have a space in which patients can designate procedures which they do not wish to be done.
According to Brahams (2009), women who awoke finding that they had lost their womb and reproductive organs considered their situation as if they were raped or went under “castration”. Brahams (2009) recommended that there should be “a delayed procedure with renewed consent, albeit with the risks and inconveniences attached to a second operation” (p. 361). In other words, the patient should have time to consult and think about her situation and all information should be provided.
The Sarah Lee Brown case
In 1981, a case involving Sarah Lee Brown and Dr. John Mladineo became the subject of a legal battle over medical malpractice (Justia US Law, 1987). Instead of only the tumor to be removed, Dr. Mladineo made a complete hysterectomy on Ms. Brown (Justia US Law, 1987). After a week of discharge from the hospital, Brown complained of excreting bodily waste by way of her vagina (Justia US Law, 1987). When the doctor was informed of Brown’s complaint, he advised the patient to take a peculiar treatment – drink some vinegar (Justia US Law, 1987). Brown was admitted to the same hospital where Dr. Helen Barnes treated her for rectovaginal fistula, which was caused when Dr. Mladineo performed the surgery and accidentally created a canal in the rectum to the vagina (Justia US Law, 1987). This case should not have happened if there was an adequate informed consent law regulating surgeons before performing hysterectomy.
Comprehensive informed consent law
During the days of slavery in America, black women were subjected to sterilization because they were deemed unworthy to provide offspring. This was known as the “Mississippi Appendectomy”. In the 1950s, black women were provided with contraceptives so that the black population would not grow (University of Maryland, n.d.).
It is a different environment today. A woman’s reproductive decisions are protected under the Fourteenth Amendment of the U.S. Constitution. Court decisions support the principle that reproduction is part of the “very core of human identity” and “reproductive choices are deemed protected rights belonging to the realms of individuality, privacy, and autonomy,” which should not be bypassed by any government agency or regulation (Laufer-Ukeles, 2011, p. 569).
Although Supreme Court jurisprudence states that the right to reproduce includes “the context of contraception, abortion, and the right not to undergo sterilization” (Skinner v. Oklahoma, 316 U.S. 535, 541, 1942 as cited in Laufer-Ukeles, 2011, p. 569), law scholars and practitioners contend that these rights should extend to the areas of reproduction and child bearing decision-making (Laufer-Ukeles, 2011). Birth decision making and procreation are personal choices that are supported by public policy, husbands and wives’ testimonies on the meaning of such choices and the social consequences of those choices.
However, Laufer-Ukeles (2011) argued that reproductive choices are usually made with the influence of a doctor in the hospital, supported by government funding and legislative mistake. The state regulates and controls reproductive choice based on its policy of promoting public health despite the constitutional provision that protects such choices (Laufer-Ukeles, 2011). In a country which has a comprehensive informed consent law, a woman with problems in the reproductive organs is given options to choose. The doctor must explain the various reasons, but the woman must have the final choice. Other states have passed their version of the law. North Carolina enacted the Woman’s Right to Know Act (WRKA) which provides that women should be provided necessary information before they decide to have an abortion (Stam, 2012).
The traditional practice of hospitals is that when a patient is scheduled for surgery, she is made to sign a consent form. The form contains provisions where the surgeon is authorized to perform further surgery where the surgeon thinks necessary. In this case, there should be an open discussion with patient regarding those options that will come out during the surgery. The form should not be over-all consent. The patient can seek redress by asking police assistance or directly go to court (Brahams, 2009).
Alternatives to hysterectomy
Complications in hysterectomy force some in the medical profession to perform alternative treatment and one of these is uterine artery embolization (UAE). According to a study, UAE provides symptomatic relief compared to hysterectomy (Ruuskanen, 2010). There have been positive findings of patient satisfaction for UAE, like shorter time of hospitalization, but the patient has to go through surgical intervention after a few years (Scutiero et al., 2013). UAE is also effective treatment for myoma (Dueholm, Langfeldt, Mafi, Eriksen, &Marinovskij, 2014).
There are other alternatives to hysterectomy provided by the medical profession. For menorrhagia, women are now aware of the other treatment options. Endometrial ablation, which targets the lining of the uterus, is simpler to perform with lesser complications than hysterectomy. The National Heavy Menstrual Bleeding Audit of the Royal College of Obstetricians and Gynecologists and the National Institute for Health and Clinical Excellence (NICE) have advised that women experiencing extreme menstrual bleeding should undergo subsequent invention of ablative trials. NICE reported that ablation as alternative to hysterectomy can improve women’s quality of life. If it still failed, then the patient should be advised to undergo hysterectomy (Gupta &Manyonda, 2014).
A technical innovation that is gaining popularity is the use of uterine manipulator (UM) which is under the classification of minimally invasive hysterectomy (MIH). The doctor moves the uterus by way of the vagina, improving exposure in the pelvis and increasing the length between urethra and the operative field (Zhang et al., 2014). One problem with MIH is when the UM disseminates cancer cells, although this is still a debatable one because of the lack of empirical studies regarding this issue. The surgeon inserts the manipulator which increases intrauterine pressure when the balloon is inflated. This can enhance lymph vascular space invasion (LVSI) or enhance the passage of malignant cells through the fallopian tubes into the peritoneal cavity. Another problem with the UM is that it can disaggregate tumor cells (Zhang et al., 2014).
An alternative to hysterectomy for women with excessive menstrual bleeding (that is not due to cancer, fibroids, or endometriosis) is “balloon ablation” which destroys the endometrium, or uterine lining, but does not involve uterus removal (Harvard Women’s Health Watch, 2009). The principle reflects that of the balloon angioplasty procedure, which also uses a “balloon” to open blocked coronary arteries (Harvard Women’s Health Watch, 2009).
In balloon ablation, a sterile solution is attached to the balloon so that it coincides with the shape of the uterus. Something is placed in the balloon to heat the fluid to 190 degrees Fahrenheit temperature. The heating process lasts for 8 minutes. The purpose of the heating process is to destroy the endometrial tissue that touches the balloon (Harvard Women’s Health Watch, 2009). The final stage consists of deflating the balloon, draining the fluid through the catheter, and removal of the catheter (Harvard Women’s Health Watch, 2009).
Reducing variations in surgery
Doctors can reduce variations in surgeries for ethical and economic reasons. Reducing variation can help a lot of patients and reduce mortality and unwarranted use of resources. Patients can have other choices if the surgery can offer no benefits. McCulloch and colleagues (2013) suggested that patient autonomy can reduce variation. However, reducing variations should be assessed by experts in the health profession who must have a broad and clear interpretation of the facts in a particular case. The doctors involved should conduct further investigation if a proposed hysterectomy case is clear with the patient or not. There should be good evidence to provide a surgical intervention that is effective for such a disease (McCulloch et al., 2013).
Causes of variation include “the need or value, the delivery system factors, local cultural beliefs (both public and professional), and the availability of robust, relevant, and casemix-adjusted data. The decision pathway to surgery can be modified in numerous and complex ways” (McCulloch et al., 2013, p. 1131). Medical reports have noted lower deaths and complications than few decades ago as a result of surgery (Polk, 2012).
Studies suggests that signs for operation are difficult to discern in surgical guidelines and many published materials only point to patient care after the decision for operation has been made (McCulloch et al., 2013). Indications for hysterectomy have been much abused because these were not clear, which means hysterectomies were conducted without substantial reasons or causes why they should be performed (Polk, 2012).
Evidence about the benefits and risks of surgery is significant in the decision to reduce variations but it is not a decisive one. Variation for surgery can be provided if there is no treatment benefit or if there is no identification of best treatment. Some new techniques of surgical practice have been introduced but these are incomplete and slowly implemented, which means there is still lack of evidence for its success (McCulloch et al., 2013).
A Cochrane study on the effects of clinical decision making of passive distribution of review evidence showed that appropriate reduction in surgery rates can be accomplished with the distribution of a bulletin. Educational measures distributed to surgeons doing operations resulted in 9 percent fall in the operation rate. Additionally, shared decision making, which aims to give patients balanced information and a friendly atmosphere to give them the chance to choose the right treatment that fits their values and beliefs, is an ethical priority for the doctor and can reduce unwanted variation in surgery rates (McCulloch et al., 2013).
The principle of informed consent
The principle of informed consent states that doctors and other health professionals should provide information on health risks and treatment options and get their consent to proposed medical procedures from their patients (Laufer-Ukeles, 2011). Women should be legally and humanely advised before undergoing hysterectomy. Without a consent law, it is possible that some physicians will not brief their patients about the complications or treatment alternatives. Passage of a law means reducing threats or health risks and patients are protected from medical malpractice. A comprehensive informed consent law provides that doctors inform women of the parameters and consequences before they give their consent to undergo hysterectomy. Informed consent is provided to enhance patient autonomy (Laufer-Ukeles, 2011).
Mississippi women give their consent for surgical procedure without an informed consent law, which challenges their health and rights as women. With informed consent law, the doctor is mandated to provide information about all treatment options and effects of hysterectomy to a woman who is about to undergo hysterectomy (Streicher, 2013). The doctor should provide all the information and the patient should be the last to decide with the assistance of the doctor. Laufer-Ukeles (2011) suggests that there should be a consensus between the doctor and the patient undergoing hysterectomy. With an informed consent law, the doctor is obliged to discuss with the patient on whether hysterectomy should be performed.
Informed consent is a legal term that lays down the way physicians or surgeons conduct treatment or surgeries on their patients. In the medical profession, physicians are obliged to provide an explanation on the attributes of planned therapeutic action, its diagnosis for treating the infection, its hazards, and options to the anticipated diagnosis (Owens, 2009, p. 34). The law provides for fines and other punishments if physicians diverge from what they are supposed to observe under the law and ethical principles, based on people’s treasured worth of “autonomy” (Berg, Appelbaum, Lidz, & Parker, 2009). When a patient and surgeon enter into an agreement, they are governed with certain rules and ethical practice (Maclean, 2009). This is one ground why such a law should be passed in Mississippi.
The principles of medical law provide that autonomy and consent are related. The focus of informed consent is that the doctor should provide all information as this is important to the patient’s decision whether to have a hysterectomy or not (Maclean, 2009). Autonomy focuses on guiding where one is going, deciding where to go and in what activities to engage. Other studies also supported the autonomy principle in the context of informed consent. Informed consent enhances the patient’s independence. Autonomy also connotes treating an individual with informed consent as opposed to James Taylor’s contention that when a patient is being treated, the well-being of that person is the primary concern (Maclean, 2009).
Autonomy means the patient dictates her life’s direction. For a patient to be autonomous, specifically in her decision to undergo a medical treatment, the doctor should not stop her decision, or control her decision by selecting information about medical options. Otherwise, the doctor would compromise the woman’s decision regarding her medical treatment. All information about other treatment options should be given to her.
Healthcare professionals can refrain from taking over the patient’s autonomy by providing them with all information about the alternative courses of treatment that are at their disposal, including the advantages and disadvantages of those options. Some medical scholars and researchers have recommended reducing variation in surgical procedures, which has ethical and economic effects on surgery rates. Patient autonomy can be elevated, and she can choose to avoid it if there are no benefits to be derived from surgery (McCulloch et al., 2013).
Although attacked on both sides, the principle of informed consent has impacted the medical profession (Laufer-Ukeles, 2011). The concept of providing necessary information and acquiring consent from the woman to be placed under the knife has become a benchmark for change from the traditional protectionist and patriarchal method of treatment and a benchmark for yearning of enhancing women’s rights. There may be shortcomings to this present trend but patients’ rights, hospital ethics, the need to provide appropriate medical information to patients, and the need to acquire patient’s consent are now ordinary procedures in medical institutions, hospitals, clinics, and doctors’ dealings with their patients (Laufer-Ukeles, 2011).
In North America, doctors performed some hysterectomies even if they were not necessary. Investigations were conducted in the United States and Canada, which found that there were unwarranted hysterectomies performed. The medical profession is not united on this medical procedure regarding the reasons for hysterectomies in women (Roos, 2007as cited in Laufer-Ukeles, 2011).
As mentioned, there are minor and serious complications in hysterectomy. The Hippocratic code on medical ethics states that the doctor will treat the patient according to his capability and knowledge but not to hurt or injure the patient. Furthermore, if the patient can have a choice of another method of therapy, it is possible that the mode of therapy is less expensive than surgery (Hippocratic Corpus, 1923; Bhutta, 2004 as cited in Laufer-Ukeles, 2011). The doctor has a big role to play in the woman’s decision, but the doctor can also influence the decision. This, however, depends on the provisions of the informed consent law.
Proponents of women’s autonomy argue that the woman has individual right, more valuable than the right of the fetus. They criticize and want to be free from government regulations and doctor’s intervention on reproductive issues because this comprised women’s autonomy (Laufer-Ukeles, 2011). Others argue that women’s autonomy is weakened because they are discriminated by men. With the principle of informed consent, any doctor who operates on a woman and removes something from the reproductive organ without the patient’s consent, commits an offense like physical injury or coercion (Laufer-Ukeles, 2011).
Patients’ consent is not the only thing necessary, rather, adequate information that can help in the patient’s promulgation of a logical decision should be provided by the doctor. Patients can also refuse any treatment indorsed by the doctor and the doctor can be unethical and may violate the law if he/she refused to provide information regarding the patient’s condition, including other options, risks, and complications because of the treatment (Laufer-Ukeles, 2011, p. 575).
Concerned organizations have provided guidelines, which include a case-to-case risk assessment based largely on the woman’s family history. Perera et al. (2013) conducted a study on women who underwent hysterectomy for the period from 2000 to 2010 and patients who underwent bilateral oophorectomy. The study identified 752,045 women who underwent hysterectomy wherein 403,073 patients had ovarian conservation while 348,972 underwent bilateral oophorectomy. The number of ovary removal has been controlled, particularly on women ages 45 to 49. This is shown in figure 3.
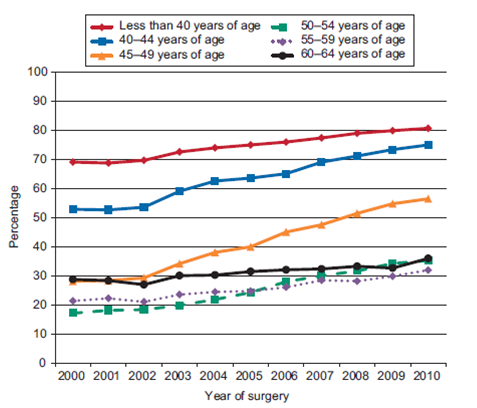
The study of Perera et al. (2013) suggests that ovarian conservation has been increasing. Procedural factors influenced this trend, such as the type of hysterectomy, which influenced the most for retaining the ovaries. Hospital characteristics influenced about 10 percent in the decision to conserve the ovaries, while 5 percent and 3 percent were attributed to patient decisions and physician characteristics, respectively (Perera et al., 2013).
The researchers noted the variation and group the participants according to age and for those who underwent vaginal hysterectomy or not. There were about 2,000 to 10,578 hospitals that admitted and subjected 68,022 women of this latter grouping. The percentage of ovarian conservation registered at 37.2 percent. Hospitals across the United States have chosen to tread along the path of ethical practice by performing hysterectomy and bilateral oophorectomy only on extreme cases. The trend for ovarian conservation is influenced by data collected by hospitals regarding the relationship of oophorectomy and coronary heart disease and possibly mortality (Perera et al., 2013).
Gender identity
A woman’s reproductive system is associated with gender identity. When this is removed by surgical means, the woman loses herself (Elson, 2002 as cited in Senie, 2013). Medical sociologists argue that medical treatments like hysterectomies can affect people’s lives. When a woman undergoes hysterectomy, she loses one part of her identity as a woman and that is menstruation. Medical sociologists contend that monthly period and female femininity are correlated positively (Elson, 2002 as cited in Senie, 2013). Randomized studies that have been conducted indicated that menstruation is highly recognized by women (Senie, 2013).
Menstruation makes women different from men and they just would not like to give it up easily through hysterectomy. Menstrual periods provide an emblematic and substance connection between women. Hysterectomy marks the end of a woman’s menstruation, which disturbs gender identity as this is closely related with womanhood (Martin, 1992 as cited in Senie, 2013).
Quality of Life (QoL)
The process of healing must be in several stages. Although painful as it may be, a woman who undergoes hysterectomy becomes a new individual (Long, 2002 as cited in Bayram & Beji, 2010). Healing stages must be experienced with care and positive attitude. The loss of one part must lead to the recovery of new life’s horizons. Various studies indicated that women who have undergone hysterectomy should develop a new way of looking at life and womanhood.
Nursing care should be planned adequately to correspond to the various stages of the healing process. Specific nursing care should make the patient move from the stage where she was dependent through a stage where she becomes conscious, self-actualizing, and independent (Bayram & Beji, 2010). The first stage should involve the patient to come out of isolation. Breaking free from hiding and numbness and accepting the innermost pains are significant movements that should be followed. Second, the numbness must be resolved and transformed into feeling (Long, 2002 as cited in Bayram & Beji, 2010).
In fact, suffering is a part of life that sometimes cannot be avoided and acceptance of suffering is the best way to reduce the pain. Visits from a mental health nurse or a professional person who can provide meaningful counseling is essential. The next stage is releasing or emptying, which involves dealing with fear and accepting the reality of womanhood (Long, 2002 as cited in Bayram & Beji, 2010). The processes of emptying are in four vital steps:
- The patient must take hold of the pain like a pack of sticks to build a fire.
- The sticks have to be held in an embrace so that the person can move across the room to the fireplace.
- When reaching the fireplace, the individual can release the sticks and let them go.
- After all the steps, the individual feels warmed and happy from the sticks she has thrown out to the fire.
The individual who has undergone hysterectomy must embrace womanhood once again, after she has suffered from the medical event (Long, 2002 as cited in Bayram & Beji, 2010). Studies indicate that one can accept the fact that suffering enables one to admire life, feel compassion for others of the same fate (Bayram & Beji, 2010). A woman who chooses to undergo hysterectomy must learn to endure the pain because this can lead to an improved quality of life (QoL). QoL is multidisciplinary but its definition is not universal as it can be seen from different perspectives (Long, 2002 as cited in Bayram & Beji, 2010).
Hysterectomy can lead to improved QoL if the woman knows how to deal with it, patiently and perseveringly. There are also several notions and concepts which are influenced by culture. The World Health Organization classifies QoL into six broad areas: “physical, psychological, level of independence, social relationship, environment and spirituality, religion, or personal belies” (Bayram & Beji, 2010, p. 4). Each of these areas affects all the others while QoL covers the entirety and wholeness.
The WHO definition highlights life’s goals, expectations, aims and anxieties of individuals as they go on and meet life’s sufferings. Health-related quality of life (HRQL) encompasses the person’s entire well-being. According to international experts, HRQL includes the physical, social, and emotional areas of a person’s functions, including awareness of a person’s quality of life and general life satisfaction (Bayram & Beji, 2010).
Positive and negative effects can be seen on women who undergo hysterectomy. With the loss of fertility, the woman may become anxious and afraid of the many personal issues surrounding her life and her relationships with the people around her, particularly her husband (Bayram & Beji, 2010). Women complained of difficulties in uterine problems, to include physical and menstrual pain, emotional and sexual dysfunctions and the decline in general health.
Summary and Conclusion
This literature survey has explored the advantages and disadvantages in hysterectomy. The empirical studies provided the pros and cons and hysterectomies and the reasons why doctors recommend surgeries. The surgeon should provide the necessary information for the woman to choose what best suits her health. Like any other medical activity or event, doctors have varying views. There were patients who reported of improved life while others had negative feelings about hysterectomy. In other words, the subject needs more empirical studies to substantiate what is in the literature. The presence of informed consent law can also affect the outcomes.
This study will use a theoretical framework known as the health belief model (HBM) to determine problems of behavior. Researchers use HBM to understand and predict how patients apply health prevention and services. HBM begins with a hypothesis that actions pertaining to health are influenced by factors like: the presence of adequate motivation to make problems of health significant; the idea that a person is at risk to a health issue or as a consequence of that health problem, or there is the perception of a health threat; and the belief that observing a doctor’s or a health worker’s recommendation would reduce the health issue at lesser costs (Huber & Tu-Keefner, 2014).
Authors argue that HBM is linked with social cognitive theory (SCT) (Rosenstock, Strecher, & Becker, 2010). King, Singh, Bernard, Merianos, and Vidourek (2012), further expound on the concept of HBM elements, such as apparent benefits, difficulties and indications to action. Individuals exhibit certain behaviors when they feel that:
- benefits are derived in exhibiting the behavior,
- the benefits are greater than the barriers in displaying such behavior, and
- there are clues reminding them to display such behavior (King et al., 2012).
This concept was later modified and combined with Howard’s (1989) model: individuals need a stimulant to enhance their decision-making process, or they need to be motivated with what is known as environmental cue (Risker, 2012). The combination of Howard’s (1989) model and HBM provides explanation of patient behavior relative to the subject of health services. The model further explores that when individuals look for information about their health, the motivation relies on how confident they are in understanding and providing excellent choice with regards their health. Self-belief and experience of an exact choice are relevant when the individual seeks information about availability of health service (Risker, 2012).
King et al. (2012) explained that for individuals to take action to avoid sickness, they have to believe that
- they are vulnerable to the disease;
- the disease can inflict a severe impact on some part of their lives;
- certain behaviors can reduce the severity of the disease whenever the disease inflicts upon them; and
- these behaviors cannot be hindered by aspects like expenses, pain, and humiliation, or the perceived barriers.
HBM has a predictive ability and we can expand this to include the concept of self-efficacy, which is the perception or belief in how competent an individual in possessing certain behavior (Lin, Simoni, & Zemon, 2010).
HBM constructs assert that individuals make decisions based on their beliefs and perceptions. The individuals’ actions relate to surgeries, preventive care, and other form of treatment. HBM can provide explanation on theories regarding the experiences and treatment responses/reactions of Mississippi women who have undergone or will undergo hysterectomies. Some questions that need responses in this instance are: Does the absence of informed consent law affect Mississippi women’s decisions to undergo hysterectomies? Are the women well informed about the causes and complications of hysterectomy? What are the advantages and disadvantages of having informed consent law for Mississippi women?
Methodology
This chapter of the dissertation explains the expected methods for conducting the research. This section will provide the description of various study techniques ranging from data collection method to research strategy. Lastly, this section of the paper also explores the ethical considerations of the research.
Research Design and Rationale
The research questions are:
- What are the perceptions of women who have undergone hysterectomy without prior awareness of comprehensive informed consent?
- What are the new themes that emerge from the lived experiences of women who have undergone hysterectomy in the absence of comprehensive informed consent law?
The central concept of this paper is to understand the influence of informed consent in shaping the lived experiences of women who have undergone hysterectomies. The research tradition for investigating this central concept is to use a qualitative approach for sampling the views of the respondents. The rationale for doing so is that the qualitative approach best samples people’s attitudes and perceptions (Grove & Gray, 2010).
Role of the Researcher
One of the characteristics of the qualitative studies is that it should be repeated by other researchers, under the similar conditions and comparable results attained. The attribute makes the qualitative studies different and the role of the researcher in the process significant (Grove & Gray, 2010). In fact, in qualitative studies, the researchers are considered as part of the data collection instrument. In other words, the researcher plays a critical role in reconciling the data collection process. Essentially, despite the availability of the data collection instruments such as the questionnaire, the data collection process is facilitated by the human mechanism or the researcher (Grove & Gray, 2010).
During the facilitation process, the researcher explains different aspects of the study including the expected biases as well as the assumptions made in the study. Moreover, the researcher describes the study expectations as well as the experiences that qualify the ability to conduct the study (Bound, 2011). In addition, it is critical for the researcher in qualitative studies to keep records that expound the individual reactions, reflections as well as insights concerning the undertaken study.
Besides, the researcher should also be in a position to differentiate whether their role is emic or etic (Bound, 2011). In other words, the researcher acts as an insider who fully participates in the study. On the other hand, an etic role is where the researcher acts as an outsider or a mere objective observer. Nevertheless, in most instances, researchers find themselves acting in both responsibilities (Bound, 2011). Researchers normally begin the interview as an outsider and gradually become a member of the interviewee through appropriate explanation of the study instrument. The reverse case can also occur in which the researcher starts as an emic observer and progressively become an etic participant. Such variations exist in qualitative studies (Bound, 2011).
Studies indicate that a good qualitative researcher has the capability of probing the research questions. The researcher listens, think through the answers from the interview and then delve deeper through probing questions in order to understand more concerning the conversation (Grove & Gray, 2010). The researcher should build a bigger picture using ideas and theories borrowed from diverse sources (Grove & Gray, 2010).
Using the above information, my role as a researcher is to interview the respondents and investigate emerging themes and patterns from their responses. In order to identify the emerging themes and patterns, I will employ various interview tactics to ask probing questions. Moreover, through the application of ideas and theoretical frameworks from a wide variety of sources, I will build a bigger picture in order to be understood by the interviewee and attain the desired answers.
Methodology
Participant selection logic
Even though all women who have undergone hysterectomy in Hinds County, Mississippi qualify to partake of this study, only eight respondents will be randomly selected to participate in this study. The respondents will be selected based on the level of their experiences with hysterectomy as well as their willingness to participate in the study. The random selection procedure is chosen due to its increased capability of minimizing the biases. A face-to-face interview will be administered to the chosen participants through the application of a well-structured interview questionnaire.
The face-to-face interview will address the main points while paying close attention to related issues that are not covered in the questionnaire. In other words, the interviews will be semi-structured, thereby allowing the interviewees to give whatever type of response they wish. Specifically, during the interview the researcher will encourage the respondents to give their lived experiences about hysterectomies. Moreover, during the interview, the researcher will also seek clarification in instances when there are unclear responses.
Instrumentation
Seidman (2012) says that all researchers should adopt prudent ways of collecting data. Particularly, he draws our attention to data collection methods that give respondents the freedom to express themselves (Seidman, 2012). The main data collection instrument in this study is the interview questions. The questions will be open-ended and well-designed in order to capture the main issues in the study while offering flexibilities for the researcher to probe deeper into the responses provided by the respondents (Seidman, 2012).
As indicated, the face-to-face interviews are associated with the risks of the respondents giving false information since the individuals that will be interviewed might be lured to do so (Seidmanr, 2012). In order to avoid the problems, the interview questions will be designed to allow flexibilities for the researcher to provide individual participants with more guidance on what to talk about depending on the observations.
Published data collection instruments
In most health studies, Cochrane risk of bias tool is normally applied in evaluating different research strategies applied by other researchers (Corbett, Higgins & Woolacott, 2013; Higgins, Altman, Gøtzsche, Jüni, Moher & Oxman, 2011). The Cochrane risk of bias tool is one of the various options that can be used to evaluate the published information particularly, the articles that are believed to be containing the required data (Davey, Turner, Clarke & Higgins, 2011; Austin, Manca Zwarenstein, Juurlink & Stanbrook 2010). In fact, various social science studies have also used similar methods in determining the variables in the published data (Vale, Tierney & Burdett, 2013).
However, in this study, NVIVO or the hand coding tool will be used to unveil themes and patterns in the published data (Hague, 2014). The reason is that the methods are accurate and easy to understand compared with the Cochrane risk of bias tool (Hague, 2014). Furthermore, the researchers said the methods for knowledge construction and our understanding of reality should further inform the research strategy. This paper considered these factors when choosing the qualitative research strategy. Furthermore, since the research involves “social” issues, the qualitative research approach would be the best approach.
For researcher developed instruments
Bound (2011) says the qualitative research strategy has several types of designs. They include “inquiry, narrative, phenomenological, participatory action, grounded theory, ethnography, and case study” designs (Bound, 2011, p. 1).
The proposed study will use the phenomenological research design. This design is right for this paper because it focuses on people’s experiences and life conditions (Martyn, 2010; Hague, 2014). Furthermore, it provides researchers with an opportunity to measure the perceptions of those experiences. This way, the phenomenological design will help to distinguish different phenomena, from the respondents’ views, which is how we construct reality. This research design also merges with the main data collection method (interview) because it interprets facts, depending on people’s assertions.
This way, the participants’ subjective opinions provide the framework for forming the research findings. Through this understanding, Bound (2011) argued, “Phenomenology (is) focused on the subjectivity of reality, continually pointing out the need to understand how humans view themselves and the world around them” (p. 1). The main drawback of using the phenomenological research design is the difficulty of preventing researcher bias. Furthermore, since this research design mainly depends on subjective data, it is difficult to guarantee the validity and reliability of the findings obtained (Martyn, 2010).
Procedures for recruitment, participation and data collection
Besides factoring in the interview responses given by the research participants, this study merges theory and data. The theory part would mainly come from the findings obtained from other researchers. Since the quality of theoretical data cannot reliably be assessed from the published reports, amalgamating these findings with raw interview responses would highlight the need to include deductive and inductive approaches in the data analysis (Vale et al., 2013; Mhaskar, Djulbegovic, Magazin, Soares & Kumar, 2012; Senn, 2012; Clement & Buckley, 2011).
Moreover, since interviews outline the main data collection technique, an inductive approach would suffice. This paper chooses the inductive research approach because it can condense raw data into easily comprehensible summaries. Furthermore, this research approach easily establishes the link between the raw data obtained from the interviews and the research objectives. From this process, it is easy to develop a framework for understanding all the different sets of raw data obtained from the interviews. Studies indicate that the general inductive approach provides an easy to use and systematic set of procedures for analyzing qualitative data that can produce reliable and valid findings (Cottrell & McKenzie, 2010).
Some researchers have criticized the inductive research approach for failing to provide a strong analytical focus that can be used to construct a model (LoBiondo-Wood & Haber, 2013). However, this study uses inductive research approach in developing the interview questions because it provides a simple evaluation of direct interview questions. Indeed, many researchers find the inductive approach easier to use than other data analysis methods.
Data analysis plan
Grove and Gray (2010) argued that the best data analysis method should resonate with the nature of the data collected. This chapter has already shown that the interview method is the main data collection technique. This paper will use the thematic data analysis method as the main data analysis tool. It works by picking out unique themes from the responses given by the research participants.
To do so, the themes will represent essential experiences of the respondents. Collectively, these themes would represent abstract concepts of the research questions. Thomas, Nelson and Silverman (2010) asserted that there are two types of themes that would emerge in such kinds of analyses. The first type is the collective theme, which represents unique concepts that represent the views of two, or more, people. The second one is the individual theme, which only applies to the views of one respondent. Both categories would outline the data analysis method.
Issues of Trustworthiness
Since this study uses human subjects, trust issues are bound to emerge. To gain the respondent’s confidence, their names and contacts will be kept anonymous. In other words, all the participants that will take part in the research will remain unidentified. This requirement is important because the research involves investigating the lives of women who have undergone hysterectomies. Some of them would like to keep this information private. Lastly, the study will make sure that the respondents understand that the proposed study will not expose their personal information because it aims to meet academic goals only.
Ethical considerations
Ethics is one of the issues that researchers need to give increased consideration during the study process (Martyn, 2010). Ethics are values or moral obligations the researcher has to observe during the research process. The moral obligations are normally associated with the consent of the participants and confidentiality (Grove & Gray, 2010). Informed consent is the permission of the respondent to take part in the study process (Grove & Gray, 2010).
The researcher has to explain to the respondent the importance of the study and why it is important for the respondents to take part in the study. On the other hand, like in most professional practices, confidentiality is the moral obligation to ensure that the information provided by the respondents is kept private. The information can only be shared in the circumstance that the respondents have provided the permission or when it is so important that it could be used to save the life of the third party (Martyn, 2010). The two important issues will guide the conducts on this study. However, the ethical consideration will primarily focus on the informed consent process.
The informed consent will be guided by three main principles. First, the consent will be provided voluntarily. Second, the participants can withdraw their consent at any given time. Third, in case the participant has withdrawn their consent, they are also free to withdraw the information or data that had already been collected. The researcher will provide full information concerning the study and explain to the respondent the importance of the study and why it is imperative for the respondents to take part in the study (Martyn, 2010). The full information will be provided in order for the participants to make informed decisions about their participation in the study.
The voluntary consent means that the participants will accept to participate in the study in accordance with their values, preferences and wishes (Grove & Gray, 2010). Providing the respondents with an opportunity to participate in the study voluntary is one of the ways through which the researcher will indicate respect for human dignity during the study. In this study, the due process of ensuring that the participants have consented to participate in the study without coercion, undue influence or incentives will be followed to the latter. The informed consent will be detailed and contain all the requirements as indicated in the appendix.
However, before conducting the study, all the procedures will be followed as a minimum requirement of the institution. In other words, ethical requirements including the permission to conduct the study by the institution, provision of consent forms to the participants as well as assurance forms for the protection of the respondents and the information provided will be conducted before the start of the study. Essentially, all the ethics approval process will be undertaken before the commencement of the study in order to protect the researcher and the respondents.
Summary
This chapter describes the methodology for the dissertation. The qualitative research approach will mainly guide the process of data collection and analysis. It describes the research design, instrumentation, and data analysis procedures. Since human subjects will provide information for the study, there will be a keen emphasis on observing all ethical considerations related to their involvement in research.
References
Austin, P. C., Manca A., Zwarenstein, M., Juurlink, D. N., & Stanbrook M. B. (2010). A substantial and confusing variation exists in handling of baseline covariates in randomized controlled trials: a review of trials published in leading medical journals. Journal of Clinical Epidemiology 63, 142–153.
Bayram, G. &Beji, N. (2010). Psychosexual adaptation and quality of life after hysterectomy. Sex Disability, 28(1), 3-13. Web.
Bellamy, R. (2004). An introduction to patient education: theory and practice. Medical Teacher, 6(4), 359-365.
Berg, J., Appelbaum, P., Lidz, C., & Parker, L. (2009). Informed consent: Legal theory and clinical practice. New York: Oxford University Press.
Boosz, A., Lermann, J., Mehlhorn, G., Loehberg, C., Renner, S., Thiel, F.,…Mueller, A. (2011). Comparison of re-operation rates and complication rates after total laparoscopic hysterectomy (TLH) and laparoscopy-assisted supracervical hysterectomy (LASH). European Journal of Obstetrics & Gynecology and Reproductive Biology, 158(1), 269-273. Web.
Bound, M. (2011). Qualitative Method of Research: Phenomenological. Web.
Bower, J., Schreiner, P., Sternfeld, B., & Lewis, C. (2009). Black-white differences in hysterectomy prevalence. The CARDIA study. American Journal of Public Health, 99(2), 300-307. Web.
Brahams, D. (2009). Unwanted hysterectomies. The Lancet, 342(8867), 361.
Brown, J., Sawaya, G., Thom, D., & Grady, D. (2009). Hysterectomy and urinary incontinence: A systematic review. The Lancet, 356(1), 535-539. Web.
Bryman, A., & Bell, E. (2011). Business research methods. New York, NY: Oxford.
Burbank, F. (2009). History of uterine artery occlusion and subsequent pregnancy. American Journal of Roentgenology, 192(6), 1593–1600.
Butt, J. L., Jeffery, S. T. & Van DerSpuy, Z. M. (2012). An audit of indications and complications associated with elective hysterectomy at a public service hospital in South Africa. International Journal of Gynaecology and Obstetrics, 116(2). Web.
Chima, S. C. (2013). Evaluating the quality of informed consent and contemporary clinical practices by medical doctors in South Africa: an empirical study. BMC Medical Ethics, 14(1). Web.
Clement, Z. V., & Buckley, N. (2011). Reporting of randomised controlled trials: before and after the advent of the CONSORT statement. Journal of Clinical Medicine and Research, 3, 28–34.
Cofey, N. (2013). Hysterectomy: Hands off my uterus. New York, NY: Teachers College Press.
Corbett, M. S., Higgins, J. P. T. & Woolacott, F. (2013). Assessing baseline imbalance in randomised trials: implications for the Cochrane risk of bias tool. Research Synthesis Methods, 5(1), 79–85.
Cottrell, R. & McKenzie, J. F. (2010). Health promotion & education research methods: using the five chapter thesis/ dissertation model. Boston, MA: Jones & Bartlett Publishers.
Creswell, J. W. (2013). Qualitative inquiry & research: Choosing among five approaches (3rded). Thousand Oaks, CA: Sage Publications.
Croce, S., Young, R. H. & Oliva, E. (2014). Uterine leiomyomas with bizarre nuclei: a clinicopathologic study of 59 cases. The American journal of surgical pathology, 59(3), 19-24.
Darwish, M., Atlantis, E., Mohamed-Taysir, T. (2014). Psychological outcomes after hysterectomy for benign conditions: A systematic review and meta-analysis. European Journal of Obstetrics & Gynecology and Reproductive Biology, 174(1), 5-19. Web.
Davey, J., Turner, R. M., Clarke, M. J., & Higgins, J. P. (2011). Characteristics of meta-analyses and their component studies in the Cochrane Database of Systematic Reviews: a cross-sectional, descriptive analysis. BMC Medical Research Methodology, 11, 160-163.
DeJohn, P. (2014). Oregon surgery center is pioneer in outpatient hysterectomy. OR manager, 30(8), 29-31.
Diamond, F. (2014). Highmark leads on procedure but other plans slow to follow. Managed care, 23(9), 5-10.
Dueholm, M., Langfeldt, S., Mafi, H., Eriksen, G., &Marinovskij, E. (2014). Re-intervention after uterine leiomyoma embolisation is related to incomplete infarction and presence of submucousleiomyomas. European Journal of Obstetrics & Gynecology and Reproductive Biology, 178, 100-106. Web.
Elmir, R., Schmied, V., Wilkes, L., & Jackson, D. (2012). Separation, failure and temporary relinquishment: Women’s experiences of early mothering in the context of emergency hysterectomy. Journal of Clinical Nursing, 21(2), 1119-1127. Web.
Firouznia, K., Ghanaati, H., Sanaati, M., Jalali, A. H., & Shakiba, M. (2009). Pregnancy after uterine artery embolization for symptomatic fibroids: a series of 15 pregnancies. American Journal of Roentgenology, 192(6), 1588–1592.
Forsgren, C. & Altman, D. (2013). Long-term effects of hysterectomy: A focus on the aging patient. Aging Health, 9(2), 179-187. Web.
Freed, M. M. & Spies, J.B. (2010). Uterine artery embolization for fibroids: a review of current outcomes. Seminars in Reproductive Medicine, 28(3). 235–241.
Freed, M. M. & Spies, J.B. (2010). Uterine artery embolization for fibroids: a review of current outcomes. Seminars in Reproductive Medicine, 28(3). 235–241.
French, M., & Hernandez, L. (2013). Organizational Change to Improve Health Literacy: Workshop Summary. New York, NY: National Academies Press.
Gaudet, M. M., Gapstur, S. M., Sun, J., Teras, L. R., Campbell, P. T, & Patel, A. V. (2014). Oophorectomy and Hysterectomy and Cancer Incidence in the Cancer Prevention Study-II Nutrition Cohort. Obstetrics and gynecology, 34(4), 64-68.
Graaff, A., D’Hooghe, T., Dunselman, G., Dirksen, C., Hummelshoj, L., WERF EndoCost Consortium, &Simoens, S. (2013). The significant effect of endometriosis on physical, mental and social wellbeing: Results from an international cross-sectional survey. Human Reproduction, 28(10), 2677-2685. Web.
Grigore, M., Ilea, C., Terinte, C., Sava, A., & Popovici, R. (2014). Heterologous type of malignant mixed Müllerian tumor of the uterus presenting as a vulvar mass. European journal of gynaecological oncology, 35(4), 458-460.
Grove, S. & Gray, J. (2010). Study guide for understanding nursing research -: building an evidence-based practice. Philadelphia, Pennsylvania: Elsevier Health Sciences.
Gupta, S. & Manyonda, I. (2014). Hysterectomy for benign gynaeological disease. Obstetrics, Gynaecology and Reproductive Medicine, 14(5), 135-140. Web.
Hampton, T. (2014). Use of morcellation to remove fibroids scrutinized at FDA hearings. The Journal of the American Medical Association 312(6), 588.
Higgins, J. P. T., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D. (2011). The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ, 343, 5928.
Huber, J. T. & Tu-Keefner, F. (2014). Health librarianship: an introduction. Santa Barbara, CA: ABC-CLIO.
John, M. M., Malekpour, F., Parithivel, V. & Goyal, V. (2014). Giant pedunculated hemangioma of the liver. The American surgeon, 80(9), 259-260
King, K., Singh, M., Bernard, A., Merianos, A., &Vidourek, R. (2012). Employing the health belief model to examine stress management among college students. American Journal of Health Studies, 27(4), 192-203. Web.
Koleli, I. K., Ozdogan, E., Sariibrahim,B., Ozturk, L. B., & Karateke, A. (2014). Prognostic factors affecting lymph node involvement in cervical cancer. European journal of gynaecological oncology, 35(4), 425-428.
Laufer-Ukeles, P. (2011). Reproductive choices and informed consent: Fetal interests, women’s identity, and relational autonomy. American Journal of Law & Medicine, 37(4), 567-623. Web.
LoBiondo-Wood, G. & Haber, J. (2013). Nursing research: methods and critical appraisal for evidence-based practice. Philadelphia, Pennsylvania: Elsevier Health Sciences.
Maclean, A. (2009). Autonomy, informed consent and medical law: A relational challenge. New York: Cambridge University Press.
Magon, N. & Chauhan, M. (2012). Editoreal. Sutotal hysterectomy: Has it come a full circle? International Journal of Clinical Cases and Investigations, 4(1), 1–4. Web.
Martyn, D. (2010). The Good Research Guide: For Small-Scale Social Research Projects: for small-scale social research projects. London, UK: McGraw-Hill International.
McCulloch, P., Nagendran, M., Campbell, W. B., Price, A., Jani, A., Birkmeyer, J. D., & Gray, M. (2013). Strategies to reduce variation in the use of surgery. The Lancet, 382, 1130-1139. Web.
Mhaskar, R., Djulbegovic, B., Magazin, A., Soares, H. P., & Kumar, A. (2012). Published methodological quality of randomized-controlled trials does not reflect the actual quality assessed in protocols. Journal of Clinical Epidemiology, 65, 602–609.
Miyata, H., Tsuji, N., Jimi, T., Butsuhara, Y., Terakawa, K., & Nagano, T. (2014). Adenosarcoma of the uterine body initially presenting as an interstitial small tumor of the uterus: a case report. European journal of gynaecological oncology, 35(4), 473-476.
Morice, P. Impact of tumor morcellation during the surgical extraction of solid tumors. Bulletin du Cancer, 101(6), 526-527.
Nickson, T. (2014). Prospectus: Women in Mississippi Undergoing Hysterectomies in Absence of Comprehensive Informed Consent Law. Unpublished manuscript, Walden University.
Owens, D. (2009). Informed consent. Journal of the American Society of CLU &ChFC, 51(6), 34-35. Web.
Papadopoulos, M. S., Tolikas, A. C. & Miliaras, D. E. (2010). Hysterectomy current methods and alternatives for benign indications. Obstetrics and Gynecology International, 1(1), 1-10. Web.
Perera, H., Ananth, C., Richards, C., Neugut, A., Lewin, S., Lu, Y., Wright, J. (2013). Variation in ovarian conservation in women undergoing hysterectomy for benign indications. Obstetrics & Gynecology, 121(4), 717-726. Web.
Phung, T., Waltoft, B., Laursen, T., Settnes, A., Kessing, L., Mortensen, P., Waldemar, G. (2010). Hysterectomy, oophorectomy and risk of dementia: A nationwide historical cohort study. Dementia and Geriatric Cognitive Disorders, 30(1), 43-50. Web.
Pinar, G., Okdem, S., Dogan, N., Buyukgonenc, L., &Ayhan, A. (2012).The effects of hysterectomy on body image, self-esteem, and marital adjustment in Turkish women with gynecologic cancer. Clinical Journal of Oncology Nursing, 16(3), E99-E104. Web.
Qamar-Ur-Nisa, H., Memon, F. & Shaikh, T. A. (2011). Hysterectomy: an audit at a tertiary care hospital. The Professional Medical Journal, 18(1), 46–50. Web.
Reis, N., Engin, R., Ingec, M., & Bag, B. (n.d). A qualitative study: beliefs and attitudes of women undergoing abdominal hysterectomy in Turkey. International Journal of Gynecological Cancer, 18(5), 921-928.
Rosenstock, I. M. (1974). Historical origins of the health belief model. Health Education & Behavior, 2(4), 328-335.
Ruuskanen, A., Hippelainen, M., Sipola, P., &Manninen, H. (2010). Uterine artery embolisation versus hysterectomy for leiomyomas: Primary and 2-year follow-up results of a randomized prospective clinical trial. European Radiology, 20(1), 2524-2532. Web.
Saito, S., Kajiyama, H., Miwa, Y., Mizuno, M., Kikkawa, F., Tanaka, S., & Okamoto, T. (2014). Unexpected ovarian malignancy found after laparoscopic surgery in patients with adnexal masses–a single institutional experience. Journal of Medical Science, 76(1-2), 83-90.
Schiavo, R. (2013). Health communication from theory to practice. New York, NY: Jossey-Bass.
Schollmeyer, T., Elessawy, M., Chastamouratidhs, B., Alkatout, I., Meinhold-Heerlein, I., Mettler, L., Weigel, M. (2014). Hysterectomy trends over a 9-year period in an endoscopic teaching center. International Journal of Gynecology and Obstetrics, 126(1), 45-49. Web.
Scutiero, G., Nappi, L., Matteo, M., Balzano, S., Macarini, L., & Greco, P. (2013). Cervical pregnancy treated by uterine artery embolisation combined with office hysteroscopy. European Journal of Obstetrics & Gynecology and Reproductive Biology, 166(2), 104-106. Web.
Seidman, I. (2012). Interviewing as Qualitative Research: A Guide for Researchers in Education and the Social Sciences. New York, NY: Teachers College Press.
Seki, T., Yanaihara, N., Hirata, Y., Fukunaga, M., Tanaka, T., & Okamoto, A. (2014). Uterine endometrial carcinoma with trophoblastic differentiation: a case report with literature review. European journal of gynaecological oncology, 35(4), 461-464.
Senie, R. T. (2013) Epidemiology of women’s health. Boston, MA: Jones & Bartlett Publishers.
Senn, S. (2012). Seven myths of randomisation in clinical trials. Statistics in Medicine, 32, 1439–1450.
Seror, J., Bats, A. S., Douay-Hauser, N., Nos, C., Bensaid, C., & Lecuru, F. (2014). Contributions of laparoscopic and robotic surgery in the treatment of uterine cancer. La Revue du praticien, 64(6), 813-815.
Sheth, S. (2013). Vaginal hysterectomy in women with a history of 2 or more cesarean deliveries. International Journal of Gynecology & Obstetrics, 122(1), 70-74. Web.
Silverstein, D. C., Cozzi, E. M., Hopkins, A. S. & Keefe, T. J. (2014). Microcirculatory effects of intravenous fluid administration in anesthetized dogs undergoing elective ovariohysterectomy. American journal of veterinary research, 75(9), 809-817.
Singh, S., Ryerson, A. B., Wu, M., &Kaur, J. (2014). Ovarian and uterine cancer incidence and mortality in American Indian and Alaska native women, United States, 1999-2009. American Journal of Public Health, 104(S3), S423-S432. Web.
Sirimusika, N., Peeyananjarassri, K., Suphasynth, Y., Wootipoom, V., Kanjanapradit, K., & Geater, A. (2014), Management and clinical outcomes of endometrial hyperplasia during a 13-year period in Songklanagarind Hospital. Journal of the Medical Association of Thailand, 97(3), 260-266.
Sparić, R., Hudelist, G., Berisava, M., Gudović, A., &Buzadzić, S. (2011). Hysterectomy throughout history. ActaChirurgicaIugoslavica, 58(4), 9-14. Web.
Stam, P. (2012). Woman’s right to know act: A legislative history. Issues in Law & Medicine, 28(1), 3-67. Web.
Streicher, L. F. (2013). The essential guide to hysterectomy: advice from a gynecologist on your choices before, during, and after surgery. Boston, MA: Rowman & Littlefield.
Suwannarurk, K., Thaweekul, Y., Mairaing, K., Poomtavorn, Y. & Bhamarapravatana, K. (2014). Silent abnormal placentation linkage to peripartum hysterectomy: Thammasat University Hospital 6-year study. Journal of the Medical Association 97(5), 473-477.
Tapper, A., Hannola, M., Zeitlin, R., Isojärvi, J., Sintonen, H., &Ikonen, T. (2014). A systematic review and cost analysis of robot-assisted hysterectomy in malignant and benign conditions. Journal of Obstetrics & Gynecology and Reproductive Biology, 177(1), 1-10. Web.
Thomas, J. R., Nelson, J. K., & Silverman, S. J. (2010). Research methods in physical activity. Champaign, Ill: Human Kinetics.
Tiwari, V. (2014). Calculating the true cost of robotic hysterectomy. Journal of the Healthcare Financial Management Association 68(8), 80-85. University Press.
Vale, C. L., Tierney, J. F., & Burdett, S. (2013). Can trial quality be reliably assessed from published reports of cancer trials: evaluation of risk of bias assessments in systematic reviews? BMJ, 346, 1798.
Watson, M. E. (2011). Systems approach workbook for health education & program planning. Boston, MA: Jones & Bartlett Publishers.
Wong, C., Jim, M., King, J., Tom-Orme, L., Henderson, J., Saraiya, M.,…Espey, D. (2011). Impact of hysterectomy and bilateral oophorectomy prevalence on rates of cervical, uterine, and ovarian cancer among American Indian and Alaska native women, 1999-2004.Cancer Causes Control, 22(1), 16812-1689. Web.
Woolcott, C., Maskarinec, G., Pike, M., Henderson, B., Wilkens, L., &Kolonel, L. (2009). Breast cancer risk and hysterectomy status: the multiethnic cohort study. Cancer Causes Control, 20(1), 539-547. Web.
Wright, J. D., Tergas, A. I., Burke, W. M., Cui, R. R., Ananth, C. V., Chen, L., & Hershman, D. L. (2014). Uterine pathology in women undergoing minimally invasive hysterectomy using morcellation. JAMA, 312(12), 1253-1255.
Yeh, J., Cheng, H., Hsu, P., Sung, S., Liu, W., Fang, H.,…Chuang, S. (2013). Hysterectomy in young women associates with higher risk of stroke: A nationwide cohort study. International Journal of Cardiology, 168(3), 2616-2621. Web.
Yildirim, Y., Ertas, I. E., Nayki, U., Ulug, P., Nayki, C., Yilmaz, I., Gultekin, E., Dogan, A., Aykas, A., Ulug, S., Ozdemir, A., & Solmaz, U. (2014). En-bloc pelvic resection with concomitant rectosigmoid colectomy and immediate anastomosis as part of primary cytoreductive surgery for patients with advanced ovarian cancer. European journal of gynaecological oncology, 35(4), 400-407.
Yilmaz, O., Korkmaz, M., Jaroszewski, J. J., Yazici, E., Ulutas, E. & Saritas, Z. K. (2014). Comparison of flunixin meglumine and meloxicam influence on postoperative and oxidative stress in ovariohysterectomized bitches. Polish journal of veterinary sciences, 17(3), 493-499
Zhang, C., Havrilesky, L., Broadwater, G., Di Santo, N., Ehrisman, J., Lee, P.,…Valea, F. (2014). Relationship between minimally invasive hysterectomy, pelvic cytology, and lymph vascular space invasion: A single institution study of 458 patients. Gynecologic Oncology, 133(1), 211-215. Web.