Summary
Ventilator-associated pneumonia (VAP) is an infection that is acquired in hospitals. It is considered among the most commonly acquired hospital infections, especially among pediatric patients in the intensive care unit. This infection is diagnosed via empiric therapy, which is considered to be around 50% of the antibiotics used in pediatrics in the intensive care units.
Several studies have been conducted on Ventilator-associated pneumonia (VAP); however, there are no documented facts or findings on the attributable excess length or mortality for patients who have contracted or been infected with Ventilator-associated pneumonia (VAP). Generally, the cost of controlling Ventilator-associated pneumonia (VAP) in health institutions is high due to the nature of remedies that patients require.
Ventilator-associated pneumonia (VAP) surveillance is considered complicated and is addressed using the clinical definitions that were established by the CDC. Several clinical definitions are used to address the infection or control it, for instance, invasive testing, pathogenesis, and educational interventions among others. Furthermore, pathogenesis is conducted among children, but it is not fully understood due to several factors, for instance, immunodeficiency and aspiration, which are considered risk factors. Moreover, educational interventions have been identified as a method that can be used to decrease Ventilator-associated pneumonia (VAP) infection among children.
This is possible by educating children on the importance of adhering to washing their hands. Although this measure can assist in the reduction of Ventilator-associated pneumonia (VAP), especially among children, certain studies have opposed the effectiveness of the measure, for instance, antibiotic cycling studies of pediatric patients. Generally, these studies have not fully supported this measure as a way of effectively controlling or reducing Ventilator-associated pneumonia (VAP).
Basically, health practitioners and professionals should develop precise and consistent approaches that can be used to diagnose pediatric Ventilator-associated pneumonia (VAP). This is important because it will assist in the definition of attributable mortality, pathophysiology, morbidity, and interventions that can be used in preventing Ventilator-associated pneumonia (VAP).
Introduction
Within this chapter, the research problem would be discussed followed by the value of the study and topic rationalization. This particular chapter would give insight on both the topic of the study, which is Ventilator-associated pneumonia (VAP) among neonates. This chapter is concerned with the overview discussion of the research topic (Scheffinit 56).
Literature review
Within this chapter past studies conducted by researchers and past models created relevant to the current study would be discussed and critically reviewed. This particular chapter is very important as it gives an edge in the study below. It provides relevant studies to the research topic and assists in the adequate understanding of the topic. This is important because it prepares a researcher for the research work. It is also important because it may provide guidelines on how to conduct the research based on previous research activities. After all, they act as references (Womer and Waltmire 43).
Research methodology
Within this chapter the research methodology i.e. the research design would be discussed, the factors for an option for qualitative or quantitative would be discussed below. This section would display ways of collecting data that are adopted for the research. There are different types of strategies of research. The type to use for specific research depends on the nature of the data to be collected and the research process (Thompson 78).
Research Analysis
Within this chapter, the data collected would be analyzed and reviewed. Post this chapter the hypothesis created would lead to an accurate result. The information contained in this chapter will depend on the research method used in the collection of data and the nature or quality of data collected (Simms and Sullivan 72).
Recommendation and conclusion
This chapter contains recommendations based on the data collected, results obtained, the analysis, and the information contained in the literature review. The information contained in the literature review will be compared with those in the results and methodology to make reliable conclusions and recommendations (Ramsey and Person 29).
Introduction
Health care allied infections are on the verge of increase in the pediatric intensive care unit. The rigorous use of medical services, along with the immaturity of the immunologic system of neonates admitted within neonatal units tends to increase the risk of developing heart-allied infections. These infections have a vast impact on survival, neonatal morbidity, hospital costs, and the length of stay. ICUs (Intensive Care Units) have come to represent the frequently identifiable source of nosocomial infections in the hospital, with rate of antimicrobial resistance and infection rates several folds being greater than the general hospital settings.
Nosocomial infections are likely to affect up to 30 percent of neonates, and the rates can be more than five times higher within this populace as compared to older children (Pessoa-Silva, Richtmann, Calil, Santos, Costa, Frota, and Wey 772). VAP in a neonate is a form of hospital-acquired pneumonia that occurs among people receiving mechanical ventilation. VAP is a potentially fatal and widespread crisis among mechanically ventilated patients within ICUs. The CDC (Centers for Disease Control and Prevention) defines VAP as an episode of pneumonia in patients who require a device to control or assist respiration via an endotracheal or tracheostomy tube within forty-eight hours prior to the onset of the infection (Garland 629).
VAP is accountable for up to 30 percent of nosocomial infections among NICU patients, and complicates the condition of between 8 and 28 percent of patients getting mechanical ventilation (Badr, Ali, Albanna, Beshir, and Amr 419).
Among the principal factors that predispose to acquiring VAP include poor host factors, lengthened use of mechanical ventilation, lengthened use of invasive procedures and devices, severe underlying illnesses, and inadequate pulmonary toilet. Gram-positive and gram-negative bacteria are the most widespread causative organisms of VAP (Petdachai 724). Although numerous researchers have studied extensively the subject of VAP, there remains a paucity of data on the subject, thus stipulating further research.
Statement of the problem
There has been increased Ventilator-associated pneumonia (VAP) infection in the recent past. Moreover, the number of reported deaths caused by Ventilator-associated pneumonia (VAP) has increased. This has raised the concern among medical researchers and health professionals on the remedies that can be adopted to reduce or control the infection of Ventilator-associated pneumonia (VAP) among patients in the intensive care units. This has led to increased research on the topic, “what are the measures that can be taken to control or reduce Ventilator-associated pneumonia (VAP) infection in hospitals among patients in the neonatal intensive care unit.”
Purpose of the study
Research activities are conducted to provide solutions or recommendations to specific problems in the environment. Generally, health care research is conducted to assist in the improvement of the quality of life and reduction in disease infection among others. This is research on Ventilator-associated pneumonia (VAP). There are several purposes of the research paper, they include the following:
- Analyzing the risk factors for Ventilator-associated pneumonia (VAP) neonatal patients in the intensive care units.
- Discussing Ventilator-associated pneumonia (VAP) infection preventions
- Discussing the diagnosis for Ventilator-associated pneumonia (VAP) infection
- Discussing Ventilator-associated pneumonia (VAP) infection treatment
- Providing recommendations on how to decrease or control Ventilator-associated pneumonia (VAP) infection among neonatal patients
Significance of the study
Medical research activities are conducted to improve the quality of life and provide solutions to various health issues affecting life. There are several causes of infections in the environment. It is through medical research that these causes are addressed and recommendations on how to decrease or control them are presented. Ventilator-associated pneumonia (VAP) is considered the second most common infection among patients in the neonatal and pediatric intensive care units in the hospitals. It is also one of the most prevalent infections in health institutions. Several infections are acquired in hospitals, for instance, Ventilator-associated pneumonia (VAP).
Generally, previous research activities have revealed that this infection has caused several deaths, and control or reduction measures have not been developed to effectively control the infection. Medical professionals have been working towards developing strategies and methods that can be used in controlling and regulating the effects of Ventilator-associated pneumonia (VAP) infection among neonatal patients in the intensive care unit. Similarly, this research aims at researching on the measures that can be adopted to effectively assist in the control or reduction of Ventilator-associated pneumonia (VAP) infection among neonatal patients in the intensive care unit.
Research questions/hypotheses
Review of literature
Ventilator-associated pneumonia (VAP) is one of the most common infections that are acquired in hospitals according to the statistics provided by the Centers for Disease Control and Prevention (CDC). It is an infection that is prone to neonates in the intensive care unit. Generally, this infection is caused within 48 hours among patients who lacks the device, which can be used to control or regulate endotracheal or tracheostomy respiration. This infection has an influence of effect on morbidity, length of stay, costs of hospital or survival (Mercier and Kutch).
Risk factors associated with VAP
Infants who are mechanically ventilated within the NICUs (Neonatal Intensive Care Units) are at a predominantly increased risk of developing VAP. Cernada, Aguar, Brugada, Gutierrez, Lopez, Castell, and Vento document the recognized risk factors as including duration of mechanical ventilations, enteral feeding, use of sedation, and reintubations (56).
According to Apisarnthanarak, Holzmann-Pazgal, Hamvas, Olsen, Fraser VAP is linked to increased intensive care unit and hospital length of stay as well as a high mortality and morbidity rate among neonates (1284). In addition, genetic syndromes, transportation out of pediatric ICU, and reintubation occur as independent risk factors. The etiologic cause of neonatal VAP may differ in proportion to co-morbid conditions, length of hospital stay, and exposition of anti-microbials (Badr, Ali, Albanna, Beshir, and Amr 419).
The development of neonatal VAP is positively correlated with birth weight, gestational age, intubation times, presence of gastrointestinal bleeding, need for transfusion of blood products, and duration of mechanical ventilation.
The risk of VAP emergence increases with the duration of mechanical ventilation, and is expressed in terms of infectious episodes per a thousand ventilator days. Prevalence tends to range between 2.9 and 11.6 per a thousand ventilator days. Neonates who develop VAP may have a sevenfold increase for days on mechanical ventilation, resulting in a two to fivefold increase in the span of stay within the pediatric intensive care unit as well as doubles the general length of stay in the hospital. The annual expenditure on diagnosing and treating neonatal VAP is estimated at $ 2 billion (Pfeifer, Orser, Gefen, McGuinness, Hannon 24AA).
Conducting a study to determine the impact of delay of extubation on the development of VAP, Fischer et al. As in Foglia, Meier, and Elward found that the median delay of extubation likely to cause VAP was 3.7 days (411). Among the patients extubated within the initial three days, merely 4 percent developed VAP, compared to 40 percent of patients intubated longer than a month. Intubated patients tend to have rates of VAP as much as twenty-one times higher than the rates among vitally ill patients not on mechanical ventilators.
Cardiac-related issues, such as cardiopulmonary bypass in combination with hypothermia, surgical trauma, and ischemia-reperfusion injury elicit an intricate, systematic inflammatory response characterized by the release of endotoxin, vascular endothelium, the release of proinflammatory cytokines, and activation of leukocytes (Wheeler, Jeffries, Zimmerman, Wong, Carcillo 393). This complex inflammatory state leads to a transient immune-suppressed state, which increases the threat of hospital-acquired infection, such as VAP among neonates. VAP occurs in nearly 3 percent of neonates undergoing cardiac surgery and has been allied to a longer length of stay in the hospital, and mortality risks within the pediatric cardiac intensive care unit.
However, the irony is that VAP is the most common rationale behind the instigation of pragmatic antibiotics among PICU patients. Antibiotics are the common medications used for the treatment of neonatal VAP because there is a large amount of information on the organisms resulting in neonatal bloodstream infections.
In conducting a study to determine the risk factors and characteristics of VAP among critically ill newborn infants, Badr, et, al found that the duration of mechanical ventilation is highly significantly longer among VAP patients as compared to non-VAP (420). An analysis of radiological and clinical characteristics showed that the presence of penetration in chest X-ray, hypothermia, and mucopurulent discharges from ETT (endotracheal tubes) were considerably more common in VAP patients (Wheeler 395).
According to Foglia et al (417), a relationship exists between VAP and aspiration of oropharyngeal secretions. The principal factor encouraging colonization include PH-altering medications, which provide a conducive environment for the overgrowth of gastric bacteria as well as the feeding tubes that promote bacterial migration. Micro-aspiration of populated secretions occurs owing to inadequate glottic closure in the region of the endotracheal tubes as well as neuromuscular blockage and impairment of cough and mucociliary clearance by sedative agents, particularly in those nursed supine.
Equally, suctioning has been implicated in VAP via direct contamination owing to inadequate handwashing nasopharyngeal suctioning succeeded by endotracheal tube suction and mucosal upset from deep suctioning. Endotracheal tubes colonization develops early after intubation, and suctioning might move the bacteria into the lower airways. Notably, colonization first occurs within the stomach and oropharynx, followed by subsequent colonization within the lower airways, and lastly the endotracheal tubes. This implies that aspiration, as opposed to contaminated equipment, could be implicated in VAP.
Endotracheal intubation is allied to most of the conditions associated with VAP. Because endotracheal tubes exacerbate the tracheal mucosa, obstruct the cough reflex, cause mucosal injury, work as a reservoir for bacteria, they place patients at higher risks. The endotracheal tubes bypass the defensive mechanisms of the nasopharynx, giving bacteria direct entrée to the lower respiratory tract. The pooled secretions can be introduced into the lungs if cuff leak develops, or the cuff of the endotracheal tubes is deflated for repositioning or removal of the tube. The epoch of highest risk is the initial two weeks of endotracheal intubation.
Incidence rates
VAP is a common illness accounting for between 6.8% and 32.2% of health-acquired infections among the neonates (Garland 629). However, little data is available on VAP in NICUs, and there is no exact number of infection rates available. Studies shows that NICU patients portray that pneumonia comprises of 6.8-32.4 percent of nosocomial infections within this populace (Foglia, Meier, and Elward 410; Tripathi, Malik, Jain and Kohli 13). Later studies of VAP have incorporated the revised definitions, and have reported decreased rates of VAP, deeming it complex to ascertain if VAP is under diagnosed or was previously over diagnosed.
The VAP rates in neonatal intensive care units vary by institution as well as birth weight. A cross-sectional study by the Pediatric Prevention Network, which aimed at determining the hospital acquired infections amid fifty children’s hospitals, portrayed that of 43 children’s hospitals returning questionnaires, 19 hospitals reported VAP rates by device days. However, 12 hospitals showed VAP rates by birth weight (Foglia, Meier, and Elward 410).
Diagnosis
The criteria for diagnosing VAP in neonates encompass mechanical ventilation within forty-eight hours of onset of alleged VAP, two or more chest radiographs portraying novel infiltrates, cavitation, pneumatoceles, or consolidation, deteriorating gas exchange with an increase in ventilatory requirements and oxygen, at least three signs and symptoms (Badr, et, al. 419). Other symptoms linked to VAP neonates include tachypnea and hypothermia, whereas purulent tracheal aspirates are a common laboratory finding (Apisarnthanarak, Holzmann-Pazgal, Hamvas, Olsen, Fraser 1286). Use of a customized CPIS (Clinical Pulmonary Infection Score) has improved the clinical diagnosis of VAP.
Modified CPIS is a custom instrument for clinical evaluation of VAP; including five components namely blood leukocytes, oxygenation index, temperature, chest roentgenogram, and tracheal secretions. The discovery for the causative organism in VAP is critical for guiding the suitable therapy because there is strong proof of the unpleasant effects of insufficient experimental treatment on outcome (Badr, et, al. 419).
Accordingly, the diagnosis of VAP in intubated neonate patients proves difficult to confirm. This owes to a lack of specificity of diagnostic imaging, physical examination findings, cultures, and related laboratory tests. The organisms obtained via an endotracheal tube or from the upper airway may be colonizers and at the same time may not represent lower respiratory flora. Equally, pharyngeal flora may contaminate the bronchoscopic samples. Nevertheless, there are major advances in diagnosing VAP by quantitating the proportion of organisms obtained from bronchoalveolar lavage fluid.
Recovered in huge numbers, these organisms are the alleged etiologic agent. However, this technique deems more challenging for diagnosing the VAP newborn disease owing to a dearth in specimens other than the secretions drawn via an endotracheal tube as well as the ease with which neonates are colonized by the organisms transmitted from the surrounding environment or from people they get into contact with. With the aim of performing surveillance, CDC, in 1998, published recommendations that integrated special criteria for infants below the age of one year. Recently, this has been restructured for CDC-sponsored examination studies (Van Nieuwenhoven et al 337).
A clinical criterion that the National Nosocomial infection Surveillance System has recently revised for pediatric patients is used in diagnosing VAP. Bronchoscopic techniques, such as bronchoalveolar lavage, non-bronchoscopic techniques for an instance quantitative ETA (endotracheal aspirate), and protected specimen brushing are employed in most intensive care units. Nations like India employ radiological and clinical criteria in alliance with semi-quantitative ETA within most ICUs.
The challenges with these recommendations are lack of a gold standard against which to contrast the surveillance studies. Other than following year-to-year trends, there is no known diagnostic value for the Center for Disease Control and Prevention surveillance recommendations for neonates (Baltimore 1420). Due to these complexities of diagnosis and scarcity of validation standards, there have been minimal studies of VAP among neonates.
In this context, Apisarnthanarak, et al. has conducted an in-depth research on VAP in preterm neonates (1283). The authors study the epidemiologic features, apparent among infants with VAP, analyze presumed risk factors, and enumerate the microorganisms seemingly responsible for VAP. They highlight that CDC and NNIS descriptions for infants below the age of one year were employed for nosocomial infections, predominantly VAP and bloodstream infections. Afterwards, they state that allied organisms were designated as the organisms drawn from bronchoalveolar lavage or tracheal aspirates.
The major challenge is that, even though CDC definition paper is a commonly used indication for epidemiologic surveillance, it has not been validated for descriptive clinical research or microbial diagnosis. Equally, even though the reference encompasses criteria for pneumonia diagnosis, it has nothing specifically pertaining to VAP.
Although the NNIS guidelines allow for diagnosis of nosocomial pneumonia among infants to be made based on novels or progressive infiltrate as well as separation of respiratory pathogens, infiltrates within the chest radiograph of intubated premature neonates may indicate progression of meconium aspiration, atelectasis, hyaline membrane disease, or early development of bronchopulmonary dysplasia. Apisarnthanarak, et al. articulates that expert review of neonate VAP cases is susceptible to ruling out the other conditions, but this is merely acceptable on faith (1283). Hence, some of the numerous organisms derived from the tracheal aspirates may embody colonization as opposed to the causes of neonatal VAP.
Therefore, although the interesting data from various institutions and individuals may be the initial step in discovering the prime causes of VAP among neonates, there is the need for extensive research to develop the appropriate criteria for diagnosing VAP in neonates.
Etiology
In general, pneumonia is an inflammatory reaction to the uninhibited presence and growth of microorganisms that have plagued the lower respiratory tract. Aspiration is alleged to be the most widespread etiology of VAP. Under given conditions, the pathogenic bacteria inhabiting the gastrointestinal (GI) or oropharynx tract can relocate to the lower airways, causing VAP.
An impairment or absence of these defenses leads to high inoculums of organisms, and pneumonitis ensues.
VAP etiology has been accounted for as being polymicrobial, with Pseudomonas aeruginosa standing as the most common isolated pathogen.
The microorganisms allied to purulent tracheal aspirates within extremely preterm neonates incorporate Enterobacter species, Klebsiella species, Pseudomonas species and Staphylococcus aureus (Apisarnthanarak, Holzmann-Pazgal, Hamvas, Olsen, Fraser 1286).
According to Badr, et, al., aerobic gram-negative bacilli account for approximately 60 percent of VAP cases (419). However, some researchers have found that gram-positive bacteria are becoming progressively more common with S. aureus being a predominant isolate. In a study to determine the risk factors and characteristics of VAP among critically ill newborn infants, Badr, et, al found that the most prevalent organism in VAP patients was Klebsiella, accounting for 34.3 percent, and Pneumococci were the least, comprising of 6.2 percent.
In a study aimed at identifying the underlying pathology in VAP, Richardson, et, al. studied three cases of neonatal VAP and found two cases that occurred within five days of intubation resulted from fully susceptible organisms S. Pneumonia and S. aureus often implicated during the early onset of pediatric VAP, and linked to aspiration of gastric contents (223). The other case, which incorporated late-onset, resulted from a multiply resistant E.coli. This genre of an organism is allied to the late-onset VAP, usually five days after intubation.
The chief isolated pathogens in VAP are frequent antibiotic-resistant opportunistic bacteria. The principal isolated pathogens are opportunistic antibiotic-resistant bacteria, the majority being gram-negative bacilli. The most commonly detected gram-negative bacilli are Acinetobacter stenotrophomonas maltophilia and Klebsiella. The frequently detected gram-positive bacilli are Streptococcus mitis.
Outcomes associated with ventilator-associated pneumonia
Besides its high mortality rates as compared to auxiliary nosocomial infections, VAP is allied to prolonged hospitalization as well as substantial medical costs. As Cernada, Aguar, Brugada, Gutierrez, Lopez, Castell, and Vento assert, VAP has been accounted for an increasing length of stay in hospitals as well as high mortality rates among both adult and pediatric patients (56). The mortality rate among VAP neonates may be as high as 43 percent (Pfeifer, et, al. 24AA).
Richardson, et al. documents a 20 percent mortality rate for infants with VAP as compared with 7 percent among those without (220). Significant morbidity is manifest, from 3.7 to 10.0
Prevention
Preventing VAP is one of life saving initiatives within the health care sector. A better understanding of neonatal VAP as a health care allied infection may result in prevention strategies within neonatal units, thus reducing mortality and morbidity rates associated with these infections. By understanding how neonatal VAP develops, learning to identify those infants at risk, and applying simple but effective preventive measures at the bedside, health care providers hold the prospective to affect a decrease in the increasing rate of neonatal VAP.
Richardson, et al. describes the introduction of a nurse-led VAP surveillance plan as an overall drive toward patient safety as well as reduction of health care related infection (220). In spite of the absence of definite interventions to reduce and prevent VAP, there exists a relatively modest VAP rate of 5.6 per a thousand ventilator days (Richardson, et, al. 223). Increased morbidity is manifest in patients ventilated for longer periods.
Hence, appropriate measures are required in preventing neonatal VAP. Oral cure is one of the designed preventive techniques. In this technique, the oral cavity ought to be consistently suctioned because if secretions are allowed to segregate above the endotracheal tube cuff, microorganisms from the oropharynx remain readily available to be aspirated within the lower respiratory tract. A specially generated endotracheal tube, Hi-Lo Evac endotracheal tube, is available for suctioning subglottic secretions among patients receiving mechanical ventilation.
Methodology/research design
There are different types of research methods that can be used in the collection and analysis of data, for instance, qualitative and quantitative research methods. Furthermore, these methods have sub branches that are used in the collection and analysis of data based on the required information and nature of data to be collected and analyzed. The choice of a research method to use determines the collection of data and analysis of the results and representation of reliable and quality results.
The sources of information to use also depend on the required data. Data can be obtained from primary or secondary sources. Primary sources of information may be time-consuming but it depends on the nature of the data required for the respective study. On the other hand, obtaining information from secondary data is easy because they are readily available for use.
Ventilator-associated pneumonia (VAP) is an infection that is common in most hospitals. This is one of the most common infections in the intensive care units. This is a research paper on Ventilator-associated pneumonia (VAP) infection among neonates. Ventilator-associated pneumonia (VAP) in an infection acquired in hospitals, therefore, the research will use secondary sources of data in the study. Ventilator-associated pneumonia (VAP) infection has been reported in the past in several health care organizations. This information is stored in databases of different hospitals and other researchers have also presented in the respective data in the past.
These sources will be reviewed to obtain the data for analysis. Furthermore, health journals on the prevention, control and determination of hospital-acquired infection will be used in the study to obtain relevant data on hospital-acquired infections such as Ventilator-associated pneumonia (VAP) (Smith and Sirmans 112).
The data on Ventilator-associated pneumonia (VAP) infection will be obtained from different hospitals in different areas. Secondly, data will be obtained from adult and children’s sections in the respective hospitals to determine the group that is prone to the infection in health care organizations. The control methods that have been used by different hospitals in the past to control the hospital acquired infections will also be analyzed to determine the most appropriate and reliable method that can be used in effective reduction (Mercier and Kutch 64).
Data analysis and results
Several journals and research activities conducted by different researchers were reviewed and analyzed. According to the available data from hospitals and researchers, it was evident that Ventilator-associated pneumonia (VAP) is the second largest infection among patients in the intensive care unit.
A diagram illustrating the number of newborns diagnosed with Ventilator-associated pneumonia
According to the diagram represented above, it is evident that the number of patients or individuals diagnosed with Ventilator associated pneumonia has been increasing steadily (Kennington and Myers 123).
A diagram illustrating the percentage of Ventilator-associated pneumonia among neonatal patients in hospitals
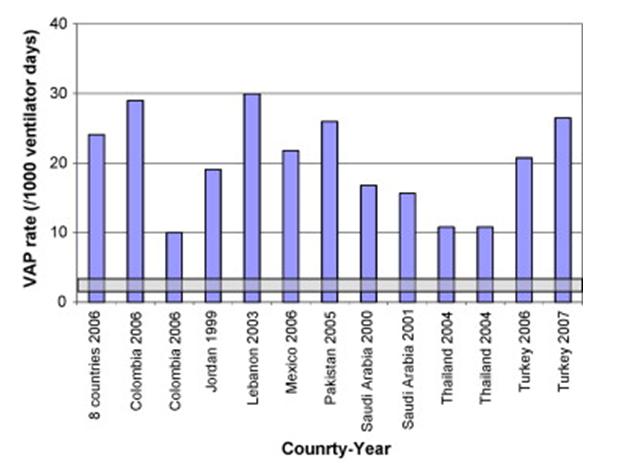
A diagram illustrating Ventilator-associated pneumonia infection among patients in different countries
The above diagram illustrates the number of Ventilator-associated pneumonia (VAP) infection cases reported in hospitals in different countries. According to the diagram, Lebanon reported the highest number of cases in 2003, followed by Colombia in 2006, Turkey in 2007 and Pakistan in 2005 among others (Loesing, Dick and Clemente 28).
Table illustrating Ventilator-associated pneumonia infection in developing countries.
According the diagram represented above, Ventilator-associated pneumonia (VAP) infection is common among developing states compared to developed states. The infection is common in the medical-surgical departments in developing states (Johnson, Fischer and Foster).
Table illustrating the interventions used in controlling and reducing Ventilator-associated pneumonia among patients in developing countries
The diagram above shows the interventions that are increasingly used in controlling or decreasing Ventilator-associated pneumonia (VAP) infection among patients in the intensive care units in developing countries. According to the diagram above, hand washing, educational interventions and other basic methods of controlling or reducing Ventilator-associated pneumonia (VAP) infection is used in developing countries (Sirmans, Mool and Bodganic 29).
Discussion
Health care allied infections are on the verge of increase in the pediatric intensive care unit. The rigorous use of medical services for, along with the immaturity of the immunologic system of neonates admitted within neonatal units tends to increase the risk of developing heart-allied infections. These infections have a vast impact on survival, neonatal morbidity, hospital costs, and the length of stay. ICUs (Intensive Care Units) have come to represent the frequently identifiable source of nosocomial infections in the hospital, with rate of antimicrobial resistance and infection rates several folds being greater than the general hospital settings.
Nosocomial infections are likely to affect up to 30 percent of neonates, and the rates can be more than five times higher within this populace as compared to older children (Pessoa-Silva, Richtmann, Calil, Santos, Costa, Frota, and Wey 772). VAP in neonate is a form of hospital-acquired pneumonia that occurs among people receiving mechanical ventilation. VAP is a potentially fatal and widespread crisis among mechanically ventilated patients within ICUs. The CDC (Centers for Disease Control and Prevention) defines VAP as an episode of pneumonia in patients who require a device to control or assist respiration via an endotracheal or tracheostomy tube within forty-eight hours prior to the onset of the infection (Garland 629).
VAP is accountable for up to 30 percent of nosocomial infections among NICU patients, and complicates the condition of between 8 and 28 percent of patients getting mechanical ventilation (Badr, Ali, Albanna, Beshir, and Amr 419).
Among the principal factors that predispose to acquiring VAP include poor host factors, lengthened use of mechanical ventilation, lengthened use of invasive procedures and devices, severe underlying illnesses, and inadequate pulmonary toilet. Gram-positive and gram-negative bacteria are the most widespread causative organisms of VAP (Petdachai 724). Although numerous researchers have studied extensively the subject of VAP, there remains a paucity of data on the subject, thus stipulating further research.
Etiology
In general, pneumonia is an inflammatory reaction to the uninhibited presence, and growth of microorganisms that have plagued the lower respiratory tract. Aspiration is alleged to be the most widespread etiology of VAP. Under given conditions, the pathogenic bacteria inhabiting the gastrointestinal (GI) or oropharynx tract can relocate to the lower airways, causing VAP.
An impairment or absence of these defenses leads to high inoculums of organisms, and pneumonitis ensues (Won et al 744).
VAP etiology has been accounted as being polymicrobial, with Pseudomonas aeruginosa standing as the most common isolated pathogen.
The microorganisms allied to purulent tracheal aspirates within extremely preterm neonates incorporate Enterobacter species, Klebsiella species, Pseudomonas species and Staphylococcus aureus (Apisarnthanarak, Holzmann-Pazgal, Hamvas, Olsen, Fraser 1286).
According to Badr, et, al., aerobic gram-negative bacilli account for approximately 60 percent of VAP cases (419). However, some researchers have found that gram-positive bacteria are becoming progressively more common with S. aureus being a predominant isolate. In a study to determine the risk factors and characteristics of VAP among critically ill newborn infants, Badr, et, al found that the most prevalent organism in VAP patients was Klebsiella, accounting for 34.3 percent, and Pneumococci were the least, comprising of 6.2 percent.
In a study aimed at identifying the underlying pathology in VAP, Richardson, et, al. studied three cases of neonatal VAP and found two cases that occurred within five days of intubation resulted from fully susceptible organisms S. Pneumonia and S. aureus often implicated during the early onset of pediatric VAP, and linked to aspiration of gastric contents (223). The other case, which incorporated late onset, resulted from a multiply resistant E.coli. This genre of organism is allied to the late onset VAP, usually five days after intubation.
The chief isolated pathogens in VAP are frequent antibiotic-resistant opportunistic bacteria. The principal isolated pathogens are opportunistic antibiotics resistant bacteria, the majority being gram-negative bacilli. The most commonly detected gram-negative bacilli are Acinetobacter stenotrophomonas maltophilia and Klebsiella. The frequently detected gram-positive bacilli are streptococcus mitis.
Outcomes associated with ventilator-associated pneumonia
Besides its high mortality rates as compared to auxiliary nosocomial infections, VAP is allied to prolonged hospitalization as well as substantial medical costs. As Cernada, Aguar, Brugada, Gutierrez, Lopez, Castell, and Vento assert, VAP has been accounted for an increasing length of stay in hospitals as well as high mortality rates among both adult and pediatric patients (56). The mortality rate among VAP neonates may be as high as 43 percent (Pfeifer, et, al. 24AA).
Richardson, et al. documents a 20 percent mortality rate for infants with VAP as compared with 7 percent among those without (220). Significant morbidity is manifest, from 3.7 to 10.0
Ventilator-associated pneumonia (VAP) is a pneumonia that is common among patients who are mechanically ventilated, which develops within 48 hours after placing the respective patients on mechanical ventilations. Ventilator-associated pneumonia (VAP) is an infection, which may cause death if not handled effectively in health care facilities. There are different areas where individuals may acquire infections, for instance, hospital or health facilities among others.
There are several infections that can be acquired in hospitals, for example, Ventilator-associated pneumonia (VAP). Generally, Ventilator-associated pneumonia (VAP) was the second most acquired infection in hospitals according to health statistics collected in the past by medical researchers at the hospital acquired infections. Basically, it is the second most prevalent infection acquired in hospitals, but among patients in the neonatal and pediatric intensive care units.
According to the previous research activities on the prevalence of Ventilator-associated pneumonia (VAP), it was estimated that between 3 and 10 percent of patients in the pediatric intensive care units are vulnerable to be infected by Ventilator-associated pneumonia (VAP). Secondly, the research further revealed that between 6.8 and 32.3 percent of nosocomial infections among NICU patients are pneumonia. Furthermore, it indicated that Ventilator-associated pneumonia (VAP) infection is prevalent among adults than children or teenagers because the reported cases ranged between 15 and 30 percent (Van Nieuwenhoven, Buskens and Van Tiel 213).
The NICU Ventilator-associated pneumonia (VAP) rates are determined by weight at birth and the institution. The findings of the extensive study on Ventilator-associated pneumonia (VAP) are presented in the table below. The data on the National Nosocomial Infection Surveillance (NNIS) are updated annually. However, the most recent presentations that have been analyzed by researchers are those between 2002 and 2004. Generally, the analysis of these data reveals that the rate ranges from 1.4 to 3.5 per 1000 days of ventilator (Won, Chou and Hsieh 105).
Table 1.
There are several research on the infections acquired in hospitals that have been conducted in the past, for instance, in 1998, medical researchers led by the Pediatric Prevention Network conducted study on the infections acquired in hospitals among 50 children’s hospitals. The data of the research were collected via questionnaires. Generally, out of the 50 questionnaires supplied in the hospitals, only 43 were received reporting on the PICU and NICU surveillance data. Generally, 19 hospitals reported device days Ventilator-associated pneumonia (VAP) rates, while 12 hospitals reported stratified Ventilator-associated pneumonia (VAP) rates by weights at birth (See table 1 for more information on the data) (Tejerina et al 58).
There are different types of methods that can be used in research or collection of data. These methods influence the findings presented by individual researchers. The increased reporting cases of Ventilator-associated pneumonia (VAP) among children and adults have been on the rise, which has raised the concern on the methods that can be used to regulate Ventilator-associated pneumonia (VAP) infection in hospitals (Tejerina, Frutos-Vivar and Restrepo 50).
Health care organizations are concerned with the provision of quality health services in the globe. There are several causes of diseases that have compromised the quality of life, for instance, Ventilator-associated pneumonia (VAP). There are several infections that are acquired in hospitals apart from Ventilator-associated pneumonia (VAP). However, Ventilator-associated pneumonia (VAP) is the second largest infection acquired in hospitals.
Basically, health professionals have struggled to develop strategies that can be used in controlling Ventilator-associated pneumonia (VAP) infection among patients in the intensive care unit. There are several strategies that have been designed and tested in different hospitals. These strategies have led to realization of different results, which have led to increased control and decrease of the effects of the infection among neonate patients (Gregory, Herman and Bassett 195).
According to the obtained data from the reviewed sources of information, it is evident that developing states experiences high level of Ventilator-associated pneumonia infection among patients in the intensive care units, especially neonates. This is caused by the substandard nature of health care services in hospitals in developing states. Generally, hospital acquired infections such as Ventilator-associated pneumonia is caused by poor services in hospitals or healthcare organizations. Most developing states are not able to establish quality health care services due to financial strain (Johnson, Fischer and Foster 243).
Risk factors associated with VAP
Infants who are mechanically ventilated within the NICUs (Neonatal Intensive Care Units) are at a predominantly increased risk of developing VAP. Cernada, Aguar, Brugada, Gutierrez, Lopez, Castell, and Vento document the recognized risk factors as including duration of mechanical ventilations, enteral feeding, use of sedation, and reintubations (56).
According to Apisarnthanarak, Holzmann-Pazgal, Hamvas, Olsen, Fraser VAP is linked to increased intensive care unit and hospital length of stay as well as a high mortality and morbidity rate among neonates (1284). In addition, genetic syndromes, transportation out of pediatric ICU, and reintubation occur as independent risk factors. The etiologic cause of neonatal VAP may differ in proportion to co-morbid conditions, length of hospital stay, and exposition of anti-microbials (Badr, Ali, Albanna, Beshir, and Amr 419).
The development of neonatal VAP is positively correlated with birth weight, gestational age, intubation times, presence of gastrointestinal bleeding, need for transfusion of blood products, and duration of mechanical ventilation.
The risk of VAP emergence increases with the duration of mechanical ventilation, and is expressed in terms of infectious episodes per a thousand ventilator days. Prevalence tends to range between 2.9 and 11.6 in every 1,000 days of a ventilator. Neonates who develop VAP may have a sevenfold increase for days on mechanical ventilation, resulting in a two to fivefold increase in the span of stay within the pediatric intensive care unit as well as doubles the general length of stay in the hospital. The annual expenditure on diagnosing and treating neonatal VAP is estimated at $ 2 billion (Pfeifer, Orser, Gefen, McGuinness, Hannon 24AA).
Conducting a study to determine the impact of delay of extubation on the development of VAP, Fischer et al. As in Foglia, Meier, and Elward found that the median delay of extubation likely to cause VAP was 3.7 days (411). Among the patients extubated within the initial three days, merely 4 percent developed VAP, compared to 40 percent of patients intubated longer than a month. Intubated patients tend to have rates of VAP as much as twenty-one times higher than the rates among vitally ill patients not on mechanical ventilators.
Cardiac-related issues, such as cardiopulmonary bypass in combination with hypothermia, surgical trauma, and ischemia-reperfusion injury elicit an intricate, systematic inflammatory response characterized by release of endotoxin, vascular endothelium, release of proinflammatory cytokines, and activation of leukocytes (Wheeler, Jeffries, Zimmerman, Wong, Carcillo 393). This complex inflammatory state leads to a transient immune suppressed state, which increases the threat of hospital-acquired infection, such as VAP among neonates. VAP occurs in nearly 3 percent of neonates undergoing cardiac surgery, and has been allied to longer length of stay in the hospital, and mortality risks within the pediatric cardiac intensive care unit.
VAP is presumed to be allied to additional resource consumption as regards antibiotic administration. However, the irony is that VAP is the most common rationale behind the instigation of pragmatic antibiotics among PICU patients. Antibiotics are the common medications used for treatment of neonatal VAP, because there is a large amount of information on the organisms resulting in neonatal bloodstream infections.
In conducting a study to determine the risk factors and characteristics of VAP among critically ill newborn infants, Badr, et, al found that the duration of mechanical ventilation is highly significantly longer among VAP patients as compared to non-VAP (420). An analysis of radiological and clinical characteristics showed that presence of penetration in chest X-ray, hypothermia, and mucopurulent discharges from ETT (endotracheal tubes) were considerably more common in VAP patients.
A relationship exists amid VAP and aspiration of oropharyngeal secretions. The principal factor encouraging colonization include PH-altering medications, which provide conducive environment for the overgrowth of gastric bacteria as well as the feeding tubes that promote bacterial migration. Micro-aspiration of populated secretions occurs owing to inadequate glottic closure in the region of the endotracheal tubes as well as neuromuscular blockage and impairment of cough and mucociliary clearance by sedative agents, particularly in those nursed supine.
Equally, suctioning has been implicated in VAP via direct contamination owing to inadequate hand washing nasopharyngeal suctioning succeeded by endotracheal tube suction and mucosal upset from deep suctioning. Endotracheal tubes colonization develops early subsequent to intubate, and suctioning might move the bacteria into the lower airways. Notably, colonization first occurs within the stomach and oropharynx, followed by subsequent colonization within the lower airways, and lastly the endotracheal tubes. This implies that aspiration as opposed to contaminated equipment could be implicated in VAP.
Endotracheal intubation is allied to most of the conditions associated with VAP. Because endotracheal tubes exacerbate the tracheal mucosa, obstruct the cough reflex, cause mucosal injury, work as a reservoir for bacteria, they place patients at higher risks. The endotracheal tubes bypass the defensive mechanisms of the nasopharynx, giving bacteria direct entrée to the lower respiratory tract. The pooled secretions can be introduced into the lungs if cuff leak develops, or the cuff of the endotracheal tubes is deflated for repositioning or removal of the tube. The epoch of highest risk is the initial two weeks of endotracheal intubation. These risk factors require effective strategy to enhance quality of health care services in hospitals.
Recommendations and conclusion
There has been an increase in the number of Ventilator-associated pneumonia (VAP) infection cases among neonates in the intensive care units in most hospitals globally. This has led to the extensive research on the methods that can be used to control or regulate the increased infection among patients in the intensive care units.
Although Ventilator-associated pneumonia (VAP) is a serious infection that is common among patients in hospitals and acquired in hospitals, it can be controlled or regulated using several health care recommendations that have been offered by the American Thoracic Society and Centers for Disease Control and Prevention (CDC). There are several guidelines that have been published by these two organizations on the prevention and control of Ventilator-associated pneumonia (VAP). Basically, there are several studies that have been conducted on the efficiency of these guidelines on the reduction and control of Ventilator-associated pneumonia (VAP) infection in hospitals. The studies on the efficiency of these methods have shown the positive impact of the guidelines in the reduction and control of Ventilator-associated pneumonia (VAP) infection among neonates in hospitals.
Basically, the published guidelines bring together several strategies, which are enjoined into a bundle to assist in the reduction of Ventilator-associated pneumonia (VAP) infection. The bundle brings together diverse evidence-based practices, which can be used individually to improve care among neonates. Therefore, considering the results of these guidelines, it is recommendable to apply them in the process of regulating or controlling Ventilator-associated pneumonia (VAP) infection among neonates in hospitals in the intensive care units (Benedict, Hicks and Jeffries 274).
Diagnosis
Ventilator-associated pneumonia (VAP) infection is common among patients in the intensive care unit. This infection is acquired in the hospital and has caused deaths among patients. Hospitals should provide quality health care services to ensure safety of individual patients within health organizations. It is a common knowledge among health professionals that Ventilator-associated pneumonia is the second most common hospital acquired infection in the globe.
However, there are several strategies that have been adopted in the past to control the infection of this infection, which have helped in decreasing or controlling the infection, for instance, diagnosis. Diagnosis is provided to both adults and children and the nature of diagnosis for adults differs from those offered to children. These diagnoses have assisted several health organizations in controlling Ventilator-associated pneumonia; therefore, health organizations should consider developing or establishing policies that provides mandatory diagnosis for patients within the intensive care units to protect them against Ventilator-associated pneumonia infection (Jones, Driscoll and Johnson 217).
Table illustrating Ventilator-associated pneumonia (VAP) in children and adults.
Prevention
Preventing VAP is one of life saving initiatives within the health care sector. A better understanding of neonatal VAP as a health care allied infection may result in prevention strategies within neonatal units, thus reducing mortality and morbidity rates associated with these infections. By understanding how neonatal VAP develops, learning to identify those infants at risk, and applying simple but effective preventive measures at the bedside, health care providers hold the prospective to affect a decrease in the increasing rate of neonatal VAP.
Richardson, et al. describes the introduction of a nurse-led VAP surveillance plan as an overall drive toward patient safety as well as reduction of health care related infection (220). In spite of the absence of definite interventions to reduce and prevent VAP, there exists a relatively modest VAP rate of 5.6 per a thousand ventilator days (Richardson, et. al. 223). Increased morbidity is manifest in patients ventilated for longer periods.
Hence, appropriate measures are required in preventing neonatal VAP. Oral cure is one of the designed preventive techniques. In this technique, the oral cavity ought to be consistently suctioned because if secretions are allowed to segregate above the endotracheal tube cuff, microorganisms from the oropharynx remain readily available to be aspirated within the lower respiratory tract. A specially generated endotracheal tube, Hi-Lo Evac endotracheal tube, is available for suctioning subglottic secretions among patients receiving mechanical ventilation (Baltimore 1420).
Hospital-acquired infections are common in hospitals due to laxities among health professionals. However, this can be controlled or prevented. Several prevention strategies have been used in the past to prevent the increased infection of such infections among patients, especially in the intensive care unit. These prevention strategies should be adopted and improved to enhance the possibility of decreasing or controlling the increased ventilator-associated pneumonia among patients being one of the most prevalent hospital acquired infections in the globe (Benedict, Hicks and Jeffries 315).
Bundle approach
According to the health records and statistics collected in 2004, several health organizations were challenged by the Institute of Healthcare Improvement to develop and establish strategies that would lead to life-saving practices in hospitals and control or reduce the increased hospital-acquired infection such as Ventilator-associated pneumonia (VAP) among others. The strategy aimed at saving more than 100,000 lives in health care organizations by mid-2006.
Several evidence-based guidelines were to be implemented by healthcare organizations to assist in the achievement of the goal and objective of the program. The following guidelines were successfully applied towards the decreased hospital-acquired infection among patients in the intensive care unit. These strategies led to the decreased infection of hospital-acquired infections in the targeted healthcare organizations. Therefore, these guidelines should be adopted to assist in the reduction of Ventilator-associated pneumonia (VAP) infection among neonates (Meuchel, Herman and Peterson 179).
- Decreasing the intubation of endotracheal and mechanical ventilation duration when necessary
- Maintaining oral care
- Maintaining hand hygiene
- Maintaining the elevation of head-of-bed at 30 degrees to 45 degrees
- Avoiding neuromuscular block and heavy sedation with cough reflexes depression
- Preventing the entry of condensate tubing in the tract of lower respiratory
- Maintaining the pressure of endotracheal at 20 cm greater
- Decreasing the hospital-acquired sinusitis risks using orogastric and orotracheal tubes
This is one of the approaches that have been used by several hospitals and health organizations in the past to reduce or control Ventilator-associated pneumonia (VAP) infection among patients in the intensive care units. This has assisted several hospitals in effectively controlling the infection and improving the quality of life among patients in the intensive care units. There are several healthcare organizations or hospitals that have successfully applied the strategy in controlling Ventilator-associated pneumonia (VAP) infection among neonates, for instance, Vanderbilt and Boston Children’s Hospital. The strategy involved education on hand washing and its importance among others. Therefore, considering the results of the strategy, it should be used in improving the quality of life among neonates (Baldwin and Brown 85).
Table illustrating the summary of interventions that can be taken to control Ventilator-associated pneumonia (VAP) infection.
Several infections are acquired in hospitals. Basically, these infections are acquired due to the conditions prevailing in health organizations or hospitals. Management and health professionals should ensure that safe and healthy conditions are provided in all departments within the hospital. Although several infections are acquired in hospitals, the most common department that is prone to hospital-acquired infections is the intensive care unit due to the nature of attention the patients in the respective department require. There are several infections that patients in the intensive care unit may acquire, for instance, Ventilator-associated pneumonia (VAP).
Ventilator-associated pneumonia (VAP) is the second most common hospital-acquired infection among patients in the intensive care unit. This infection has compromised the quality of life of patients within the health care organizations and affected quality health care provision among patients (Booker and Keith 185).
Several strategies have been used by different hospitals to reduce or control Ventilator-associated pneumonia (VAP) infection among patients in the intensive care units. These strategies have yielded different results to individual health organizations. However, these strategies should be used jointly to ensure increased control and reduction of Ventilator-associated pneumonia (VAP) infection among patients in the health care organizations.
This will assist in improving the quality of health services and decrease deaths associated with Ventilator-associated pneumonia (VAP) infection. The use of diagnosis is a strategy that hospitals should develop to assist in the reduction and control of Ventilator-associated pneumonia (VAP) infection among patients. Generally, Ventilator-associated pneumonia (VAP) infection affects children and adults differently; therefore, diagnosis strategy for both adults and children should be developed to ensure appropriate diagnosis for adults and children. Basically, the development of effective and appropriate diagnosis for both adults and children will assist hospitals reduces and controlling Ventilator-associated pneumonia (VAP) infection (Benedict, Hicks, and Jeffries 276).
Implementation of the bundle approach among hospitals will be important too because it will assist in effective control and reduction. The bundle approach is an effective strategy to adopt in the control and reduction of Ventilator-associated pneumonia (VAP) infection because it incorporates different methods or approaches in controlling and decreasing Ventilator-associated pneumonia (VAP) infection.
The strategies incorporated in the bundle approach may not be effective if used single-handedly but the collective implementation of the strategies as a single approach can be useful in controlling and decreasing Ventilator-associated pneumonia (VAP) infection among patients in the intensive care units. Bundle approach incorporates the use of educational interventions and hygiene maintenance among others (Gregory, Herman, and Bassett 419).
According to Badr et al(420), several people do not understand Ventilator-associated pneumonia (VAP) infection and control measures that can be taken. Therefore, the educational intervention will enhance a better understanding of individuals on the infection of patients in the intensive care units, how to detect and control the respective infections. Provision of education on hospital-acquired infections is important because certain individuals are not aware of any infections that are acquired in hospitals. Basically, the infections that are acquired in hospitals are due to laxities or ineffective handling of patients and treatment procedures in hospitals.
Therefore, it is true that Ventilator-associated pneumonia (VAP) infection is common among neonates in hospitals. It is also one of the most common infections acquired in hospitals. Hospital-acquired infections are caused by inappropriate procedures in the treatment process. The development of strategies such as the bundle approach and diagnosis can be useful in controlling or reducing the infection since it is almost impossible to completely eradicate the infection in hospitals (Jones, Driscoll, and Johnson 318).
According to Apisarnthanarak et al, (1288), Preventing VAP is one of the life-saving initiatives within the health care sector. A better understanding of neonatal VAP as a health care allied infection may result in prevention strategies within neonatal units, thus reducing mortality and morbidity rates associated with these infections. By understanding how neonatal VAP develops, learning to identify those infants at risk, and applying simple but effective preventive measures at the bedside, health care providers hold the prospective to affect a decrease in the increasing rate of neonatal VAP.
Ventilator-associated pneumonia is prevalent in developing states. This is due to the standards of health care services in the respective states. The health care services in developing states are low, which has contributed to the increased Ventilator-associated pneumonia infection among hospitals. Basically, Ventilator-associated pneumonia is one of the infections that are acquired in hospitals. This infection is acquired due to poor or substandard services in the intensive care units among hospitals. Therefore, developing states should develop their healthcare institutions to assist in the reduction and control of Ventilator-associated pneumonia infection among patients in the Intensive Care Unit (ICU). Generally, they will require financial aid due to the financial strain experienced in such states.
Works Cited
Apisarnthanarak, Anucha, Galit Holzmann-Pazgal, Aaron Hamvas, Margaret Olsen, Victoria Fraser. ‘Ventilator-Associated Pneumonia in Extremely Preterm Neonates in a Neonatal Intensive Care Unit: Characteristics, Risk Factors, and Outcomes’. Pediatrics, 112.6 (2003): 1283-1289. Print.
Badr, Mohamed, Yasser Ali, Ehab Albanna, Mohamed Beshir, and Gahda Amr. ‘Ventilator Associated Pneumonia in Critically-Ill Neonates Admitted To Neonatal Intensive Care Unit, Zagazig University Hospitals’. Iranian Journal of Pediatrics. 21.4 (2011): 418-424. Print.
Baldwin, Gordon and Daisy Brown. Ventilator-associated pneumonia infection: Intensive Care Unit (ICU). London: Cengage Learning, 2009. Print.
Baltimore, Robert. The difficulty of diagnosing ventilator-associated pneumonia. Pediatrics 112 (2003): 1420. Print.
Benedict, Samantha, Samantha Hicks and Valerie Jeffries. Ventilator-associated pneumonia infection. New York: Norton & Company, Inc, 2009. Print.
Booker, Mark and Calvin Keith. Ventilator-associated pneumonia infection, risk factors and control methods. New York: Willian Heinemann Limited, 2008. Print.
Cernada, Maria, Marta Aguar, Maria Brugada, Antonio Gutierrez, Jose Lopez, Marta Castell, and Maximo Vento. Ventilator-associated pneum, onia in newborn infants diagnosed with an invasive bronchoalveolar lavage technique. Pediatric Critical Care Medicine. 14.1 (2013): 55-61. Print.
Foglia, Elizabeth, Mary Meier, and Alexis Elward. Ventilator-Associated Pneumonia in neonatal and pediatric intensive care unit patients. Clinical Microbial Reviews. 20.3 (2007): 409-425. Print.
Garland, Jeffery. Strategies to prevent Ventilator-Associated Pneumonia in Neonates. Milwaukee: Elsevier Inc., 2010. Print.
Gregory, Megan, Peter Herman and Nyla Bassett. Ventilator-associated pneumonia control and reduction. New York: Anchor Books, 2011. Print.
Johnson, Phyllis, Patricia Fischer and Lavoris Foster. Health Issues in developing states: Ventilator-associated pneumonia. London: John Wiley & Sons, Inc, 2011. Print.
Jones, Sam, Ronald Driscoll and Melissa Johnson. Ventilator-associated pneumonia: Control methods. New York: ACM Press, 2008. Print.
Kennington, Elizabeth and Daniella Myers. Ventilator-associated pneumonia infections. New York: John Wiley & Sons, Inc, 2012. Print.
Loesing, Brock, Joseph Dick and Morgan Clemente. Ventilator-associated pneumonia in developing countries. New York: John Wiley & Sons, Inc, 2007. Print.
Mercier, Shannon and Roxanne Kutch. Hospital acquired infections: Ventilator-associated pneumonia. Chicago: Yale University Press, 2010. Print.
Meuchel, Cynthia, Peter Herman and Daniella Peterson. Ventilator-associated pneumonia: Control Measures. London: Cengage Learning, 2011. Print.
Pessoa-Silva, Carmem Lúcia, Rosana Richtmann, Roseli Calil, Rosana Santos, Maria Costa, Ana Frota, and Sergio Wey. Healthcare-Associated Infections among Neonates in Brazil. Infection Control and Hospital Epidemiology. 25.9 (2004): 772-777. Print.
Petdachai, Witaya. Ventilator-Associated Pneumonia in a Newborn Intensive Care Unit. Southeastern Asian Journal of Tropical Medicine Public Health 35.3 (2004): 724-729. Print.
Pfeifer, Laura, Lynn Orser, Carmelit Gefen, Robin McGuinness, and Carla Hannon. Preventing Ventilator-Associated Pneumonia. The American Journal of Nursing. 101.8 (2001): 24AA+24CC+24EE+24GG+24HH. Print.
Ramsey, Joshua and Tiffany Person. Research methods and strategies. New Jersey: Adventure Works Press, 2011. Print.
Richardson, M, Sarah Hines, Garth Dixon, Lorraine Highe, and Joe Brierley. Establishingnurse-ledventilator-associatedpneumoniasurveillancein pediatric intensive care. Journal of Hospital Infection. 75 (2010): 220-224. Print.
Scheffinit, Clinton. Research Techniques. London: Cengage Learning, 2009. Print.
Simms, Aaron and Sean Sullivan. Research protocols and techniques. Oxford: Oxford University Press, 2008. Print.
Sirmans, Tanya, Joshua Mool and Marcele Bodganic. Risk factors in Ventilator-associated pneumonia infection. Cambridge: Cambridge University Press, 2008. Print.
Smith, Tyrisha and Keith Sirmans. Ventilator-associated pneumonia. Oxford: Oxford University Press, 2009. Print.
Tejerina, Eva, Frutos-Vivar, Fernando, et al. “Incidence, risk factors, and outcome of ventilator-associated pneumonia.” J.Crit Care (2006): 56-65. Print.
Thompson, Brandon. Research Methods. Chicago: Yale University Press, 2011. Print.
Tripathi, Shalini, G.K. Malik, Amita Jain and Neera Kohli. Study of ventilator associated pneumonia in neonatal intensive care unit: characteristics, risk factors and outcome. Internet Journal of Medical Update. 5.1 (2010): 12-19. Print.
Van Nieuwenhoven, C A, et al. “Relationship between methodological trial quality and the effects of selective digestive decontamination on pneumonia and mortality in critically ill patients.” JAMA (2001): 335-340. Print.
Wheeler, Derek, Howard Jeffries, Jerry Zimmerman, Hector Wong and Joseph Carcillo. Sepsis in the Pediatric Cardiac Intensive Care Unit. World Journal for Pediatric and Congenital Heart Surgery. 2.3 (2011): 393-399. Print.
Womer, Wiliam and Scott Waltmire. Research techniques and Principles. New York: ACM Press, 2009. Print.
Won, Sau-Pin, et al. “Handwashing program for the prevention of nosocomial infections in a neonatal intensive care unit. Infect.” Control Hosp. Epidemiol (2004): 742-746. Print.