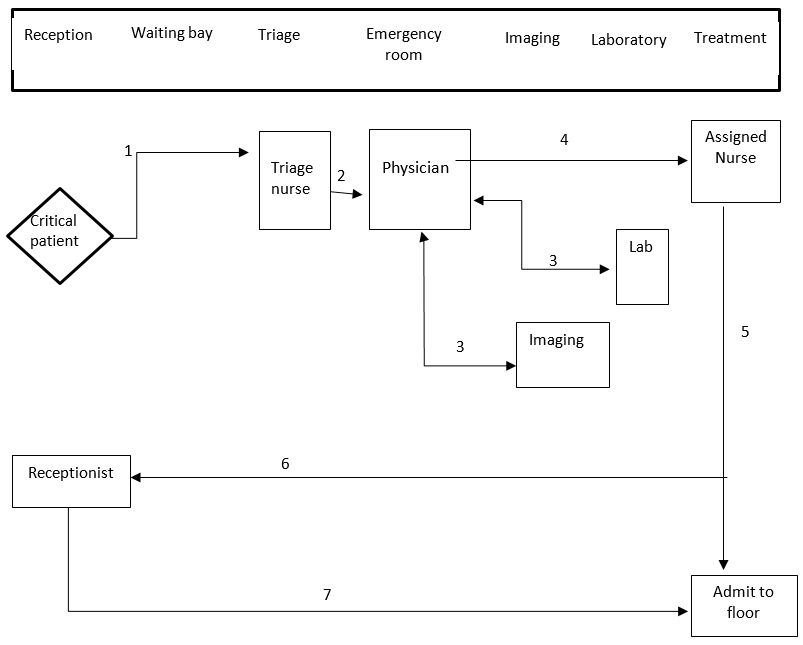
Key:
- Critical patient taken to triage.
- Taken to physician.
- Either taken to lab or image.
- Assigned nurse upon getting from either lab or image.
- Admitted or discharged.
Enhancing medical facility workflow by its management enables nurses to find it simpler to guarantee that each patient’s relevant patient information is readily available at the time of treatment. It is because the nurses will have faster access to the information. It guarantees that all client data is safely stored and, hence, not distorted and up-to-date while being constantly accessible to facilitate decisions regarding medical treatment (Peacock et al., 2022). Nurses will utilize this data to guide medical treatment decisions. It is critical to fine-tune hospital procedures to minimize redundancies that waste hospital resources, delay medical care, and limit patient throughput (McGonigle & Mastrian, 2017). It has been established that excellent workflow management may simplify operations, reduce the chance of mistakes in medical treatment, ensure compliance with industry rules, and improve the quality of care provided to patients.
Yes, it is possible to migrate away from paper-based medical records and replace them with clinical information systems. Nevertheless, this will result in a considerable shift in the information environment in which hospital physicians operate. Clinical information systems are designed for use in settings associated with critical care, such as intensive care units. It can communicate with a number of the hospital’s systems, such as the radiology and pathology departments (Xiao et al., 2018). It brings together these different systems into a unified electronic patient record, which medical professionals can view directly from the patient’s hospital bed. Physicists would be able to draw more precise and speedy conclusions with this information.
Before a new system can be implemented appropriately, a detailed strategy must first result from careful thought. It will be easier to guarantee that everything goes according to plan and that the project is successful if a strong and diverse implementation team is assembled (McGonigle & Mastrian, 2017). The informatics nursing expert (INS), who will be in charge of implementation, is a vital member of the team and will play a crucial part in formulating such a strategy. The INS will also be in charge of implementing the plan after being developed. Organizational solid support, a visible leadership team, and clearly stated procedures and workflows are two essential components that contribute to a successful conclusion. Both of these elements are required for success. Upon developing an appropriate strategy and being ready for implementation, the INS will move on to the next step: establishing educational opportunities.
Before the launch, it is essential to offer end-users appropriate training and exposure to the system. Inadequate training can lead to issues once the system has been implemented, negatively affecting the workers. Implementing new technologies without providing enough staff training before product releases may decrease patient satisfaction during and after the adoption process. Once both the system and the system’s end-users are ready for launch, enough help must be provided for the system’s deployment. Increase end-user acceptance and adoption of the system by ensuring that appropriate resources, such as super-users and support teams, are immediately available to resolve any problems during the go-live phase. Ineffective assistance for physicians to properly adopt a new system can also result in skepticism, discontent, and slow adoption of the new system.
Collecting feedback is one of the most critical components of a successful implementation strategy. The system’s quality should be examined to verify that it satisfies the user, that the information is accurate and can be accessed, that the service offered is of higher quality, and that there are net advantages (Peacock et al., 2022). In several studies, gathering feedback during the installation of new systems may assist in the expansion of software capabilities and the encouragement of buy-in from end-users, which ultimately results in a higher level of acceptability. End-users frequently have unique information and insights regarding how to enhance operations. These can help generate system upgrades, which support continuous improvement.
References
McGonigle, D. & Mastrian, K. (2017). Nursing informatics and the foundation of knowledge (4th ed.). Jones & Bartlett
Peacock, W., Kipper, S., & Neath, S. X. (2022). Stethoscope hygiene, workflow, and patient safety: The crux of healthcare-associated infections. Antimicrobial Stewardship & Healthcare Epidemiology, 2(S1), s55-s56.
Xiao, C., Choi, E., & Sun, J. (2018). Opportunities and challenges in developing deep learning models using electronic health records data: a systematic review. Journal of the American Medical Informatics Association, 25(10), 1419-1428.