Literature Review
Electronic health record (EHR) is an application of information technology in the collection, storage, retrieval, and utilization of data derived from patients or the general population. Hayrinen, Saranto, and Nykanen (2008) define EHR as “a means of repository of patient data in a digital form, stored, and exchanged securely, and accessible by multiple authorized users” (p. 294). Digital data is versatile and accessible, hence increases effectiveness and efficiency of record keeping in hospitals or clinics.
In the age of information technology, the health care systems across the world are gradually adopting and applying information technology in various facets of health care. EHR is one of the ways that the health care systems have integrated information technology into their systems (Vest, Yoon, & Bossak, 2012).
Given that the health care systems advance in increasing efficiency and effectiveness of their system, EHR provides a means of streamlining collection, storage, retrieval, and use of data from patients or the general population. Ideally, application of EHR in hospitals and clinics enables integration of information technology into health care systems. Therefore, this literature review seeks to examine the importance of information technology in healthcare by comparing paper-based medical records and EHR.
Application of information technology in the health environments has prompted many health care institutions such as hospitals and clinics to integrate EHR in their storage, retrieval, and utilization of information. The manual and cumbersome process of record keeping has been a problem in paper-based medical records for years. The emergence of information technology has compelled healthcare institutions to adopt and integrate it into record keeping.
Himmelstein, Wright, Woolhandler (2009) argue that adoption and application of EHR in healthcare is a means of increasing efficiency of record keeping and analysis of data in healthcare institutions. Hence, EHR is important in record keeping because it promotes accessibility of remote records, which would otherwise be inaccessible manually. Bisbal and Berry (2009) argue that healthcare institutions generate huge volumes of data distributed in various departments and sections like clinics and hospitals, which require different users to access. In this view, adoption and application of EHR is the important for it does not only reduce paper-based medical records, but also enhances accessibility of data by multiple users within a given health institution.
EHR has considerable significance in healthcare institutions because it improves quality of healthcare and outcomes of patients. According to Poissant, Pereira, Tamblyn, and Kawasumi (2005), for hospitals to improve the quality of healthcare and guarantee safety of patients, they should integrate information technology in record keeping. Poor keeping of medical records contributes to medical errors that normally occur in healthcare institutions.
Since paper-based medical records are susceptible to errors, they have led to the occurrence of medical errors. On this basis, Bisbal and Berry (2009) agree that integration of information technology in healthcare records will not only increase efficiency, but also reduce the occurrence of medical errors. Medical errors have dire consequences because they cause poor patient outcomes and degrade quality of healthcare services that a healthcare institution offers. Therefore, EHR is central in the elimination of medical errors, which occur due to poor keeping of records.
Since EHR data is in digital form, it is very versatile in that one can easily store it in different forms, manipulate, and update it as required. According to Vest, Yoon, & Bossak (2012), healthcare professionals require analyzed data so that they can easily infer a meaning out of data and take appropriate action in providing effective healthcare service. EHR store crude data, but it has features that enable users to analyze the data and present it in a meaningful form.
Additionally, EHR is important in the billing system as it is accurate, fast, and transparent. Use of paper-based medical records in billing is complex because each department within a healthcare institution presents its own bill resulting into different bills charged upon the same patient. Collection and harmonizing these different bills and presenting them in the paper-based form entail a complex process that is prone to errors. Hayrinen, Saranto, and Nykanen (2008) commend that application of EHR in the analysis of financial records provides accurate billing data because electronic data is reliable, quick, and valid. Moreover, EHR eliminates duplication of bills, which is a common practice in paper-based billing system, thus increasing satisfaction among patients.
However, although EHR has significant importance to healthcare institutions, it has some disadvantages. One of the disadvantages is that it is expensive to put-up. Start up costs for EHR in a hospital or a clinic is about $400,000, which is too high. Many clinics or hospitals are unable to adopt application of EHR because it is very expansive when compared to paper-based medical recording, which only requires stationery.
According to a case study done in the United States, which examined the impact of computerization of the hospital system, the evidence indicated, “Hospital computerization has not, thus far, achieved savings on clinical or administrative cost” (Himmelstein, Wright, & Woolhandler, 2009, p.2). The case study found out that application of EHR has importance in improving the quality of healthcare and safety of patients, but does not have an overall impact of reducing administrative costs. Therefore, healthcare institutions must be ready to bear huge costs of starting up EHR.
Another disadvantage of adopting EHR in a healthcare institution is that it requires technical expertise, which needs training of healthcare staff on how to use it. EHR entails complex software that has numerous functionalities. The complexity of the software demands training and learning on the part of the staff; hence, it takes time to integrate its use fully in record keeping in a healthcare institution. Goodman et al. (2010) assert that vendors and users should have basic skills of using EHR systems because they “require significant education about how to install, configure, and use the products” (p.3).
Lack of proper education or training on the use of EHR will not enable healthcare institutions to realize its importance in record keeping. Therefore, for healthcare clinics to adopt EHR and integrate it into their system of record keeping, they must spend ample resources in training staff and wait for a long period to realize benefits of the system because it has considerable learning curve.
Issues about confidentially is another disadvantage associated with EHR. Paper-based medical records are more confidential than EHR, as they are hard to access. Comparatively, EHR exists in a digital form, which is versatile for anyone can access, transfer, and utilize data, in the absence of enough securities in place to guarantee confidentially. Confidentiality of EHR depends on securities that vendors of the system have put in place and ethics of healthcare staff (Goodman, et al., 2010).
If vendors of EHR have not designed a system that is secure enough to guarantee confidentiality of health records, it means that stored records would not be confidential. Moreover, if healthcare professionals do not adhere to ethical requirements of data keeping by divulging patients’ records, then securities put in place will not help. Hence, low confidentiality of medical records is a technical, as well as an ethical issue associated with EHR.
Since EHR is a new technological application in healthcare institutions, many countries have not embraced and adopted it in record keeping. A survey conducted on hospitals found in the Eastern Province of Saudi Arabia indicates that, out of 19 government owned hospitals, only 15 per cent of them have adopted and integrated EHR into their recording keeping (Bah, Alharthi, Mahalli, Jabali, Al-Qahtani, & Al-kahtani, 2011).
The survey indicates that healthcare professionals are resistant to the introduction of EHR because they do not have technological knowledge necessary to use the EHR systems. As government hospitals are grappling with challenges of adopting and integrating EHR into their record keeping, private clinics are experiencing extra challenges because they do not have enough resources and technology. There is a private clinic in Saudi Arabia that has over 500,000 patients and yet it is still using paper-based medical records. Therefore, the clinic needs to adopt EHR to overcome challenges of paper-based medical records and gain benefits of EHR.
Considerations for Choosing EHR
For the private clinic to adopt and integrate EHR in record keeping, it must consider the startup costs. EHR is very expensive, as it requires about $400,000, which can be too high for a private clinic to afford. A survey shows that only 3 out of 19 government hospitals in the Eastern Province of Saudi Arabia have adopted and Integrated EHR into record keeping (Bah, Alharthi, Mahalli, Jabali, Al-Qahtani, & Al-kahtani, 2011).
High cost of integrating EHR into hospitals is one of the reasons that have contributed to low use of the EHR system in Saudi Arabia. If a significant number of government hospitals cannot afford to buy EHR system and integrate it into their system, yet they have huge resources, it implies that private clinics, which have minimal resources, will find is challenging to raise startup costs. Moreover, given that the clinic is trying to reduce medical costs, introduction of EHR means that there will be a concomitant increase in cost of medical care.
The private clinic has been struggling to reduce medical costs to suit living standards of the population. Probably, adoption of EHR will reduce the number of patients attending the private clinic since the surrounding population is poor to afford any increase in medical care. Therefore, the impact of startup costs is a core attribute that calls for consideration before adopting and integrating EHR into the private clinic.
The number of patients, which the private clinic serves, is another core attribute that calls for consideration in the use of EHR. For EHR system to have any meaningful impact on record keeping, it requires a large number of patients. The private clinic in Saudi Arabia has about 500,000 patients, which is too high for paper-based records. Given the high number of patients, the private clinic generates a huge amount of clinical data, which validates the use of EHR.
Bisbal and Berry (2009) argue that paper-based medical recording involves keeping of records in separate clinical environments making it hard for clinicians to access and utilize. As the private clinic generates a huge amount of clinical data, application of EHR is necessary to alleviate cumbersome process of paper-based medical records.
Confidentiality of the medical records is an attribute that needs consideration in the adoption and integration of EHR in the clinic. Medical records contain sensitive information of individual patients; hence need maximum confidentiality possible to protect patients from undue discrimination or stigmatization associated with their conditions. The features and functionalities of the EHR must have enough securities to secure medical data within the clinic.
Ideally, the EHR should have securities that allow only clinicians or specific staff members to access given information, but not everybody. EHR with poor securities integrated into the system is prone to hacking and loss of pertinent information in the clinic, which does not only affect the image of the clinic, but also leads to infringement of privacy of the patients. In contrast, EHR with enough securities guarantee safety of clinical data and protects privacy of patients.
Goodman et al. (2010) state, “Safe and successful EHR systems further require ethics education, which has become a standard part of professional development in the corporate world” (p.3). Integrated securities and ethics of healthcare professionals are factors that determine confidentiality of medical records. Therefore, security integrated into EHR is a factor that determines the importance of EHR in record keeping.
Application of EHR in record keeping needs technical expertise, thus, availability of technical experts is a factor that calls for consideration. EHR is a complex system that one cannot operate unless s/he has enough technical skills. Without technical experts, it will be impossible for the clinic to gain full benefits of the EHR system. Moreover, utilization of the program without necessary skills will lead to poor data entry, which ultimately influences the quality of medical data stored. “The success of EHRs depends on the quality of the information available to health care professionals in making decisions about patient care, and in the communication between health care professionals during patient care” (Hayrinen, Saranto, & Nykanen, 2008, p. 300).
If poor quality of information is available and healthcare professionals are not able to utilize it because they do understand EHR, it means many medical errors will occur. Healthcare professionals at the private clinic only understand paper-based medical records; thus, introduction of EHR requires education and training of staff.
Efficiency and effectiveness of EHR in record keeping is a factor that needs consideration. The private clinic has used paper-based medical records for many years, and it has mastered its application. In paper-based recording, the private clinic has classified clinical data according to clinical departments and nature of data. Additionally, the staff members have developed a filing system to increase efficiency and accessibility of information that one requires.
Hence, EHR should have effectiveness and efficiency that is better than paper-based process of record keeping for the private clinic to improve its record keeping process. Himmelstein, Wright, and Woolhandler (2009) posit that EHR increases the effectiveness and efficiency of data management in healthcare institutions. Therefore, EHR does not only help healthcare clinicians to store and retrieve data, but it also helps administrators to overcome challenges of paper-based medical records.
Since the private clinic experiences problems of medical errors due to poor record keeping, EHR will provide a solution. The private clinic serves about half a million patients and paper-based medical records are unable to track medical history of each patient. In this view, poor storage and retrieval of wrong information about a given patient have contributed to the numerous medical errors experienced in the clinic.
Therefore, to eliminate or reduce medical errors that occur due to poor keeping of records or interpretation of records, the clinic should consider adopting and integrating EHR into its recording keeping. Poissant, Pereira, Tamblyn, and Kawasumi (2005) posit that EHR increases efficiency of documentation, which gives way to better quality of care and reduced medical errors, thus promoting safety of patients. Hence, given the importance of EHR system in improving the quality of care and reducing medical errors, the private clinic should adopt and integrate it into its system as a means of promoting healthcare services that it offers to about half a million of patients.
The adoption of EHR in the clinic should consider laws and regulations. Government regulations in some jurisdictions can be stringent to the extent that they do not allow the use of ERH, stipulate the model or dictates the manner of using it. In this case, the private clinic must consider how available laws and regulations dictate the application of EHR in healthcare institutions.
Furthermore, the private clinic must ascertain how Saudi Arabian government regulates EHR in private clinics so that it can comply with the conditions and prevent any legal ramifications. Given that EHR is a technical system, governments usually have a role to play in protecting healthcare institutions and patients from malfunctioning of the system. Goodman et al. (2010) state, “EHR should not contain language that prevents system users, including clinicians and others, from using their best judgment about what actions are necessary to protect patient safety” (p.2). Hence, the private clinic should buy EHR that meets the standards set by the government of Saudi Arabia for it to comply with the existing laws and regulations.
Ultimately, organizational culture of the private clinic needs consideration because it has overwhelming influence on the adoption and integration of the EHR system. Most of the healthcare professionals do not have skills of using information technology; hence, they are unable or unwilling to adopt the new system of EHR.
According to Bah, Alharthi, Mahalli, Jabali, Al-Qahtani, and Al-kahtani (2011), “some of the main challenges faced by the IT managers in implementing EHRs in their hospitals are related to the uncooperative attitudes of some physicians and nurses toward EHRs” (p.1). The uncooperative attitudes emanate from organizational culture that is accustomed to paper-based medical records and averse to adoption of technology. Hence, for successful adoption and integration of the EHR into the private clinic, there should be a change in organizational culture to favor technological advancement.
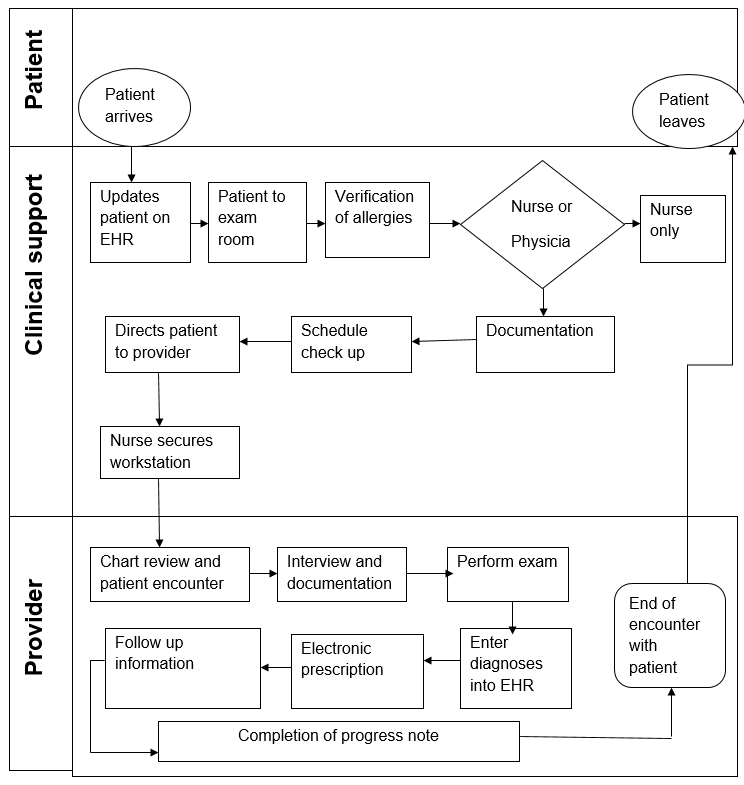
The EHR system for the clinic should have the above design to enhance efficiency and effectiveness of record keeping. The workflow design fits the clinic because it serves a large number of patients with diverse diseases. When a patient arrives, the nurse on duty updates details of the patient on EHR system before directing the patient to the exam room. The nurse clinically examines the patient and verifies if s/he has any allergies.
Depending on the condition of the patient, the nurse can direct the patient to another nurse or a physician. If the nurse can handle the situation, the patient receives essential services then leaves the hospital. If the nurse feels that the patient should see a physician, the patient follows necessary procedure towards meeting a physician. The nurse documents information about the patient, schedules check up with the physician, directs the patient to the provider, and then secures the station.
The provider then encounters the patient and reviews the chart before interviewing the patient and subsequently documenting the additional information about the patient. After that, the provider recommends for laboratory examination and diagnoses updated on the EHR system. Based on diagnoses, the provider makes necessary electronic transcription and directs the patient to the pharmacy. Moreover, the provider enters follow up information on the EHR system and allows the patient to leave the clinic.
EHR Readiness Assessment
To perform readiness assessment of the clinic, the study administered questionnaire, which it obtained from the website of a health agency of the United States, the Health Resources and Services Administration (HRSA). Based on the administered questionnaire, it is evident that the clinic is not ready to adopt and implement EHR because it has several impediments. The leadership of the clinic is not yet ready to embrace EHR, because it is not sure whether doctor’s office quality-information technology is essential in the clinic.
Although workflow evaluation of the clinic has issues in health maintenance tracking, poor legibility of medical records, medication prescribing, and handling of information, the leadership is not ready to involve the management in addressing operational inefficiencies in workflow.
The culture of the healthcare profession is averse to information technology because the clinic has not adopted any advanced system of information technology. Although the clinic has computers and Internet connectivity, the healthcare professionals use it to send mails and search for medical resources. The clinic has no electronic medical charts, e-transcription, and e-labs; hence, the members of staff are not literate in computer applications and information technology, except physicians who can access computers.
Additionally, the clinic has no enough recourses and information technology infrastructure because it has not networked its computers and has no database server. Therefore, the clinic is not ready to adopt and implement EHR because of deprived leadership, cultural resistance, and poor infrastructure of information technology.
Questionnaire
Doctor’s Office Quality-Information Technology (DOQ-IT)
Practice Readiness Assessment Form.
Preferred Method of Contact:
Telephone Fax E-mail
Project Interest Declaration (Please check all that apply)
I wish to apply to participate in the DOQ-IT project
Unsure, please contact me
No, I do not wish to participate, but do wish to be kept informed of developments
Does the Practice use a single tax ID number to bill Medicare? Yes No
Percentage of patients seen daily by the practice that are Medicare Fee-for-Service beneficiaries
40% Do Not Know
Medical specialties (Check all that apply):
Family Medicine Internal Medicine Geriatrics
Cardiology Endocrinology
Other(s) Please specify:
Patient Population
1. How many patients are seen in your practice on an average day? 0–20 patients > 20 patients
2. Of all your patients seen daily, what percentage has one or more chronic illnesses (i.e., CAD, diabetes, hypertension, heart failure or depression)? 30
Practice Workflow Evaluation
3. Please check the workflow issues that of the greatest concern in your office: (Check all that apply)
4. Of your patients seen daily, how many are seen without an available medical record?
5. Has the practice implemented any of the following workflow solutions? (Check all that apply)
Practice Management
6a. Does the practice have other projects either currently going on and/or starting soon that might affect the planning for and/or success of the EHR/HIT implementation project? (e.g., changing the telephone system)
Yes No
If ‘Yes’, please specify_____
6b. Has the practice tried to address workflow issues or operational inefficiencies in the past.
Yes No
If ‘Yes’, how successful were these efforts? Using a scale of 1 – 5 for your answer.
(1 = very unsuccessful, 3 = neither successful nor unsuccessful, 5 = very successful.)
1 2 3 4 5
7. What types of technology is the practice currently using on a regular basis? (Check all that apply)
E-mail (administrative use) E-mail (clinical use)
Disease registry E-prescribing
High-speed Internet connection Locally networked computers
Document imaging system E-Lab results
Please indicate whether the practice has or will have the following systems in place within 6 months:
7a. Practice management system
Please specify vendor/system: ________
7b. Electronic Medical Record (EMR) or Electronic Health Record (EHR) system
Please specify vendor/system:
Please specify if the system supports disease specific registries (yes/no):
7c. Other Information Technology (IT) system(s)
Please specify vendors/systems:
8. Do you currently create reports or use a registry (i.e. patient tracking system) to manage patients with chronic conditions (e.g., diabetes, cardiac, hypertension, preventive services)?
Yes No
8a. If yes, what do you do with the data? (Check all that apply)
9. Do you currently provide printed information on drug therapies, disease management, diet, etc.? Yes No
10. Does the practice provide interpreter services for non-English speaking patients? Yes No
11. Would the practice be interested in learning more about how it can provide more culturally responsive care?
Yes No
12. How many of the following do you have in your practice (all sites)?
Physicians 73 Non-Physician Clinicians __103
LPN/RN 196 __ Other Office staff __ 150
13. Do you conduct weekly or monthly staff meetings? (Clinicians & administrative staff) Yes No
13a. If yes, what are some of the discussion topics? (Check all that apply)
b. If yes, what is the frequency of the meetings?
Laboratory
14. Please estimate the proportion of total lab services generated in your practice that are processed;
14a. Do you collect blood specimens in your office Yes No
15. Thinking about how your practice receives lab reports, please estimate what percentage is received by each of following methods.
16. On average, about how many calls each week do you or your staff make to the lab about lab reports?
Prescriptions
17. On average, what is the number of new (non-refill) prescriptions does your practice write daily?
18. On average, how many refills or renewal requests does your practice process daily?
19. On average how many of your practice patients per day need their prescriptions rewritten?
20. On average, please estimate the number of follow-up calls or faxes your practice receives each week
for medication prescribing issues (illegible handwriting, drug- drug interactions, allergy alerts, non-formulary)
21a. Are you currently tracking groups of patients taking certain medications (e.g. patients on Warfarin).
Yes
No
b. If yes what is the method of tracking?
Spreadsheet Card file Database EMR PMS ICD 9 abstract
Clinical Referrals
22a. How many referrals to specialists do you make each week?
b. Does your practice have method for tracking referrals to specialists prior to the return of the consultation report? Yes No
Transcription Services
23a. Does your practice use transcription services. Yes No
b. If yes, what is your practice’s average transcription costs per month? $
Billing
24a. What is the practice’s current method of billing? (Check all that apply)
b. If you are billing electronically, is your system HIPAA compliant? Yes No
c. Does your current system allow you to generate reports sorted by CPT or ICD 9 Code? Yes No
25. What is your average turn around time on claims from submission to payment?
26. Do you have any problems with or concerns about your coding? Yes No
Information Technology.
27. Which of the following technologies would you be interested in, if you are not using them currently (Check all that apply)
28. Which staff members have direct access to a computer/terminal? (Check all that apply)
Physicians
Clinicians (e.g., NP, PA, RN)
Administrative staff
Other____
29a. What is the total number of computers currently in your practice? _____________
b. Are your computers connected to a network? Yes No
c. Do you share documents or information on your network? Yes No
d. Do you communicate within your practice using e-mail? Yes No
30. Does your practice have a high-speed Internet connection? Yes No
a. If yes, is the Internet connection used by the staff daily? Yes No
b. If yes, what are the primary uses for the Internet connection? (Check all that apply)
31. Is your current Practice Management System (PMS)/billing system capable of interfacing with an Electronic Health Record (EHR) system? Yes No Not sure
32. Are you interested in upgrading your current PMS? Yes No Not sure
33. Are you interested in an integrated solution? (Combining PMS & EHR) Yes No Not sure
34a. Has your practice explored any EHR systems? Yes No
b. If yes, how have you gone about it? (Check all that apply)
Read an article in peer reviewed journal
Attended Healthcare technology conference
Completed an online vendor return on investment
Talked to a colleague who uses EHR
Visited colleagues’ practice to see EHR
Read an article in trade / medical magazine(s)
Attended a vendor demonstration
Other
35. If you have not implemented an EHR system, what barriers are you facing? (Please prioritize the top three reasons from the list below)
Current EHR Users Only – Answer remaining questions
36. Who was involved in the decision to purchase an Electronic Health Record (EHR) system?
1 physician
All the physicians at the practice
Entire staff at the practice
Other___
37a. Were your partners and staff as eager to progress to EHR as you were.
Yes
No
b. What is the name of the EHR selected?
38. What are your goals (benefits) for using an EHR? (Please prioritize in order with “1” being the most important and “9” being the least important)
- Receive return on investment associated
- with software/hardware
- Increase Patient satisfaction
- Improve phone and fax processing
- Timely access to patient records
- Facilitate Management of chronic conditions
- Provide better follow up care to patients
- Other
- Reduce transcriptions costs
- Reduce paper based medical charts and filing charts
- Reduce administrative costs associated with practice
- Provide more services to patients per visit
- Capture all services provided at each visit
- Improved quality of life – Go home earlier
- Reduce Medical errors
Practice Contact Information
Lead Physician Contact
Administrative Contact
Other Contact
DOQ-IT Lead Physician Signature
Date 24/10/2012
Thank you for your interest, we will contact you upon receipt of the completed assessment. If you would like additional information or have any questions, please feel free to contact us at 516-326-7767 ext 445.
Sincerely,
DOQ-IT Team at IPRO
EHR Systems Used in Saudi Arabia
The common EHR systems that are in Saudi Arabia are WorldVistA EHR system, Universal EHR Solutions, and CureMD EHR. WorldVistA EHR system is free EHR software developed in the United States by Veteran Administration. The Veteran Administration provides WorldVistA EHR system as open-source software to encourage extensive adoption of EHR by physicians in various healthcare centers and since it is open-source software, it enjoys limited markets because commercial fashions dominate the market.
WorldVistA EHR system has core features such as “registration of patients, reminders for chronic diseases, clinical order entry, templates for progress notes and results reporting” (WorldVista, 2012). It has a modular structure with wide customization options given that it is open-source software. Customization options include the ability to interface with pre-existing systems and applications, scanning module, e-prescription, reporting capabilities, clinical reminders, and specialized templates for pediatrics and gynecology. Moreover, the WorldVistA EHR system is compatible to Linux-based servers, Mac OS-based servers, and windows based servers, hence promoting its wider use in various healthcare settings.
Universal EHR Solution is another EHR system that is common in Saudi Arabia. It is a sophisticated EHR system, yet it provides robust features that enable users to enter, store, and retrieve data quite easily. The Universal EHR Solution has features that enhance automation of most tasks in a healthcare center, which include laboratory results, e-prescription, incorporation of charts and other imaging modalities, maximizing coding and billing, management therapy, statistical analysis, conveying diagnoses, and generating professional documents.
In addition to these features, physicians can customize the Universal EHR solution to provide handwriting recognition, digital ink, voice recognition, scanning, and printing. Additionally, the Universal EHR solution allows physicians to have real-time contact and access to patient records thus can respond to emergency immediately. Since healthcare centers have different needs, “the Universal EHR solution exists in three versions, viz. Physician’s Solution Lite, Physician’s Solution Specialty Module, and Physician’s Solution Fully Customized” (Universal EHR Solutions, 2011).
In this case, “Physician’s Solution Lite is simple and is the most affordable EHR system because it has few customized features and limited advanced features, while Physician’s Solution Specialty Module has special features and precoded templates, which minimize its application” Universal EHR Solutions, 2011). However, Physician’s Solution Fully Customized provides all advanced features and unlimited software customization, hence allowing the healthcare users to gain full benefits of EHR system.
CureMD EHR is an efficient and fully integrated EHR system that is cost-effective. It has important features such as electronic labs, drug and allergy alerts, care guides, chart management, lab management, clinical charting, handwriting transcription, electronic billing, image management, automatic refill requests, and disease management amongst other features that are user friendly. It contains customizable features such as appointment scheduling, billing records, electronic patient statements, inter-office messaging, allows multiple users, and electronic claims.
Since medical records contain sensitive and pertinent information, CureMD EHR has security features such as automatic backup, emergency access, encrypted data transfer, user authentication, recovery protection, user identifications, and automatic logoff. The CureMD EHR is a complex EHR system and thus requires extensive training of healthcare professionals on how to use it. The CureMD EHR meets the requirements by the Certification Commission for Health Information Technology (CCHIT) criteria in terms of hypertension management, vaccination, cancer screening, weight control, and preventive care. It also meets ambulatory criteria as it supports clinical decision-making, electronic prescribing, inpatient criteria, patient reminders, clinical summaries, and demographic records.
Comparisons and Contrasts
Comparatively, the three EHR systems viz. WorldVistA EHR system, Universal EHR Solutions, and CureMD HER, which are common in Saudi Arabia, are similar in their basic functionalities and features as they serve same functions in a healthcare center. The three systems have patient registration, automation of lab results, electronic prescription, clinical charting and alerts, scanning, and printing.
Moreover, the three systems provide customization of features based on their uses in a healthcare center. For instance, the systems allow integration into pre-existing systems and applications, thus enhancing their compatibility to various healthcare centers. Automation of data entry and charting are other common features that one can customize when using the systems. Hence, a healthcare center has the freedom to customize the three systems to suit its needs and functions.
Contrastingly, the three systems differ in their features and functionalities. CureMD EHR is a complex system with a wide range of features and functionalities when compared with the other two EHR systems. The CureMD EHR has advanced features such as real-time access to medical records by physicians, emergency alerts, electronic patient statements, and essential securities that to protect the loss of data, and unauthorized access.
In contrast, WorldVistA EHR system is an average EHR system in its complexity with essential features and functionalities that suit any form of healthcare institution. It allows customization according to departments, for example, gynecological and pediatric sections. On the other hand, complexity of the Universal EHR depends on the version, because it is composed of three versions. The difference that exists among the three EHR systems is that while WorldVistA EHR system is open-source software, CureMD and the Universal EHR Solutions are available in the markets.
While CureMD EHR and WorldVistA EHR systems exist as a single version, the Universal EHR Solution exists in three versions that have different features, thus providing healthcare centers with different systems. Clinics and small healthcare centers can adopt Physician’s Solution Lite version because “it is not only simple, but also the most affordable EHR system having few customized features and limited advanced features” (Universal EHR Solutions, 2011).
A bit advanced version is Physician’s Solution Specialty Module, which has special features and precoded templates, hence minimizing its application in medical recording. The most advanced version of the two is the Physician’s Solution Fully Customized, because “it offers all advanced features and unlimited software customization” (Universal EHR Solutions, 2011). It has many functionalities and features that a large healthcare center can utilize in both basic and customized applications.
Considering the needs of the private clinic in Saudi Arabia, the best EHR system that suits the needs is the WorldVistA EHR system. Since EHR system is very expensive and the private clinic cannot afford complex system such as the CureMD EHR, the WorldVistA EHR system becomes the best of the systems because it is open-source software with essential features. The WorldVistA EHR system can satisfy the needs of the clinic for it is cheap, simple to operate, and secure. Moreover, the system allows automation of diagnoses, drug and allergy alerts, and provides electronic transcription.
The WorldVistA EHR system is also suitable because it is the most compatible software among the systems because it is compatible to Windows, Linux, and Mac based operating systems. Moreover, the WorldVistA EHR system complies with government regulations and has certification by CCHIT, thus making it valid and reliable software that can enhance efficiency of medical recording in the private clinic, and ultimately promotes quality of care and patient safety.
The Chart
References
Bah, S., Alharthi, H., Mahalli, A., Jabali, A., Al-Qahtani, M., & Al-kahtani, N. (2011). Annual survey on the level and extent of usage of electronic health records in government-related hospitals in eastern province, Saudi Arabia. Perspectives in Health Information Management, 2(1), 1-18.
Bisbal, J., & Berry, D. (2009). An analysis framework for electronic health record system. Methods of Information in Medicine, 48(6), 1-10.
Goodman, K., Berber, E., Dente, M., Kaplan, B., Koppel, R., Rucker, D., Sands, D., & Wilkelstein, P. (2010). Challenges in ethics, safety, best practices, and oversight regarding HIT vendors, their customers, and patients: a report of an AMIA special task force. Journal of the American Medical Informatics Association, 10(1), 1-5.
Hayrinen, K., Saranto, K., & Nykanen, P. (2008). Definition, structure, content, use, and impacts of electronic health records: A review of the research literature. International Journal of Medical Informatics, 77(5), 291-304.
Himmelstein, D., Wright, A., & Woolhandler, S. (2009). Hospital computing and the costs and quality of care: A case study. The American Journal of Medicine, 20(10), 1-7.
Poissant, L., Pereira, J., Tamblyn, R., Kawasumi, Y. (2005). The impact of electronic health records on time efficiency of physicians and nurses: A systemic review. Journal of the American Medical Informatics Association, 12(5), 505-516.
Universal EHR Solutions. (2011). Physician’s Solution. Web.
Vest, J., Yoon, J., & Bossak, B. (2012). Changes to the electronic health records market in light of health information technology certification and meaningful use. Journal of American Medical Informatics Association, 1(12), 1-7.
WorldVista. (2012). VistA software (FOIA) features. Web.